Report on the Survey of 2017 Nephrology Fellows
Lifestyle Concerns in Training and Practice are Key to Fellows and May Be Discouraging Applicants to Nephrology
Leo Quigley, MPH
Edward Salsberg, MPA, FAAN
Nicholas Mehfoud, MS
George Washington University Health Workforce Institute and School of Nursing
Ashté Collins, MD
George Washington University School of Medicine
Preface
Physicians in training represent the future practitioners in their field and provide a picture of the future supply. The experience of those completing their training and about to embark on their careers is also an indicator of physician demand in their specialty. For these reasons, the George Washington University Health Workforce Institute (GW-HWI) research team and the American Society of Nephrology (ASN) have conducted an annual online survey of current nephrology fellows and trainees beginning in 2014 to obtain data on demographic and educational background, educational debt, career plans, job search experiences, and factors influencing job opportunities and choices.
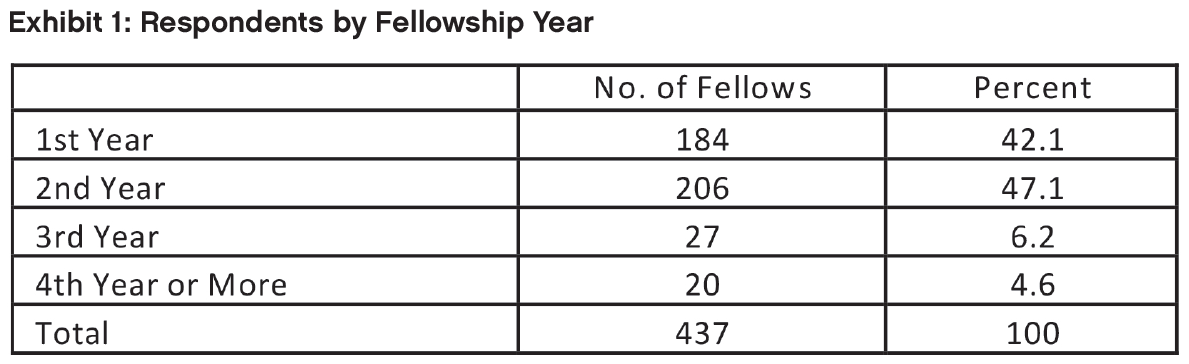
In 2017, the survey tool—adapted from the University at Albany Center for Health Workforce Studies (CHWS) annual NY State Resident Exit Survey and slightly modified from 2014, 2015 and 2016—was distributed to 1451 ASN Fellow/Trainee members (to whom ASN offers free membership) in May and June 2017. Four hundred and thirty-seven (437) fellows or trainees provided informed consent and responded to the survey questions for an overall response rate of 30.1% (this analysis excludes pediatric nephrology fellows unless otherwise stated). Among the assumed 863 fellows in their first and second year of Accreditation Council for Graduate Medical Education (ACGME)–accredited training programs, we received responses from 390 fellows (45.2% response rate). (2017 ACGME data was not available at the time this report was written; comparisons are made with 2016 ACGME data instead.) The response rate for second-year fellows was 48.0% (206 of 429) providing a good picture of the job market faced by new nephrologists. (The basic nephrology fellowship is 2 years, but many stay on for an additional year(s) for subspecialty training or research.)
This report presents demographic information for respondents in all years of fellowship and training, as well as job market experiences and fellows’ plans for those completing their second year of fellowship or beyond. It also presents data on job offers accepted by nephrology fellows and their assessments of the overall state of the specialty and job market. For all of the statistical tests presented, we considered probability values <0.05 to be statistically significant.
Key Findings
Overview
Three overarching themes emerge from the 2017 survey and analysis of the trends over the past 4 years: the job market for new nephrologists improved in 2017 for US medical graduates (USMGs) and international medical graduates (IMGs); the job market for USMGs was significantly better than for IMGs, who represent a majority of the trainees; and lifestyle concerns, both in terms of training and practice, are important to fellows and may be discouraging applicants to the specialty.
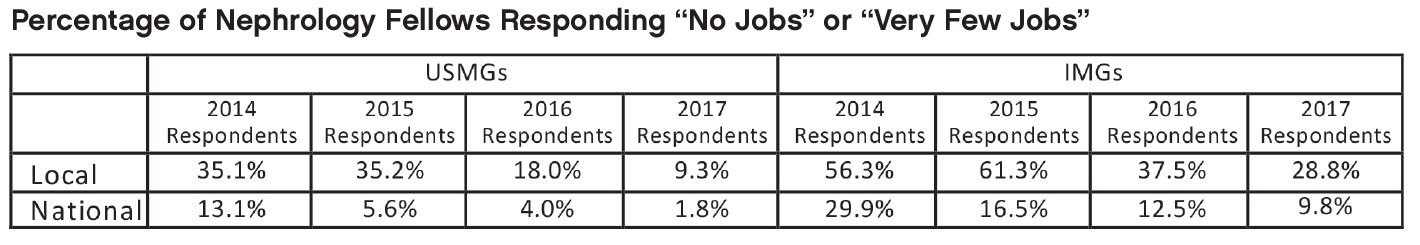
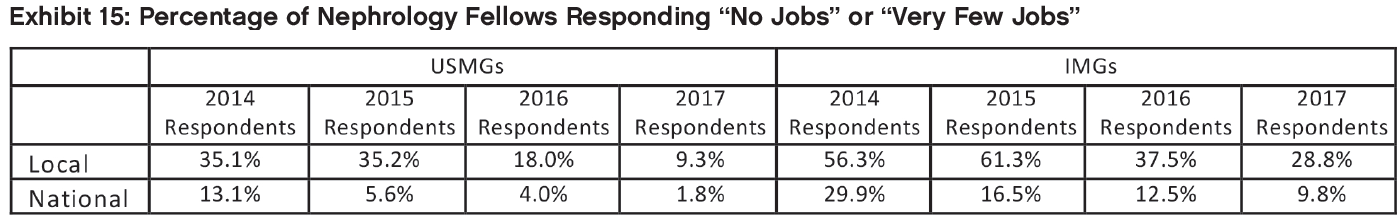
An Improving Job Market with Continued Challenges for IMGs
Among nephrology fellows who had searched for a job, perceptions of local nephrology job opportunities were much improved compared to earlier years for both USMGs and IMGs. The percent of USMGs who indicated “no jobs” or “very few jobs” in the national job market dropped from 13.1% in 2014 to 1.8% in 2017, and from 35.1% to 9.3% for the local job market.
While the view of the market was far more negative than for USMGs, the improvement for IMGs was also impressive with the percentage responding “no jobs” or “very few jobs” dropping from 29.9% in 2014 to 9.8% in 2017 for the national job market, and from 56.3% to 28.8% for the local job market.
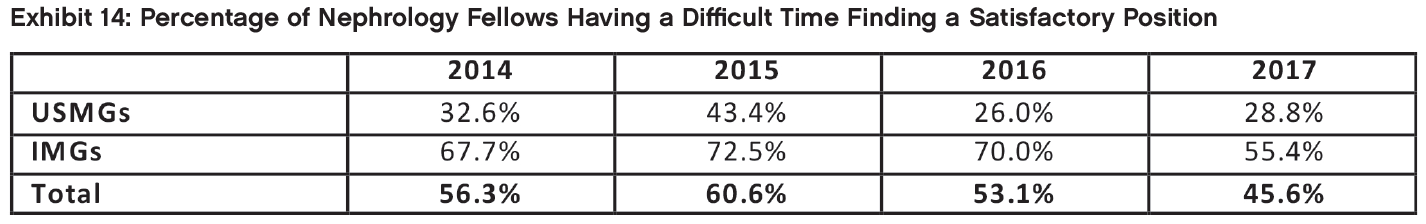
Fewer than half of respondents (45.6%) who had searched for jobs reported having difficulty finding a satisfactory position compared to 53.1% in 2016. There was a statistically significant difference between IMG and USMG fellows’ reports of difficulty finding a position: 55.4% of IMGs reported having difficulty finding a position they were satisfied with, a substantial improvement over the 70.0% of 2016. For USMGs, 28.8% reported having difficulty compared to 26% in 2016.
Overall, the percentage of respondents indicating that they had changed their plans because of limited nephrology job opportunities continued its decline, from 42.9% in 2015 to 35.4% in 2016 and 32.7% in 2017. While both USMGs and IMGs were less likely to report changing their plans in 2017 due to limited job opportunities than in prior years, their likelihood of changing plans was significantly different: only 13.6% of USMGs reported that they had to change plans, while 44% of IMGs reported changing plans (p<0.001). This difference likely reflects more limited job opportunities that meet visa requirements allowing IMGs to practice in the US.
Fellows’ anticipated salaries in 2017 were higher than in previous years; the median anticipated salary for all demographic groups (by IMG status and sex) was between $180,000 and $189,999, with a mean anticipated salary of $187,000.
There was a statistically significant difference in satisfaction with salary and compensation between IMGs and USMGs. USMGs were slightly more likely to report being “Very satisfied” with their salary and compensation (22.9% vs. 18.5%).
When asked to identify the incentives they had received for accepting their primary job offers, respondents were most likely to report receiving the following:
Support for maintenance of certification (MOC) and continuing medical education (CME) (42.3%)
Income guarantees (41.4%)
Career development opportunities (34.2%)
Relocation allowances (29.7%)
Sign-on bonus (22.5%)
Lifestyle Concerns
Responses to a number of questions indicated the importance of lifestyle factors to fellows, both during training and for practice after training.
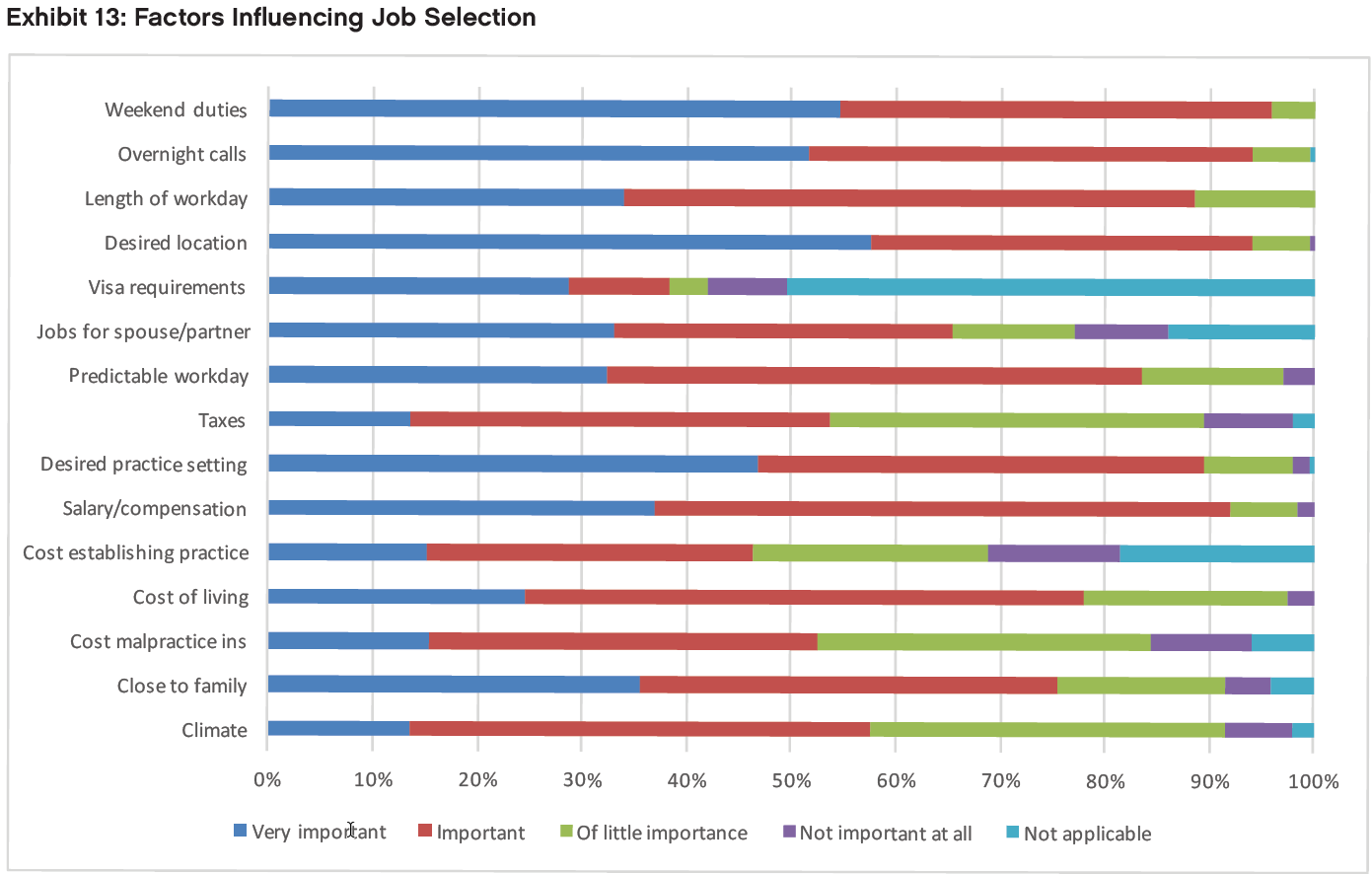
Respondents in their second year of fellowship or beyond rated the following factors as “very important” or “important” in their job selection:
Frequency of weekend duties (96.3%)
Frequency of overnight calls (94.0%)
Job/practice in desired location (94.0%)
Salary/compensation (92.0%)
Job/practice in desired practice setting (89.4%)
Length of each workday (88.5%)
This may reflect the nature of much of nephrology practice today and may be of concern to both nephrology fellows and residents who do not select the specialty.
- Fellows who would not recommend nephrology to medical students and residents cited the heavy workload, low compensation, difficult schedule, undervaluing of the specialty by other specialties, and lack of opportunities that support visas for IMGs as reasons for their negative assessments. This was consistent with the 2015 and 2016 responses.
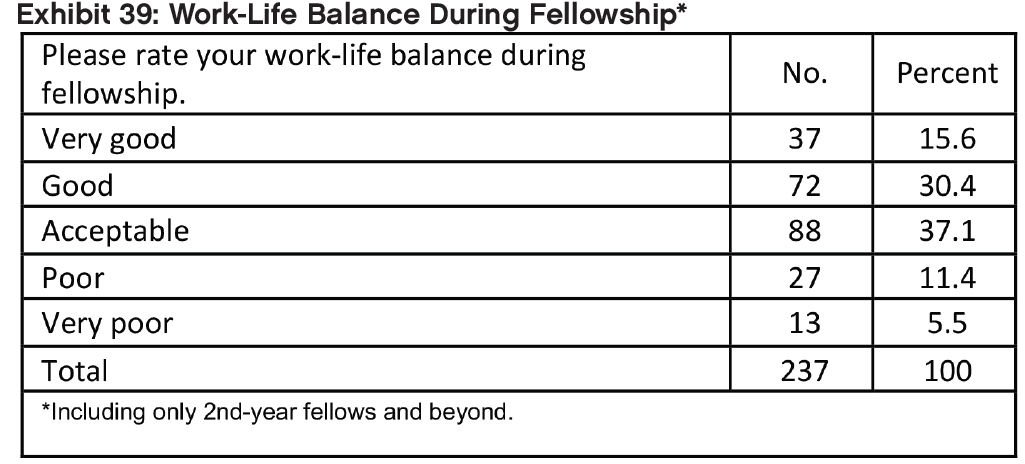
The survey included a specific question: “Please rate your work-life balance during your fellowship.” The responses were:
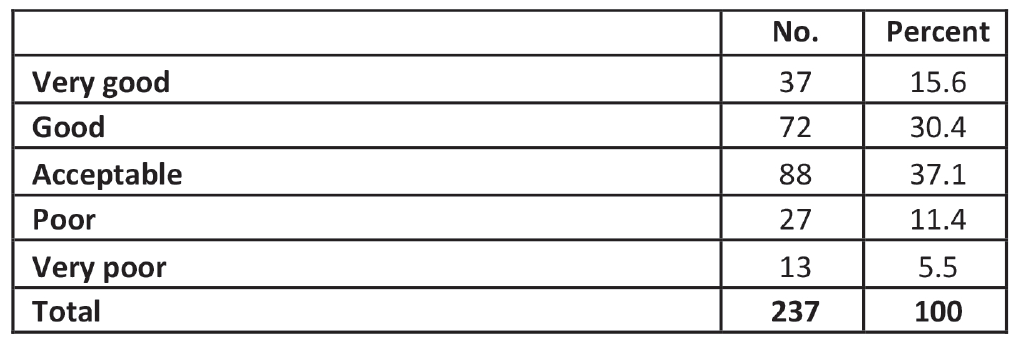
Only a minority of respondents (46.0%) in their second year and beyond felt their work-life balance during fellowship had been good or very good. About 1 in 6 rated their work-life balance as being poor or very poor.
Other Findings
Recommending the Specialty
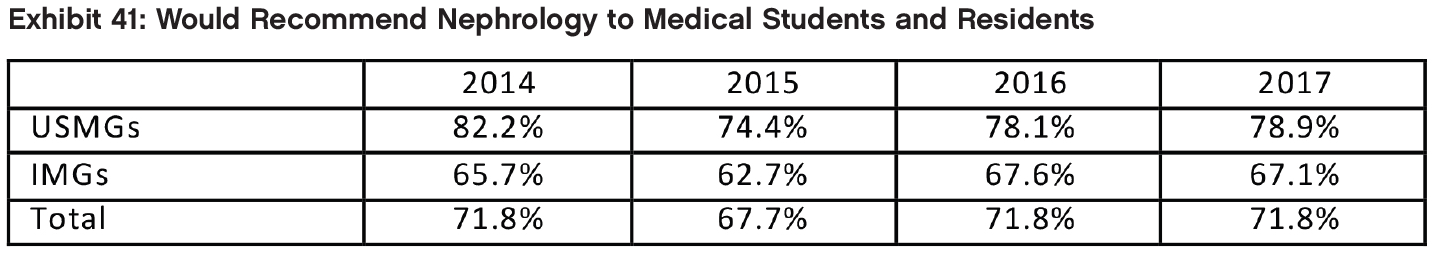
- Despite their mixed assessments of the nephrology job market, a majority (71.8%) of fellows indicated they would recommend nephrology to current medical students and residents, the same as in 2016. However, IMGs were significantly less likely than USMGs to report that they would recommend the specialty to others (67.1% vs. 78.9% respectively).
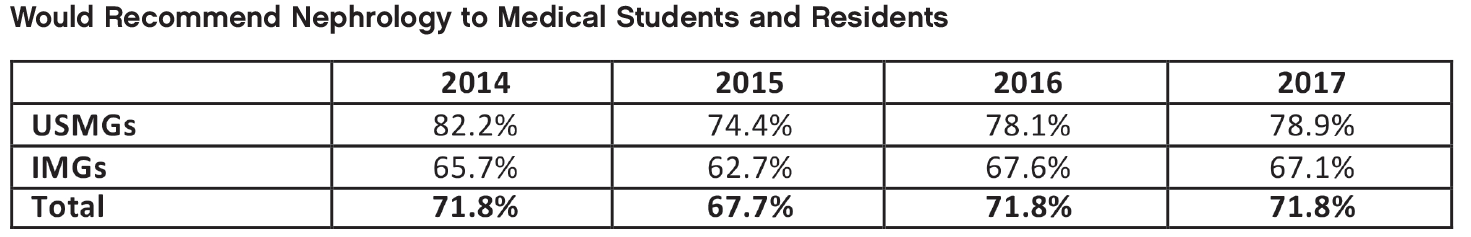
- Fellows who said they would recommend nephrology to medical students and residents cited many of the same factors mentioned by 2015 and 2016 respondents as reasons for their positive assessments: the intellectual challenge/interest of the field, variety of activities, and long-term patient relationships.
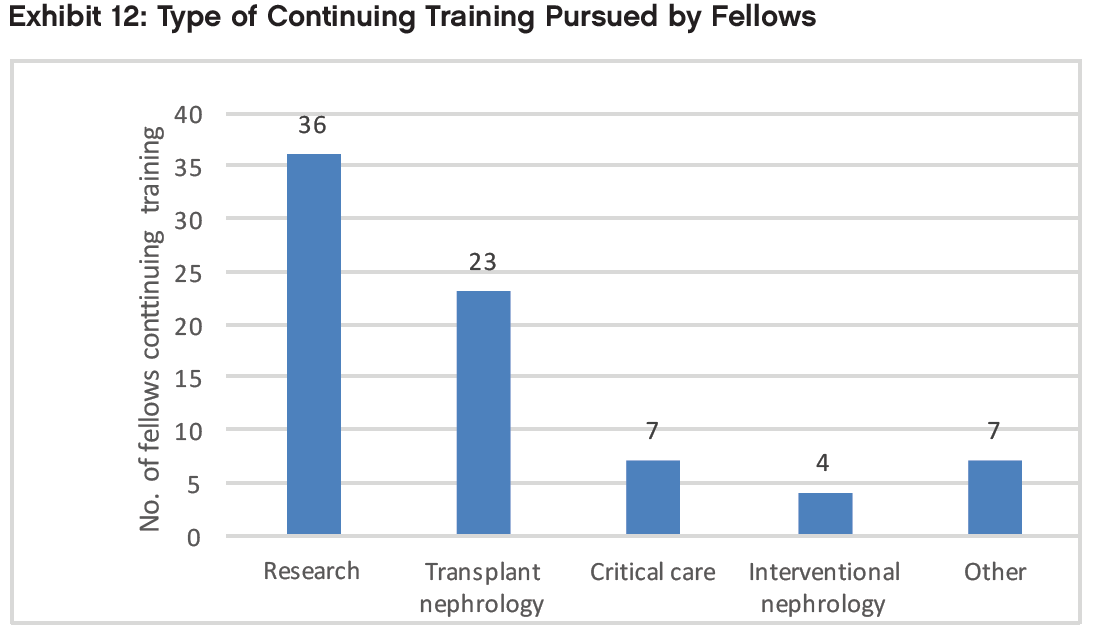
Practice Setting
Among respondents in their second year of fellowship or beyond who indicated their plans for the upcoming year, the largest proportion indicated that they planned to enter clinical nephrology practice (54.4%). Thirty-one percent (31%) intended to continue in their current fellowships or pursue additional subspecialty training. Frequently reported areas of continuing training included research, transplant nephrology and critical care.
Among respondents who had already accepted job offers, the largest group (43.1%) reported that they planned to work in nephrology group practices. Another 23.3% reported that they planned to work in academic nephrology practices, 11.2% said they planned to work in hospitals, and another 11.2% in 2-physician partnerships. Other settings included multispecialty group practices (5.2%) and multispecialty academic practices (3.4%).
Practice in Underserved Areas
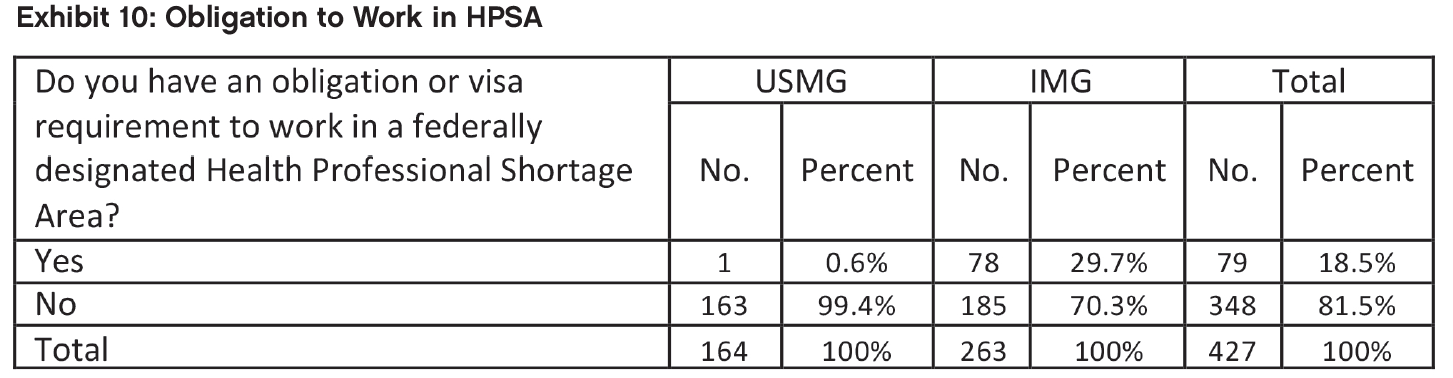
- As in previous years, IMGs appear to be making an important contribution to care in underserved areas. While 78 IMGs (29.7%) indicated an obligation to work in a federally designated Health Professional Shortage Area (HPSA), only 1 (0.6%) USMG did! The difference in the distribution of HPSA service obligations by IMG status was highly significant with a large effect size (0.791). (Effect sizes are typically classified as 0.2=low, 0.5=medium, 0.8=large; the measure of effect size used throughout is Cohen’s d.)
The Job Market
When asked an open-ended question regarding the types of jobs they perceived to be more and less available, newly graduating fellows mentioned several types of jobs that were more easily available according to their experience:
Jobs in remote, rural, or undesirable areas (e.g., Midwest, South), especially with large dialysis providers
Private practice jobs
Jobs in solo or small practices/hospitals/ communities
They reported several types of jobs that were less easily available:
Academic jobs
Jobs in metro areas or other preferred geographic areas (e.g., Florida, California, Pacific Northwest)
Jobs that meet visa requirements for IMGs
Compensation
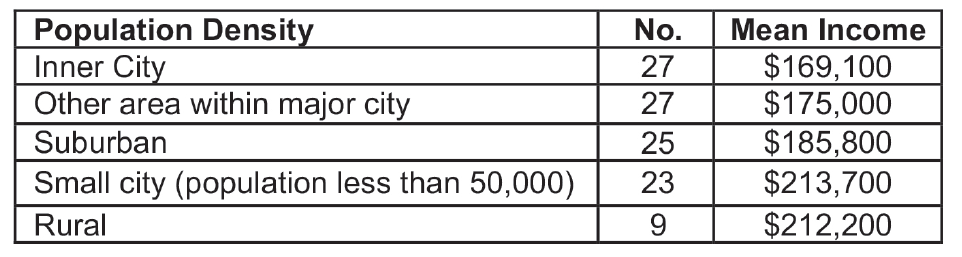
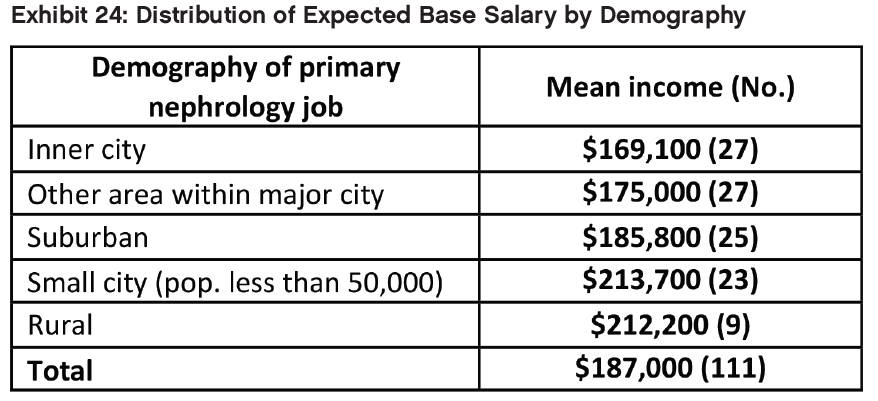
- There was a statistically significant difference in income by population density of the geographical area of practice, with the highest average incomes in small cities ($213,700) and rural areas ($212,200), and lower incomes in suburban ($185,800), large city areas other than inner city ($175,000), and inner-city areas ($169,100). It appears that small cities and rural communities need to offer nephrologists considerable more compensation than they can get in larger cities and suburban areas in order to recruit them.
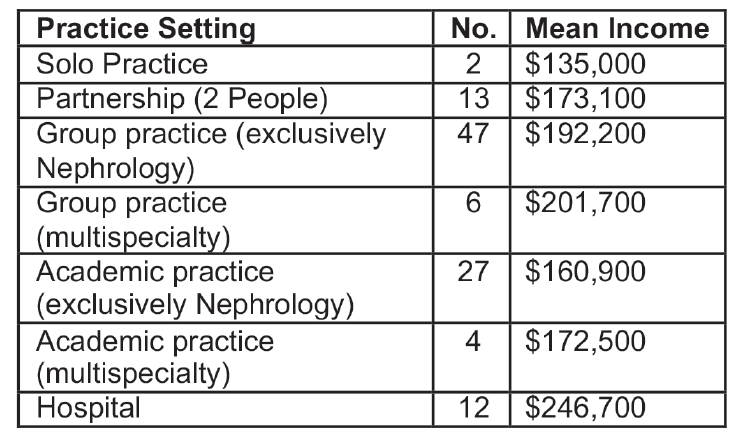
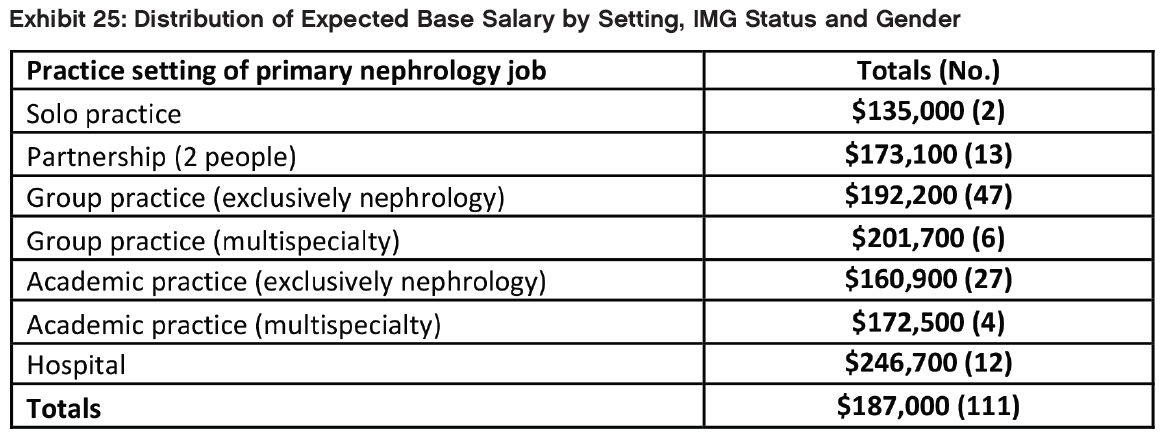
- As in 2016, there was a statistically significant difference between mean anticipated incomes between different practice settings.
Job Responsibilities
- The vast majority of respondents cited outpatient nephrology care and hospital care among their primary job responsibilities (93.2% for both). Other responsibilities listed included temporary dialysis catheter placement (29.1%), kidney biopsy (24.8%), medical directorship with a dialysis provider (22.2%), and clinical research (20.5%).
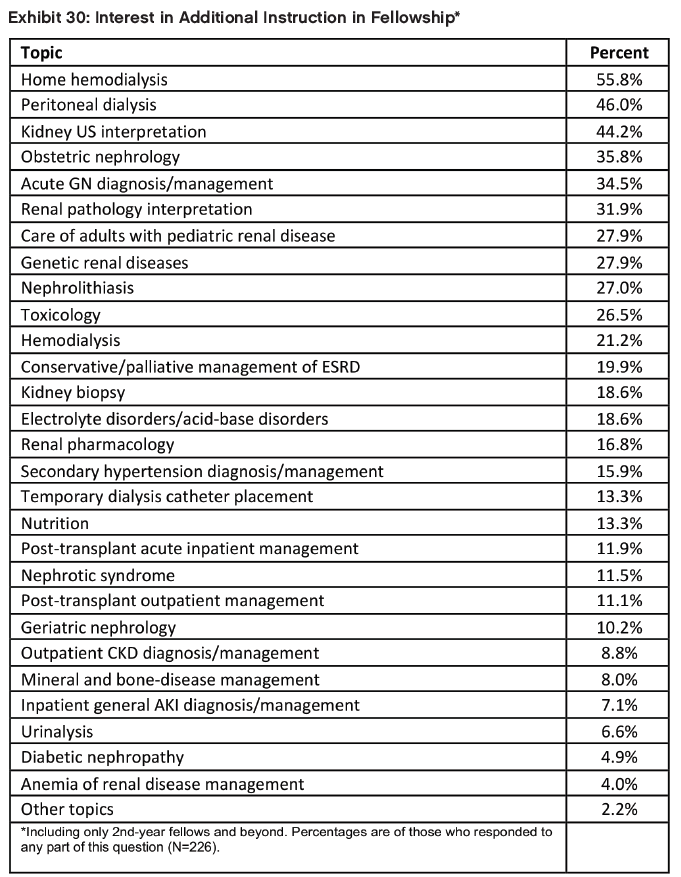
Content of Fellowship Training
- When asked about fellowship topics they would most like to receive additional instruction in during fellowship the highest response rates were for home hemodialysis (55.8%), peritoneal dialysis (46.0%), kidney ultrasound interpretation (44.2%), obstetric nephrology (35.8%), and acute glomerulonephritis diagnosis/management (34.5%).
Selecting Nephrology
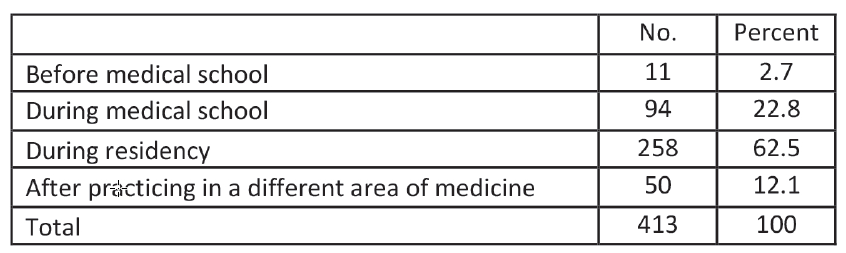
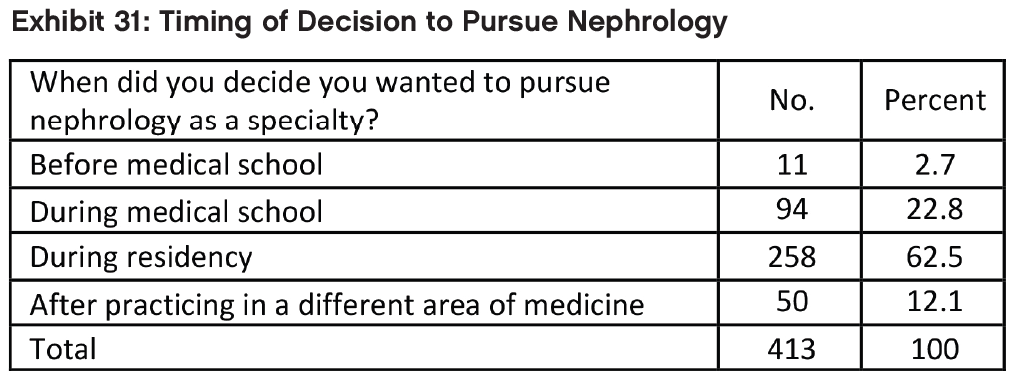
- The survey asked: When did you decide you wanted to pursue nephrology as a specialty? As indicated, a majority decided during residency.
Overview of Respondents
The 437 respondents to the 2017 Nephrology Fellows Survey included fellows in their first and second year of their ACGME training program, as well as third-, fourth-, and fifth-year fellows in subspecialty training or research positions. Of the 437 respondents, 253 had completed at least 2 years of nephrology training; 161 had searched for a job; and 119 had accepted a job offer. Different sections of this report present findings on each of these groups of fellows. (The totals in each data table vary depending on the number of respondents who answered the particular question or questions being shown.)
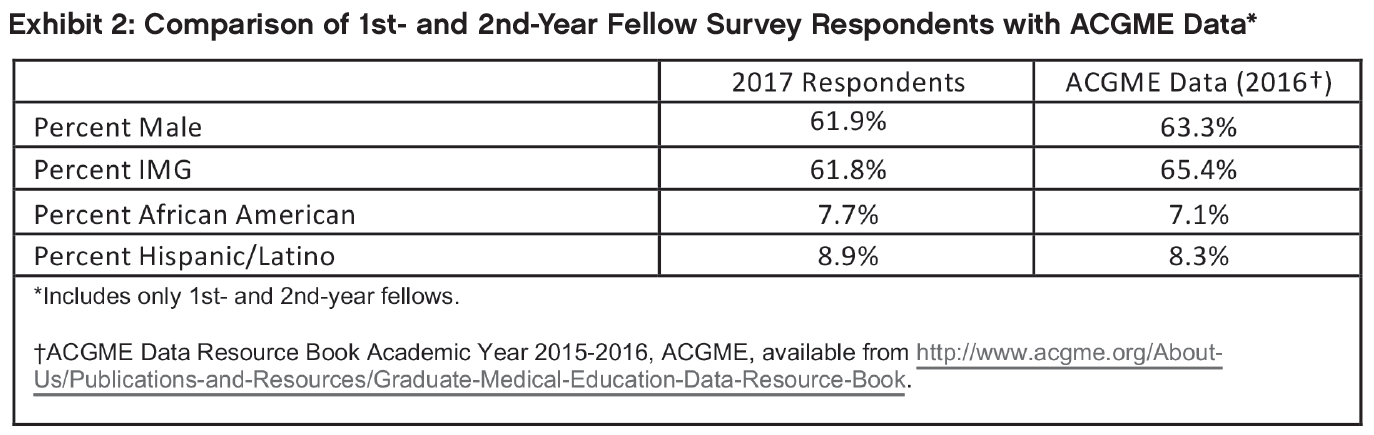
To assess the representativeness of the survey sample, we compared several demographic and educational characteristics of the 390 survey respondents in their first and second years of training to ACGME data on all 863 firstand second year- fellows (we used 2016 data as the 2017 ACGME data has not been published at the time of writing this report). Respondents in 2017 had very similar characteristics to the 2016 ACGME first- and second-year nephrology fellows, although the survey sample included slightly fewer IMGs and males and slightly more African American and Hispanic/Latino respondents. The percentage of African American survey respondents in their first and second years of training was almost the same in 2017 as in 2016 —7.7% vs. 7.9%; the percentage of Hispanic/Latino survey respondents was lower than in 2016 (8.9% compared to 9.8%).
Education, Citizenship Status, and Demographics of Respondents
This section presents data on the educational background, citizenship status, and demographics of all respondents to the 2017 Nephrology Fellow Survey.
Practice in Underserved Areas
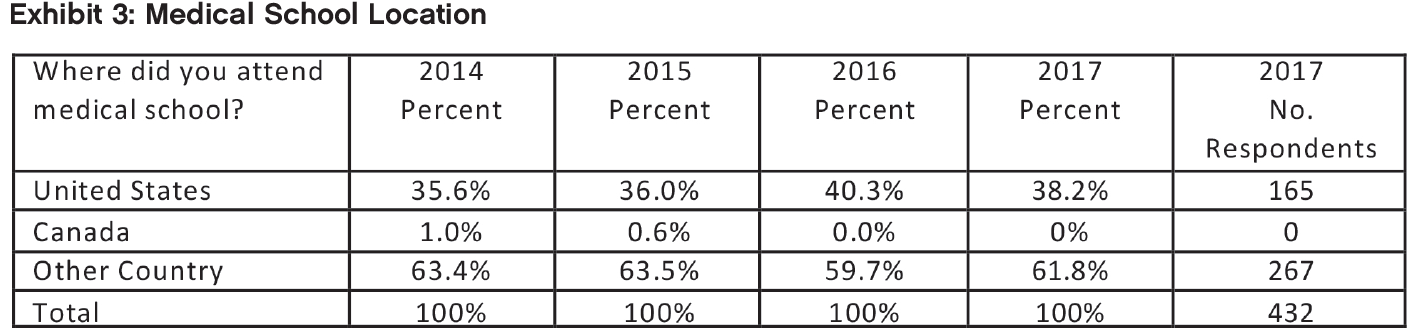
As in previous years, most 2017 survey respondents (61.8%) attended medical school outside the United States. IMG respondents reported attending medical school in 56 different countries, the most frequently cited of which were India (81 respondents); Pakistan (20 respondents); Dominica (16 respondents); Mexico and Nigeria (9 respondents each); China (7 respondents); Grenada, Dominican Republic and Syria (6 respondents each); and Egypt, Iraq and Lebanon (5 respondents each).
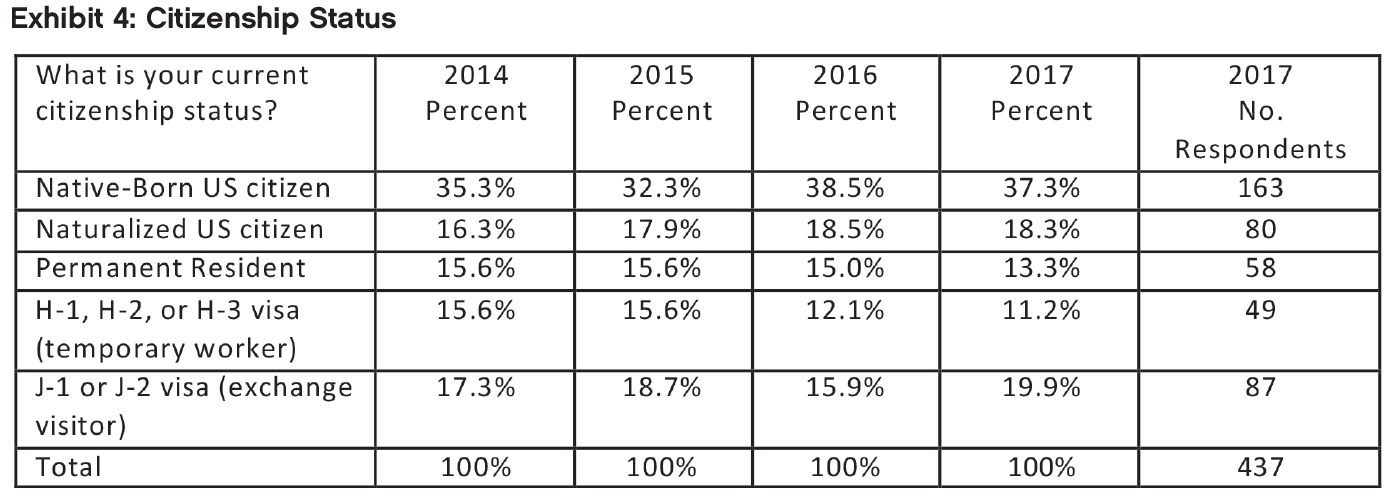
The distribution of 2017 survey respondents’ citizenship status was also similar to that of previous years’ respondents. More than half of 2017 respondents (55.6%) reported that they were US citizens, either native born or naturalized, and 13.3% reported that they were permanent residents of the United States. About 31% of the respondents were noncitizen holders of either H or J visas (a slightly higher percentage than in earlier years).
As in previous years, we identified a number of respondents who could be considered US IMGs, that is, US citizens who received their medical education outside the US. The proportion in 2017 was greater than previous years with 37 respondents (13.9% of all IMGs who indicated their citizenship status) in 2017 indicating that they were native-born US citizens who had received their medical education in another country, compared to 8.1% in 2016.
Sex
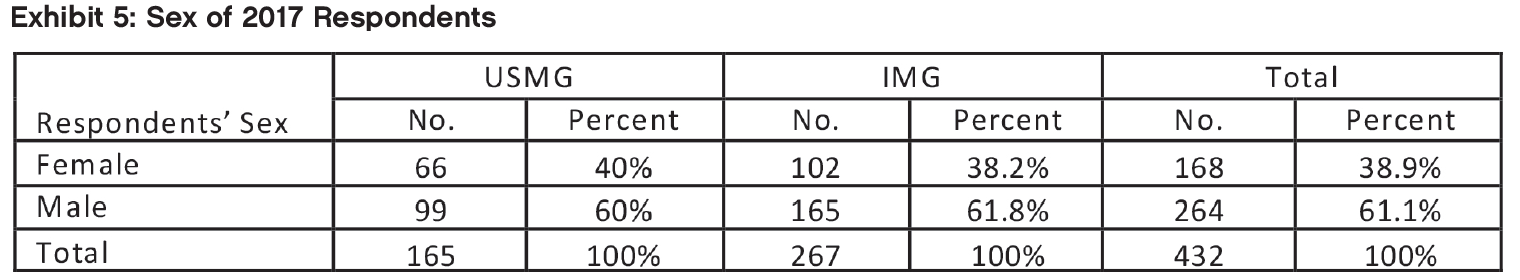
As in 2014, 2015 and 2016, the majority of 2017 survey respondents (61.1%) were male—a smaller percentage than in 2016 (64.3%). As in 2016, the difference in gender balance between IMGs (61.8% male) and USMGs (60% male) was not statistically significant, unlike in 2015 when IMGs were significantly more likely to be male than USMGs.
Age
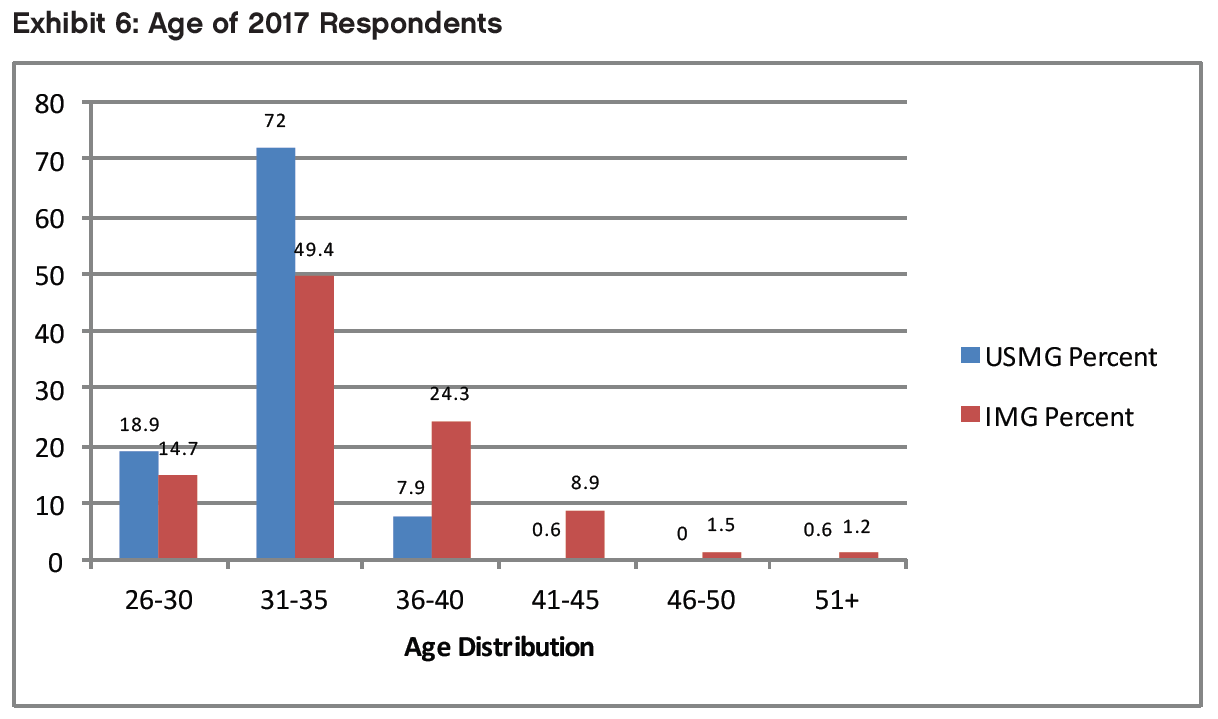
Respondents ranged in age from 27 to 54 years old. As in 2015 and 2016, the largest age group was 31 to 35 years, which included more than one-half of respondents. Also, as in 2015, IMG respondents were significantly older on average than USMG respondents on average (34.8 years vs. 32.3 years—p<0.01).
Race/Ethnicity
When asked to identify their race, the largest group of respondents identified themselves as Asian (40.7%), and the next largest group (34.5% of respondents) identified themselves as white. The distribution of race/ethnicity was significantly different across IMG categories: IMGs were significantly more likely to report being Asian (p<0.05) or of “other” race (p<0.01) than USMGs, and USMGs were significantly more likely to report being white than IMGs (p<0.01). The proportions of respondents who reported that they were black were not significantly different between the USMG and IMG groups.
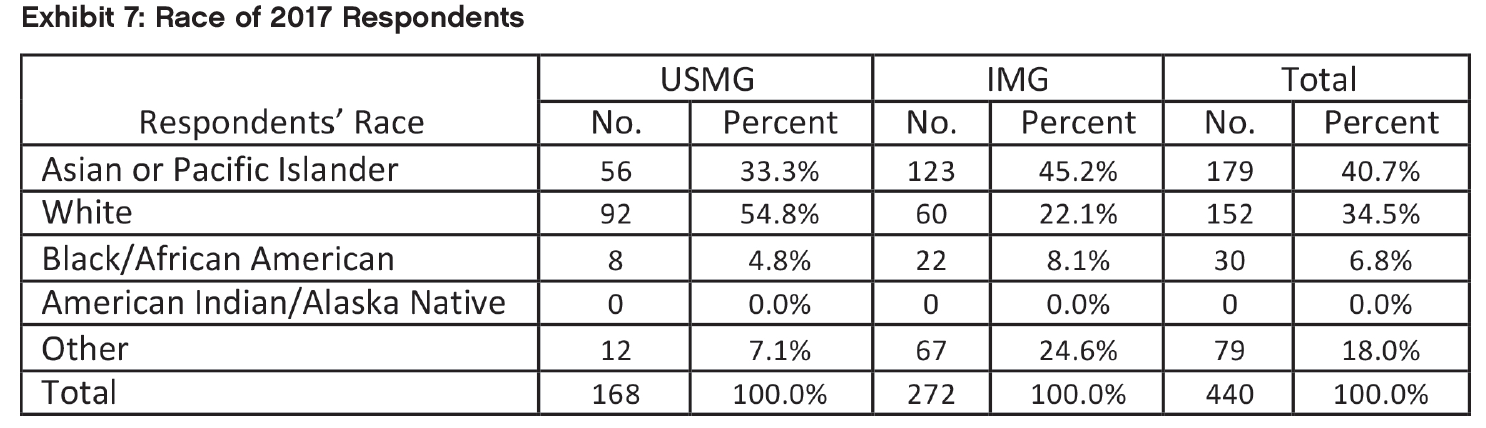
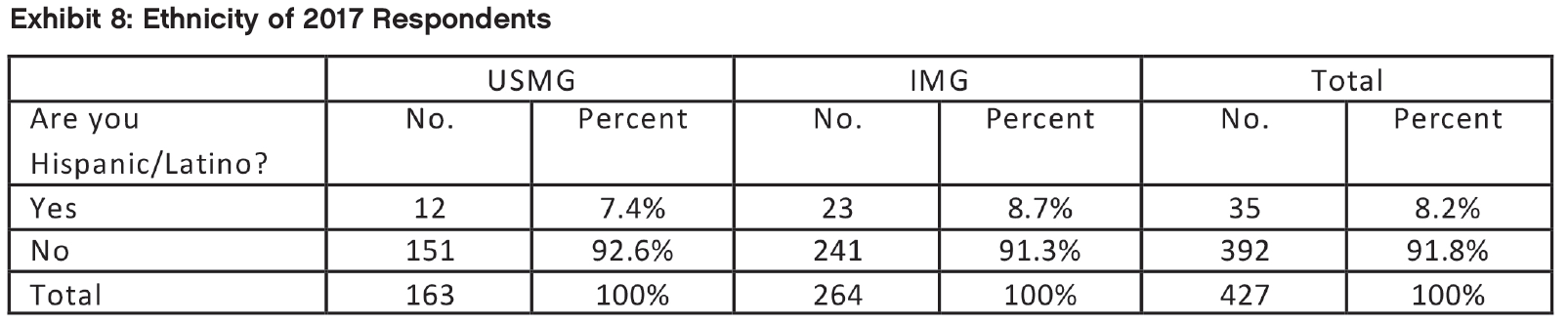
8.2% of respondents identified themselves as Hispanic or Latino, less than the 10.7% of 2016. This is almost equal to the 8.3% of ACGME nephrology residents and fellows who are Hispanic/Latino (ACGME, Annual Resource Data Book, 2015-16). IMG respondents were more likely to identify themselves as Hispanic or Latino than USMG respondents, but the difference was not statistically significant (p=0.621).
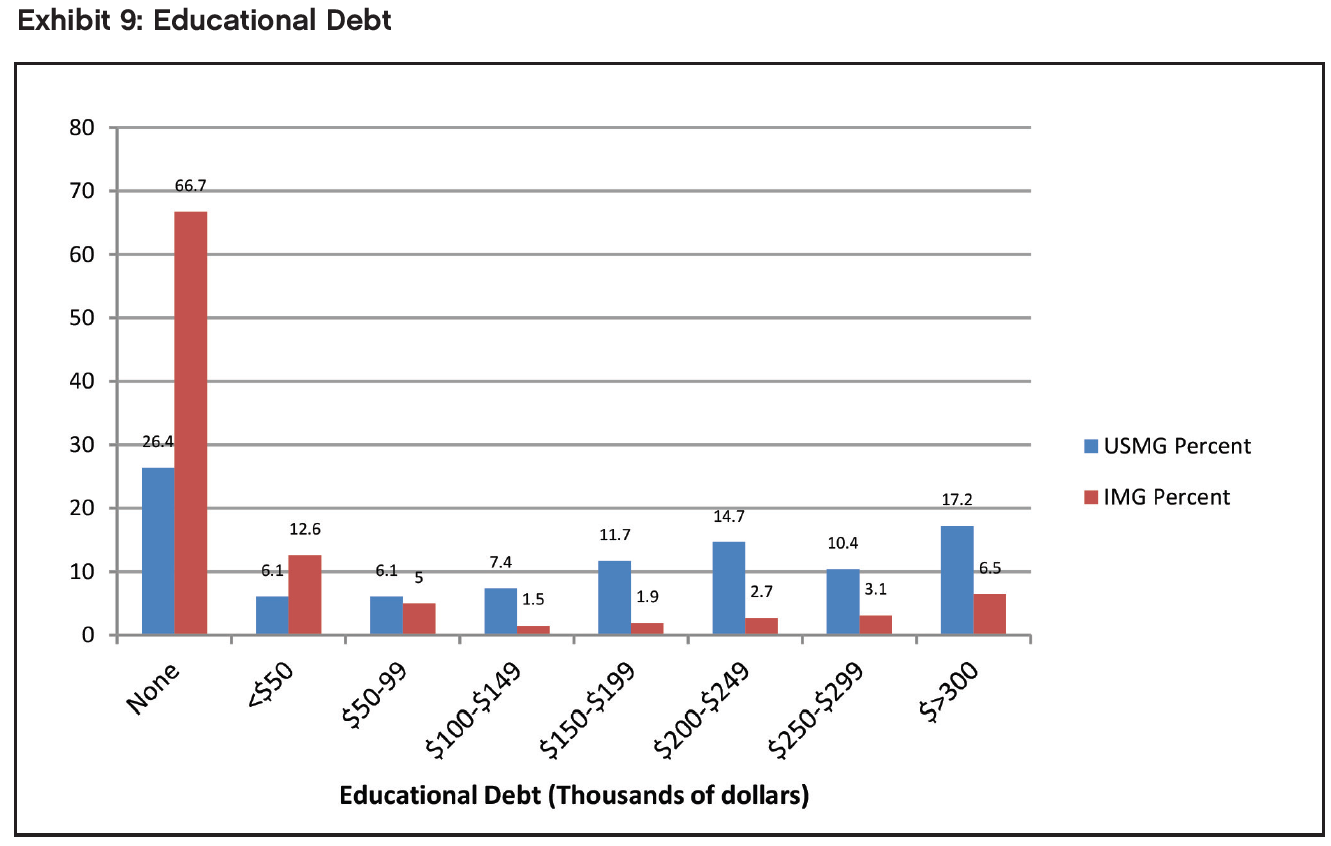
Educational Debt
Respondents’ reported levels of educational debt varied from no debt to greater than $300,000. As in previous years, IMGs were much less likely to be in debt than USMGs: 66.7% of IMG respondents reported having no educational debt compared with only 26.4% of USMGs (p<0.001, effect size = 0.824). (Effect sizes are typically classified as 0.2=low, 0.5=medium, 0.8=large; the measure of effect size used throughout is Cohen’s d.) An additional 12.6% of IMGs reported educational debt levels <$50,000. USMG respondents were more likely than IMGs to report debt levels in every debt tier beyond $50,000. More than 1 in 6 (17.2%) of USMG respondents and 6.5% of IMG respondents reported having >$300,000 of educational debt, compared to 2016 when the comparable figures were 8.7% and 5.5% respectively. IMG respondents had a median educational debt of $0, while USMG respondents had a median educational debt of between $150,000 and $174,999, which is higher than in any of the previous survey years.
Obligations to Practice in Underserved Areas
The difference in the distribution of HPSA service obligations by IMG status was highly significant (p<0.001, effect size=0.791). While 78 IMGs (29.7%) indicated an obligation to work in a federally designated HPSA, only 1 (0.6%) USMG did.
Post-Training Plans (2nd-Year and Beyond Fellows Only)
Activity After Completion of Current Training Year
Among respondents in their second year of fellowship or beyond who indicated their plans for the upcoming year (n=252), the largest percentage planned to enter clinical nephrology practice (54.4%). Thirty-one percent (31%) are continuing their training: 16.3% in their current fellowship and 14.7% in subspecialty training or an additional fellowship.
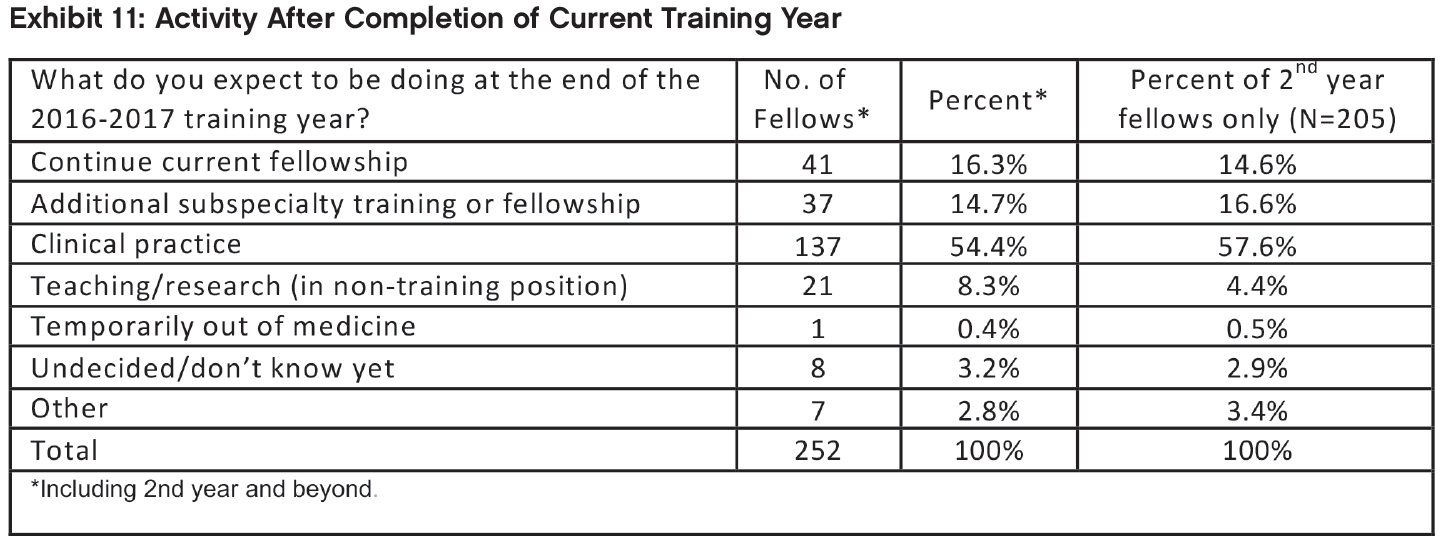
As seen in Exhibit 12, among the 77 fellows who planned to continue their training (either through additional subspecialty training or by continuing in their current fellowships) and gave information about what further training they planned to undertake, the largest groups said they planned to pursue training in research (36 respondents), transplant nephrology (23 respondents) and critical care (7 respondents). A smaller group (4 respondents) said they planned to pursue training in interventional nephrology. As in 2016, other types of training respondents mentioned included clinical nutrition and glomerular disease.
USMGs were significantly more likely than IMGs to report that they planned to continue their current fellowships (22.7% vs. 11.8%, p<.05, effect size = 0.299). We found no other significant differences in the distribution of anticipated activities between USMG and IMG fellows.
We found no significant difference in the distribution of anticipated activities between male and female fellows.
Job Selection
Respondents in their second year of fellowship or beyond rated the following factors as very important or important in their job selection:
Frequency of weekend duties (96.3% very important or important)
Frequency of overnight calls (94.0%)
Job/practice in desired location (94.0%)
Salary/compensation (92.0%)
Job/practice in desired practice setting (89.4%)
Length of each workday (88.5%)
They rated the following factors as least important:
Climate (57.5% of little importance or not important at all)
Taxes (53.8%)
Cost of malpractice insurance (52.5%)
Cost of setting up a medical practice (46.3%)
Job/practice meets visa requirements (38.4%)
Factors Influencing Job Selection
USMGs and IMGs differed significantly when rating the following factors:
Job/practice meets visa requirements (IMGs more likely than USMGs to rate as very important or important, p<0.01, effect size = 1.1)
Cost of establishing a medical practice (IMGs more likely than USMGs to rate as very important or important, p<.05, effect size = 0.44)
Frequency of overnight calls (IMGs more likely than USMGs to rate as very important or important, p<.01, effect size=0.40)
Salary/compensation (IMGs more likely than USMGs to rate as very important, p=0.001, effect size=0.49)
Cost of malpractice insurance (IMGs more likely than USMGs to rate as very important, p<.01, effect size=0.41)
Taxes (IMGs more likely than USMGs to rate as very important, p<.01, effect size = 0.42)
USMG and IMG fellows’ ratings of other factors were not significantly different.
Male and female fellows differed significantly when rating the following factors:
Job/practice in desired setting (female fellows more likely than male fellows to rate as very important, p<0.05, effect size=0.36)
Climate/weather (female fellows more likely than male fellows to rate as very important, p<0.01, effect size=0.44)
Male and female fellows’ ratings of other factors were not significantly different.
Job Market Experiences and Perceptions
This section reports on the experiences of the 160 nephrology fellows who had searched for employment. As in previous years, the job market was challenging, especially for IMG fellows who were more likely than USMG fellows to report applying for large numbers of jobs, having difficulty finding a satisfactory position, and changing plans because of limited opportunities. Nevertheless, signs of improvement included fewer job applications, fewer people receiving no job offers, fewer IMGs reporting difficult finding a satisfactory position and fewer people reporting lack of jobs in both local and national job markets.
Number of Job Applications
Among fellows who had searched for a job, 63.7% reported applying for between 1 and 5 jobs, and 33.8% reported that they had applied for at least 6 jobs (including 17.5% who applied for more than 10 jobs). A few fellows (2.5%) reported that they had not applied for any jobs.
We found a statistically significant difference in the number of job applications between IMG and USMG fellows (p=0.01): IMGs were more likely than USMGs to apply for more than 10 jobs (21.8% of IMGs vs. 10.2% of USMGs), and USMGs were more likely than IMGs to apply for 1 to 5 jobs (74.6% vs. 57.4%). The percentage of USMGs who reported that they applied for 6 or more positions declined from 34.0% in 2016 and 43.5% in 2015 to 22.1% in 2017 (lower than even the 28.6% of 2014).
The percentage of IMGs who reported applying for 6 or more jobs fell from 61.7% in 2016 and 63.3% in 2015 to 40.6% (lower even than the 47.4% of 2014).
We found no statistically significant differences in the number of job applications between male and female fellows (p=0.22).
Number of Job Offers
The majority of nephrology fellows (67.9%) reported receiving between 1 and 3 job offers. A small number of fellows reported receiving more than 10 job offers (1.9%), and 5% of fellows reported receiving no job offers. The percentage of USMGs who reported receiving no job offers (1.7%) was lower than in 2016 (4.0%) and 2015 (3.8%).
USMGs were more likely to report receiving 1 to 3 job offers (83.1% vs. 59%), and IMGs were more likely to report receiving no job offers (7% vs. 1.7%) but also more likely to report receiving 4 offers or more (34% vs. 15.2%). The differences were not statistically significant.
We found no statistically significant differences in the number of job offers between male and female fellows (p=0.28).
Difficulty Finding a Satisfactory Position
Fewer than half of respondents (45.6%) who had searched for jobs reported having difficulty finding a satisfactory position (Exhibit 14) compared to 53.1% in 2016. We found a statistically significant difference between IMG and USMG fellows’ reports of difficulty finding a position (p=0.001): 55.4% of IMGs reported having difficulty finding a position they were satisfied with, a substantial improvement over the 70.0% of 2016. 28.8% of USMGs reported having difficulty compared to 26% in 2016.
We found no statistically significant difference in reports of difficulty finding a position between male and female fellows (p=0.29).
Reasons for Difficulty
Among the fellows who reported difficulty finding a satisfactory position, the top 3 most frequently cited reasons were consistent from 2016 to 2017. The reasons most frequently cited by 2017 fellows were lack of jobs/ practice opportunities in desired locations (31.5%) inadequate salary/compensation (21.9%) and lack of jobs/ practice opportunities that meet visa status requirements (16.4%). Difficulties with visa status requirements were reported at a much lower level than in 2016, when the corresponding figure was 27.5%.
IMGs were statistically significantly more likely than USMGs to cite lack of jobs that meet visa requirements (21.4% vs. 0%, p=0.0372, effect size 0.588). They were also more likely to cite overall lack of jobs and opportunities (16.1% vs. 11.8%) while USMGs were more likely than IMGs to cite lack of jobs in desired locations (47.1% vs. 26.8%), but none of these differences were statistically significant. (In 2016 IMGs were more likely to cite lack of jobs in desired locations and USMGs were more likely to cite inadequate salary/compensation.)
We found no statistically significant difference in the reasons for difficulty finding a position between male and female fellows (p=0.547).
Changing Plans Due to Limited Practice Opportunities
Overall, the percentage of respondents indicating that they had changed their plans because of limited nephrology job opportunities continued its decline, from 42.9% in 2015 to 35.4% in 2016 and 32.7% in 2017. While both USMGs and IMGs were less likely to report changing their plans in 2017 than in prior years, their likelihood of changing plans was significantly different: only 13.6% of USMGs reported that they had to change plans, while 44% of IMGs reported changing plans (p<0.001, effect size=0.679). This difference likely reflects a continuing lack of job opportunities that meet visa requirements while allowing IMGs to practice in their preferred locations or settings.
We found no statistically significant differences in male and female fellows’ likelihood of changing their plans (p=0.41).
Job Market Perceptions
Survey respondents were asked to indicate their perceptions of the local job market (within 50 miles of where they trained) and the national job market. Response options ranged from no jobs to many jobs. Key findings include:
Perceptions of the local and national job markets were more positive in 2017 (vs. 2015 and 2016) for both USMGs and IMGs;
As in the previous years, the 2017 fellows were more likely to indicate that there were few or no job opportunities in the local job market compared to the national market; and
As in previous years, USMGs had a far more favorable view of the local and national job markets than IMGs.
Local Job Market Perceptions
Among nephrology fellows who had searched for jobs, perceptions of local nephrology job opportunities were improved since 2016: while 37.7% reported that there were many or some nephrology practice opportunities within 50 miles of their training sites in 2016, the proportion reporting the same in 2017 increased to 41.5%.
We found a statistically significant difference in IMG and USMG fellows’ assessments of local nephrology practice opportunities with USMGs more likely than IMGs to report that there were many or some job opportunities in their local area (57.2% vs. 32.3%, p<0.001, effect size=0.700).
We found no statistically significant differences in local job market perceptions between male and female fellows (p=0.50).
National Job Market Perceptions
Nephrology fellows continued to perceive national nephrology job opportunities much more positively than local opportunities: 69.1% reported there were some or many nephrology practice opportunities nationally (up from 63% in 2016) compared to 41.5% reporting some or many nephrology practice opportunities locally.
In contrast to 2016 we found a statistically significant difference in IMG and USMG fellows’ assessments of national nephrology practice opportunities, with USMGs more likely than IMGs to report that there were many or some job opportunities nationally (82% vs. 61.7%, p<0.001, effect size=0.649).
We found no statistically significant difference between male and female fellows’ assessments of national nephrology practice opportunities (p=0.36).
Types of Jobs Available
When we asked fellows to indicate in an open-ended question what types of jobs they perceived to be more and less available for newly graduating fellows, they mentioned several types of jobs that were more easily available according to their experience:
Jobs in remote, rural or undesirable areas (e.g., Midwest, South), especially with large dialysis providers
Private practice jobs
Jobs in solo or small practices/hospitals/communities
They also mentioned several types of jobs that were less easily available according to their experience:
Academic jobs
Jobs in metro areas or other preferred geographic areas (e.g., Florida, California, Pacific Northwest)
Jobs that meet visa requirements for IMGs
A small number of respondents mentioned limited availability of hospital jobs and private practice positions, with the problem more acute when combined with one of the other categories of shortfall such as urban situation.
Job Offer Characteristics
Among the 119 nephrology fellows who had already accepted job offers, we found the following with respect to their salary and compensation expectations.
Practice Setting
Among respondents who had already accepted job offers, the largest group (43.1%) reported that they planned to work in nephrology group practices. Another 23.3% reported that they planned to work in academic nephrology practices, 11.2% said they planned to work in hospitals and another 11.2% in 2-person partnerships. Other settings included multispecialty group practices (5.2%) and multispecialty academic practices (3.4%).
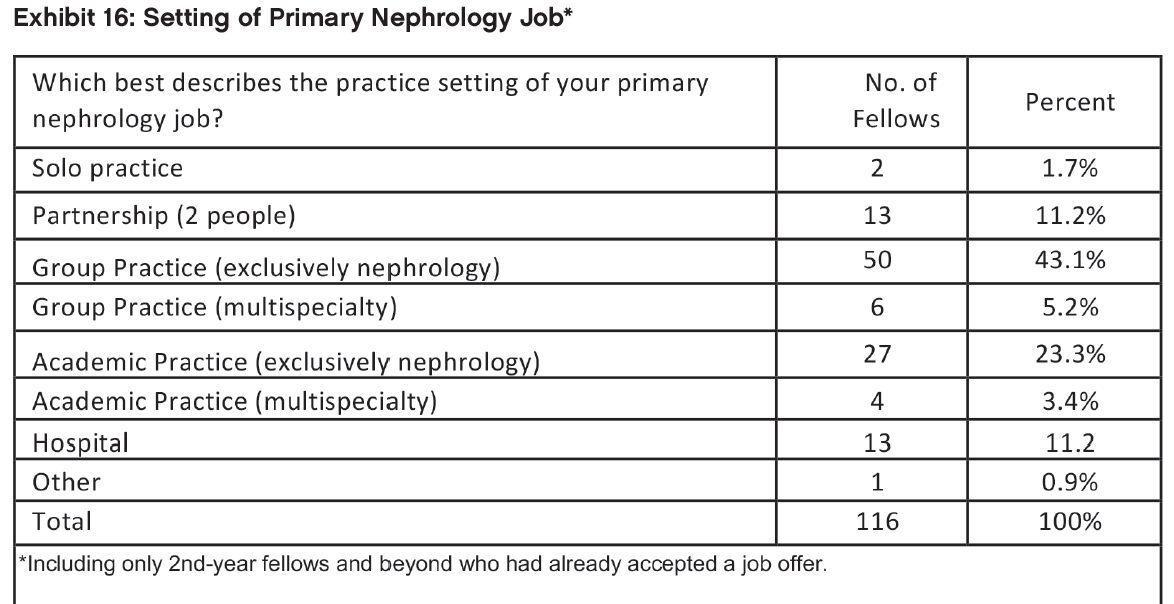
The only difference between USMGs and IMGs in setting distribution that reached statistical significance was for hospital settings, where 16.4% of IMGs but only 4.1% of USMGs reported working (p<.05, effect size=0.395).
Female fellows were more likely to report that they planned to work in academic nephrology (25.0% vs. 22.2%), 2-person partnerships (15.9% vs. 8.3%) and hospitals (13.6% vs. 9.7%); and male fellows were more likely to report that they planned to work in nephrology group practices (45.8% vs. 38.6%) and multispecialty group practices (8.3% vs. 0%). However, none of the differences were statistically significant (p=0.26).
Location of Practice
Among respondents with job offers, almost half (49.1%) indicated that they planned to work in urban areas (inner city or other). Another 22.4% said they planned to work in suburban areas, and 20.7% said they planned to work in small cities. In contrast to 2016, when only 1 fellow (1.0% of respondents) reported intending to work in a rural area, in 2017 there were 9 fellows (7.8% of respondents) reporting intending to work in a rural area.
The distribution of practice locations was different for USMGs and IMG fellows (p<0.05 for all differences). USMGs were more likely to report intending to work in suburban areas (32.7% vs. 14.9%, p=0.0237, effect size=0.431) and other urban areas (32.7% vs. 17.9%, not significant), while IMGs were more likely to report intending to work in inner cities (29.9% vs. 18.4%, not significant), small cities (26.9% vs. 12.2%, almost significant p=0.0555, effect size=0.364) and rural areas (10.4% vs. 4.1%, not significant).
We found no statistically significant differences between male and female fellows’ anticipated practice locations (p=0.36).
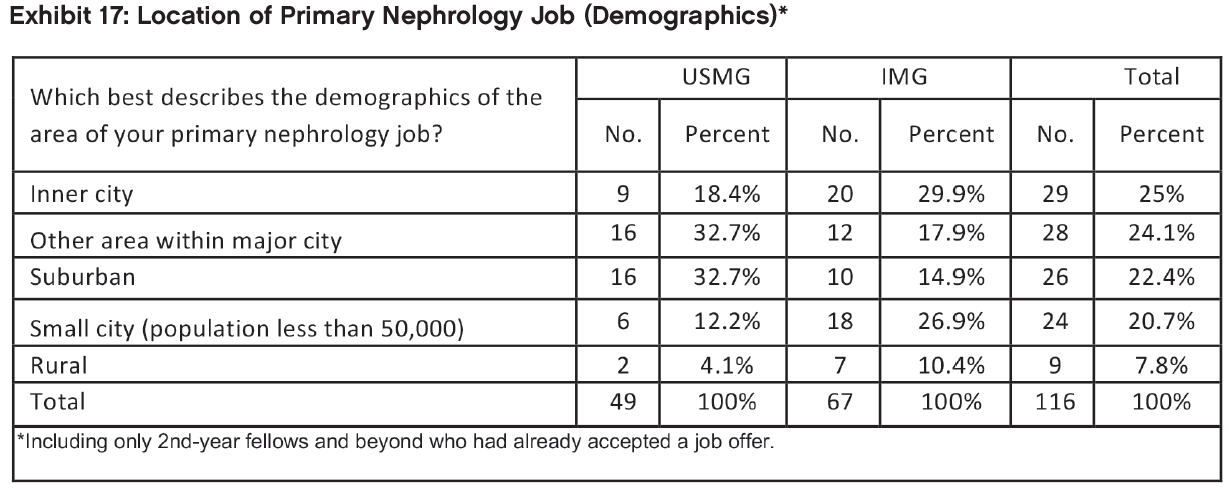
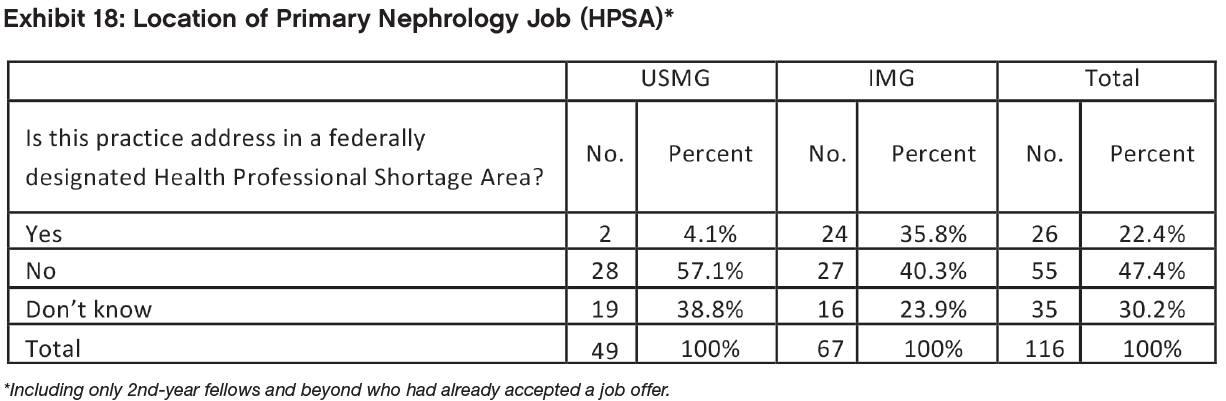
Among the 116 respondents who indicated whether their job offers were located in a HPSA, 22.4% (26 respondents) reported their principal practice address was in a HPSA. (Almost one-third of this group [30.2%] did not know, and the rest [47.4%] said not.) Among the 26 respondents who planned to work in a HPSA, 24 were IMGs. The difference in distribution of IMGs’ and USMGs’ practice locations was statistically significant (p<0.001, effect size=0.940).
We found no statistically significant differences between male and female fellows’ intentions to practice in a HPSA (p=0.69).
Base Salary/Income
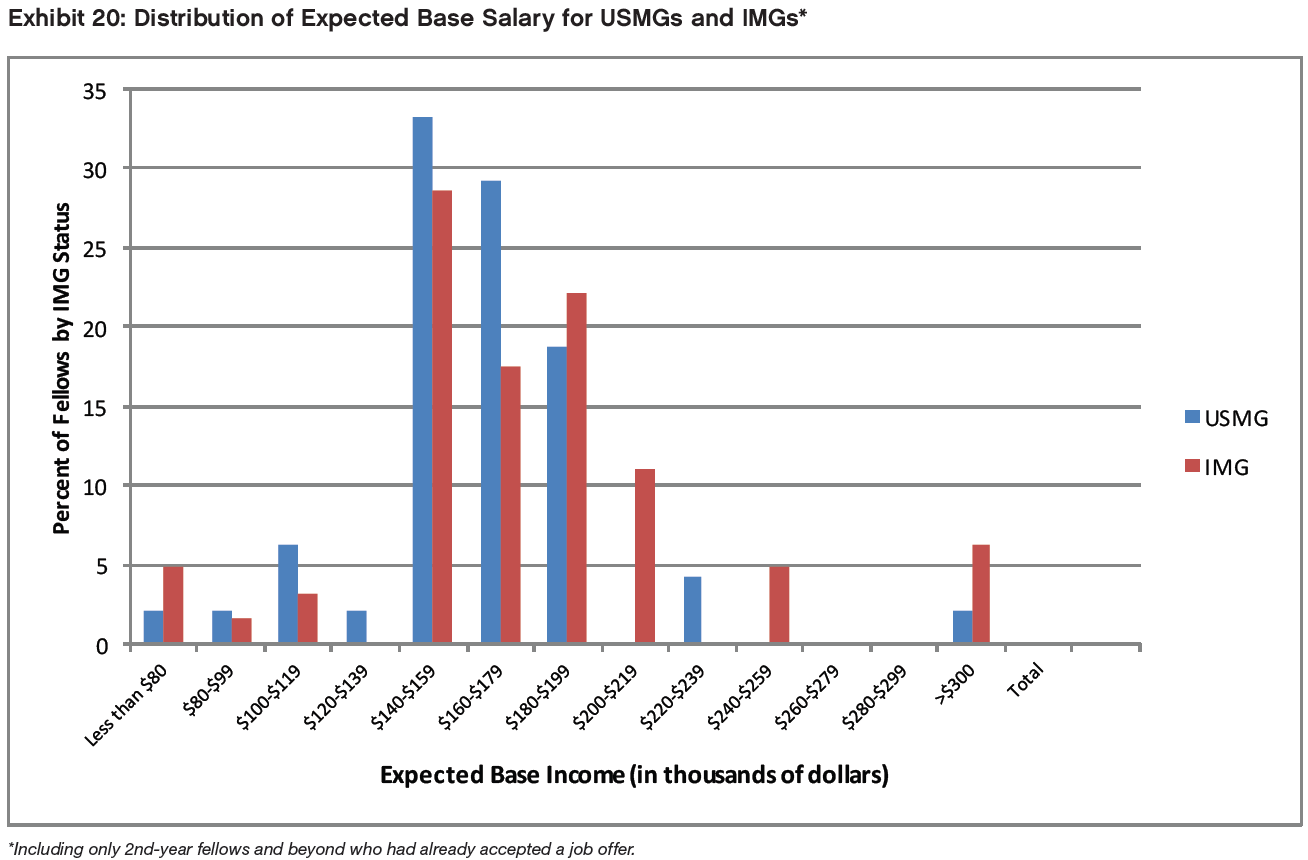
Among the fellows who had accepted job offers, the range of expected salaries was from <$50,000 to $329,999. Almost two-thirds (63.1%) anticipated annual base salaries between $160,000 and $209,999.
Perhaps surprisingly, male USMGs had the lowest median expected base salaries of all demographic groups by IMG status and gender, in the range $170,000–$179,999. Female USMGs and Male IMGs had median expected base salaries in the range $180,000–$189,999. Female IMGs had the highest median base salaries, in the range $200,000–$209,999.
Exhibit 19 shows that female USMGs had average expected base salaries a statistically significant $25,000 higher than male USMGs (p<.05 in both one-sided and two-sided t-tests, effect size=0.627). This is an unusual result and not in line with previous years’ surveys. The lower average male salary remained after controlling for hours worked and appears to be driven by a small number of male outliers (5) with much lower base salaries than the average (all 5 reported base salaries under $140,000, down to as low $70,000–$79,999), in contrast to only 1 female USMG earning less than $150,000. Further examination of setting and practice location provided no additional explanation of this difference and additional research would be warranted if this difference reappeared in next year’s survey.
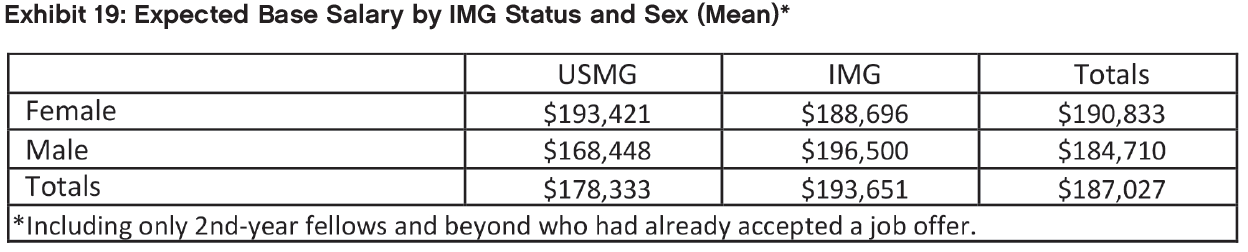
In contrast to the result for median salaries, female IMGs had almost $8,000 lower average expected base salaries than male IMGs (though this difference was not statistically significant, p=.71), suggesting that male IMGs were overrepresented at the highest earning levels. IMGs overall had $15,000 higher average expected base salaries than USMGs, a difference that was almost statistically significant in a one-sided t-test (p=.052).
(Because survey respondents were only asked to report their salaries within $10,000 ranges, the calculation of mean values set out in Exhibit 19 relies on the assumption that actual salaries were evenly distributed within each salary range, which cannot be guaranteed.)
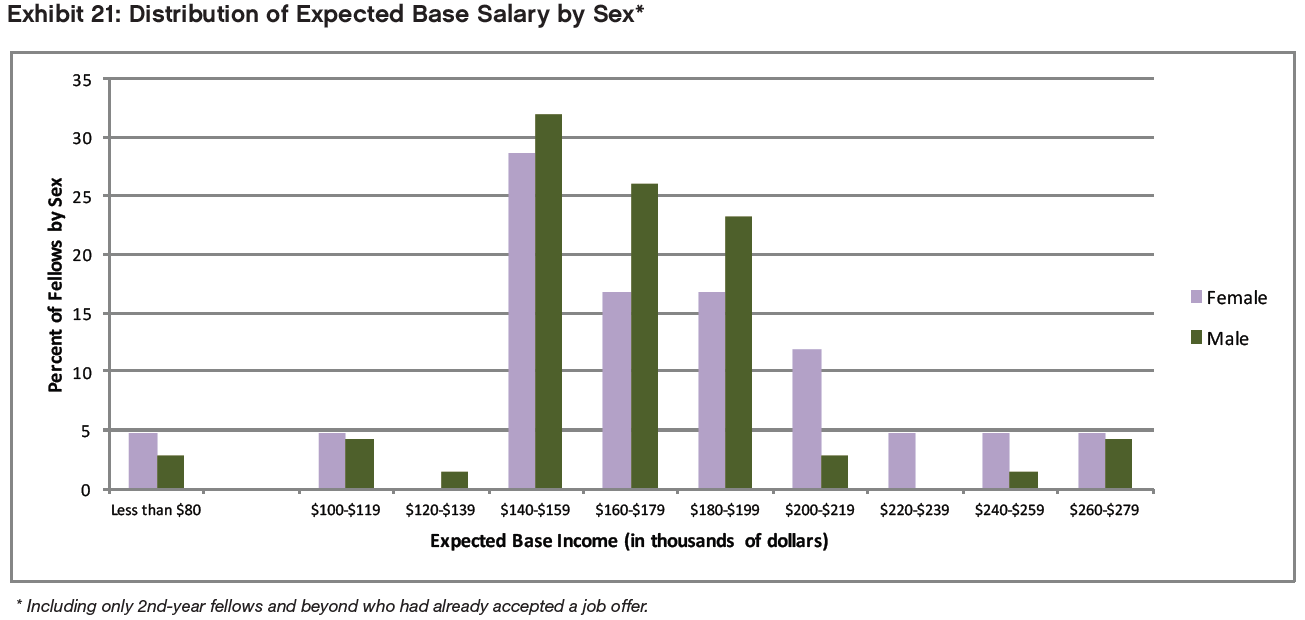
Exhibits 20 and 21 show fellows expected base salaries in histogram form. In the histograms IMGs are in higher numbers than USMGs above $180,000 and in lower numbers below $180,000 but the overall distribution of expected salaries was not significantly different between IMGs and USMGs (p=0.10). Female fellows were more highly represented than male fellows above $200,000 and less represented below $200,000. Again, however, the difference was not statistically significant (p=0.53).
Anticipated Additional Incentive Income
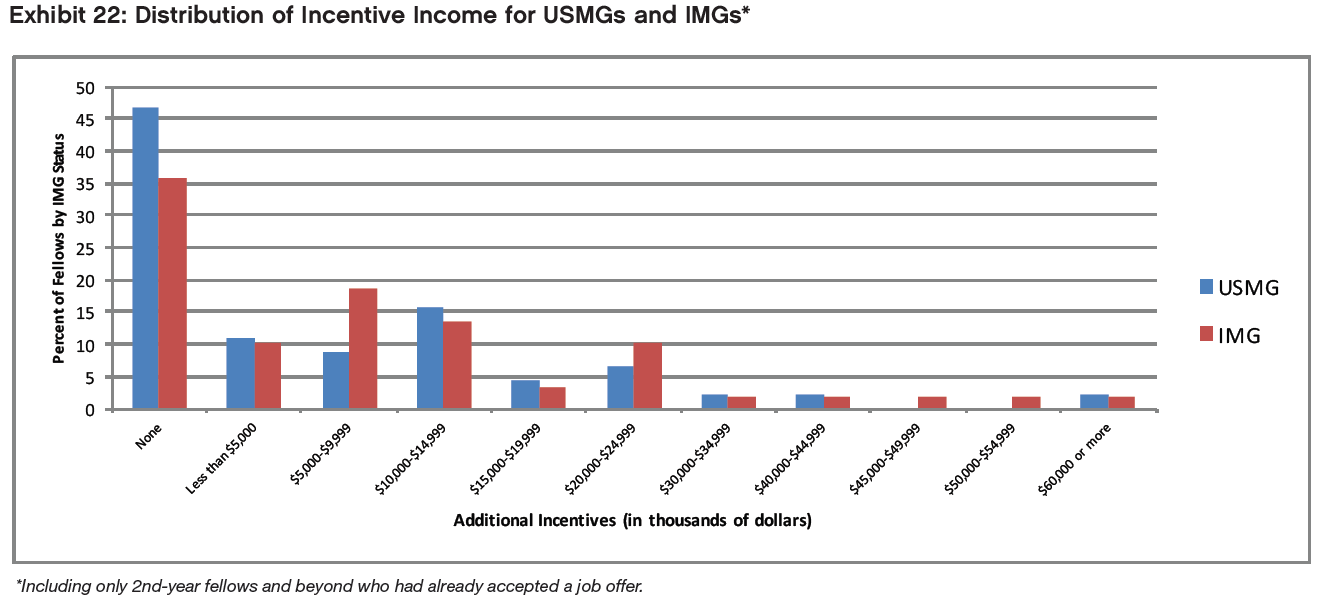
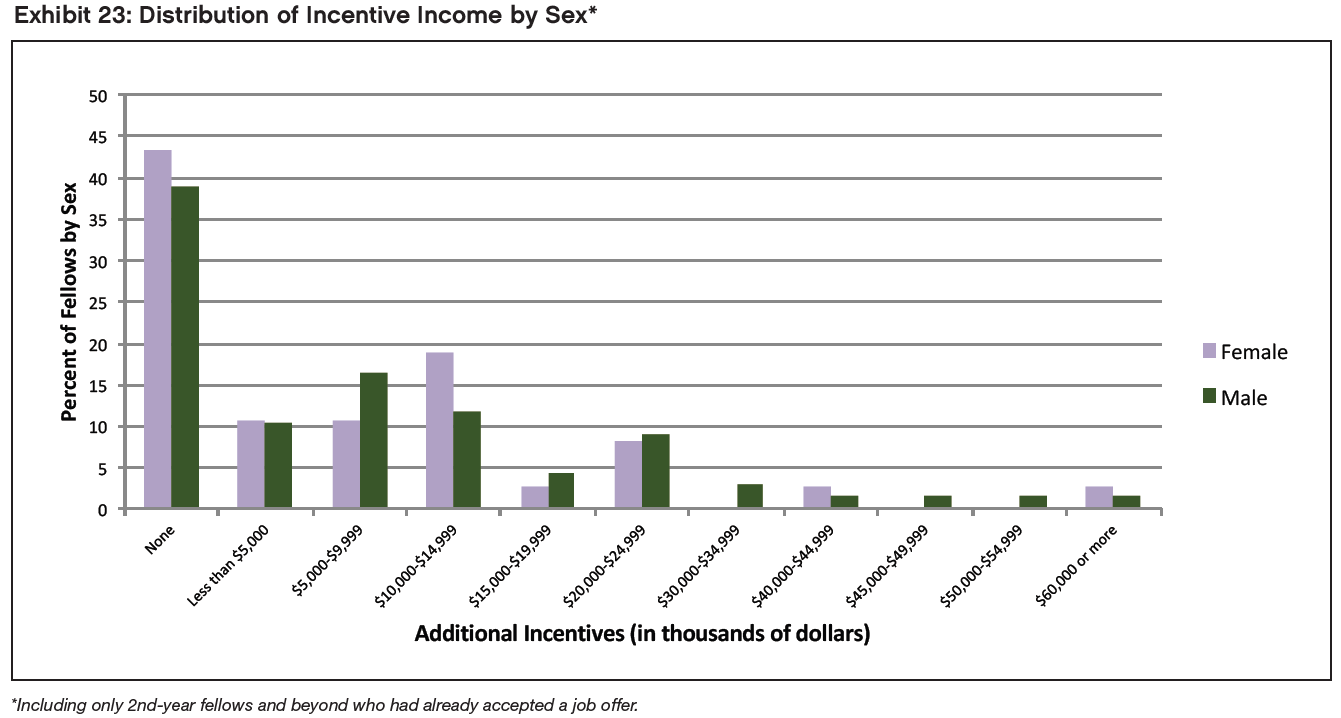
Less than half (40.4%) of fellows who had accepted job offers did not anticipate receiving any additional incentive income. Among those expecting to receive incentive income, most reported that they expected to earn less than $15,000, although the range of expected incentives extended beyond $30,000 for 3 fellows and beyond $60,000 for one of those. (Five respondents reported incentive income above $60,000 in 2016.)
Exhibits 22 and 23 show fellows’ expected incentive income in histogram form. We found no significant differences in expected incentive income between IMGs and USMGs (p=0.42) or male and female fellows (p=0.65).
Secondary Jobs
Among the respondents who had accepted nephrology jobs, 24 indicated that they planned to take on a second nephrology job in addition to their primary job. Half (12 respondents, 50%) planned to take medical directorships with dialysis providers. Other secondary job responsibilities cited included moonlighting in nephrology inpatient units (6 respondents, 25%), moonlighting in non-nephrology inpatient units (6 respondents, 25%), hospital care (4 respondents, 16.7%) and joint ventures with dialysis providers (3 respondents, 12.5%).
Among fellows who reported their expected income from secondary nephrology jobs, well over half (61.1%) expected to earn less than $30,000 in their secondary jobs. Only 3 of these respondents (16.8%) expected to earn more than $50,000 from secondary nephrology jobs.
Income Comparisons
Using the income calculation methodology detailed in our 2016 report, we conducted statistical comparisons of mean anticipated incomes (primary job base salary plus incentive income) between IMGs/USMGs and male/female fellows. We found no statistically significant differences for either comparison (p=0.12 and p=.085 respectively, two-sample t-test), likely because differences in primary job salary between males and females for IMGs and USMGs cancelled each other out.
When we compared mean anticipated incomes between fellows planning to work in different practice locations (e.g., inner cities, suburban areas) we found a statistically significant difference (p=0.01), with the highest average incomes in small city ($213,700) and rural areas ($212,200), and lower incomes in suburban ($185,800), large city areas other than inner city ($175,000), and inner city ($169,100) areas. This stands in contrast to 2016 when the differences were not statistically significant.
As in 2016 we found a statistically significant difference in mean anticipated incomes between different practice settings (p<0.001): fellows planning to work in academic nephrology ($160,900), multispecialty academic nephrology ($172,500), 2-person partnerships ($173,100) and nephrology group practices ($192,200) had the lowest mean anticipated incomes, while fellows planning to work in multispecialty group practices ($201,700) and hospitals ($246,700) had the highest mean anticipated incomes. A figure of $135,000 for mean anticipated income in solo practice came from only 2 respondents and is distorted by the very low income reported by 1 respondent (the other respondent reported an income of $207,500). One respondent reported their setting as “academic practice exclusively transplant nephrology” and was rolled into the academic nephrology group.
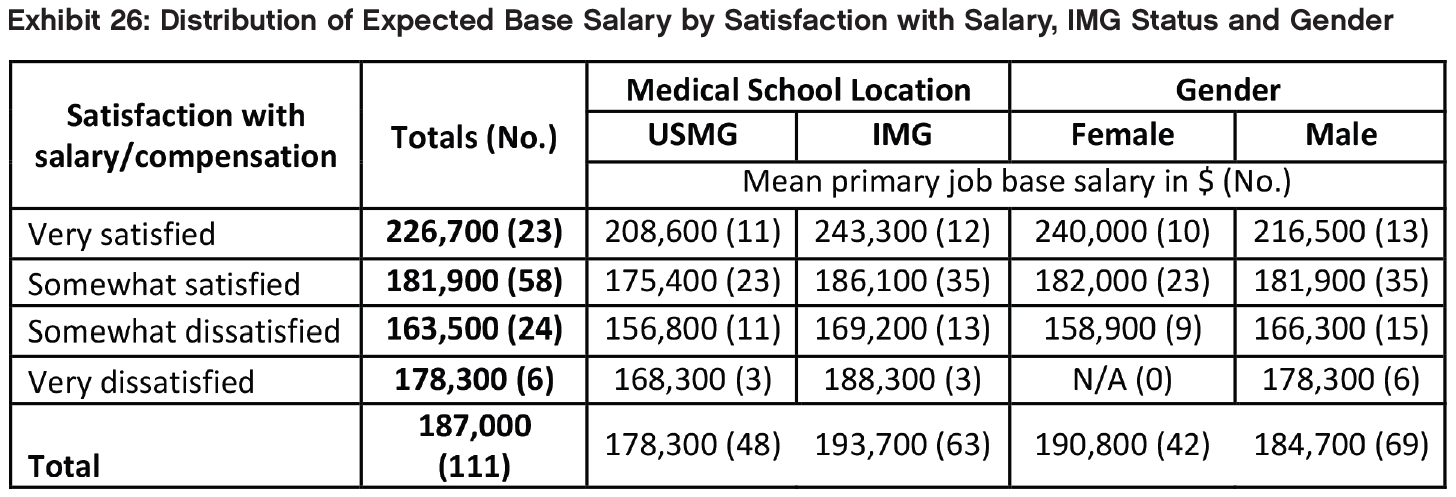
Satisfaction with Salary/Compensation
The majority of fellows who had accepted job offers indicated they were satisfied with their salary and compensation. Of these 20.4% reported being “very satisfied” (though this was rather lower than the corresponding figure of 31.6% in 2016), and 53.1% indicated that they were “somewhat satisfied” with their salary and compensation.
USMGs were slightly more likely to report being “very satisfied” with their salary and compensation (22.9% vs. 18.5%), while IMGs were more likely to report being “somewhat satisfied” (56.9% vs. 47.9%). The differences were not statistically significant (p=.82)
Female fellows were a little more likely than males to report being “very satisfied” with their salary and compensation (23.3% vs. 18.6%, but much lower than the corresponding figure of 48.7% for females in 2016) while male fellows were more likely to report being “very dissatisfied” (8.6% vs. 0%). Again, the differences were not statistically significant (p=0.25).
Those with higher salaries were generally the most satisfied. A small group of 6 (all males) were “very dissatisfied” with an average salary of around $178,000. The difference in mean salary between the “very satisfied” and the “somewhat dissatisfied” groups was around $63,000.
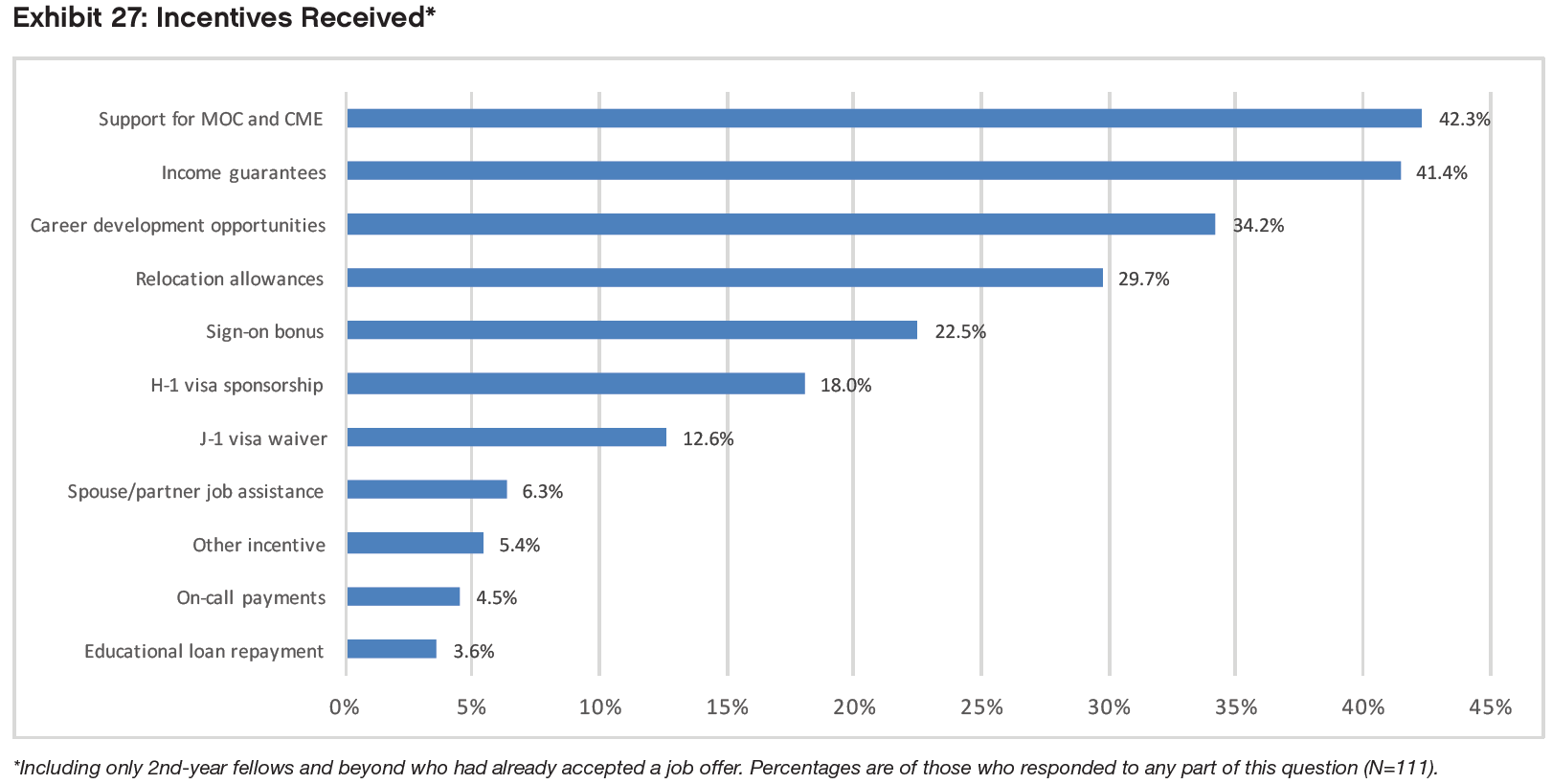
Incentives
When asked to identify the incentives they had received for accepting their primary job offers, respondents were most likely to report receiving the following:
Support for MOC and CME (42.3%)
Income guarantees (41.4%)
Career development opportunities (34.2%)
Relocation allowances (29.7%)
Sign-on bonus (22.5%)
Educational loan repayment (3.6%) and on-call payments (4.5%) were the least frequently reported incentives; 15.3% of respondents who had accepted jobs reported receiving no incentives.
Not surprisingly, we found statistically significant differences between IMG and USMG respondents’ reports of receiving H-1 visa sponsorship (31.3% vs. 0%, p<0.001, effect size=0.361) and J-1 visa waivers (21.9% vs. 0%, p<0.001, effect size=0.299). A statistically significant difference was also found between IMGs’ and USMGs’ reports of receiving educational loan repayments (0% vs. 8.5%, p<.05, effect size=0.525).
We also found a statistically significant difference between male and female respondents’ reported incentives in regard to spouse/partner job transition assistance (males 10.1% vs. females 0%, p<.05, effect size=0.209). Gender differences around income guarantees also reached statistical significance (males 49.3% vs. females 28.6%, p<.05, effect size=0.187).
Among respondents who reported receiving incentives with their primary job offers, two-thirds (67.0%) reported that they were “important” or “very important” in their decision to accept the job. We found a statistically significant difference between IMGs’ and USMGs’ ratings of the importance of the incentives they had received with IMGs more likely than USMGs to rate the incentives they had received as “important” or “very important” (76.8% vs. 52.6%, p<0.01, effect size=0.525).
We found no statistically significant differences between male and female respondents’ ratings of the importance of the incentives they had received (p=0.77).
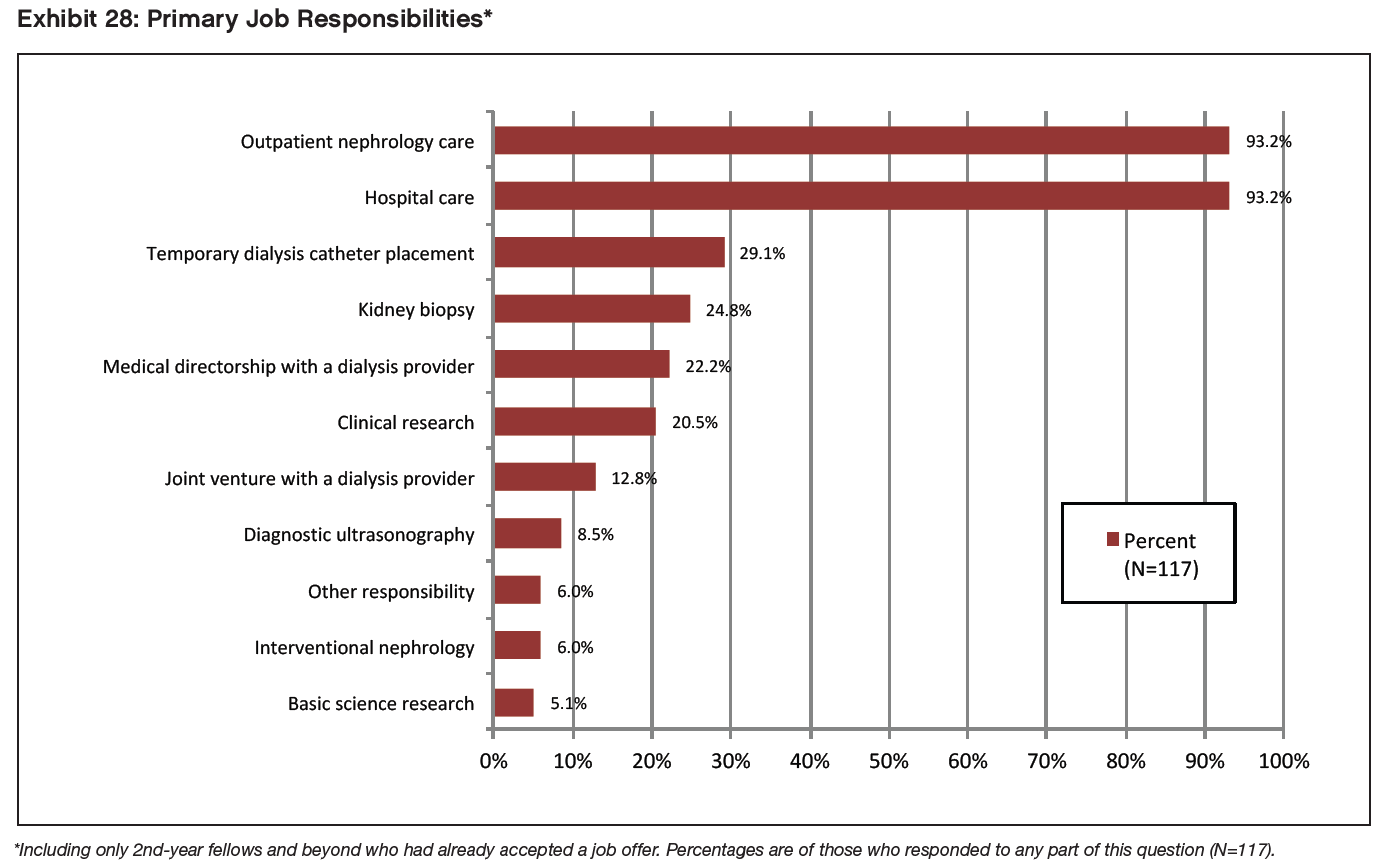
The vast majority of respondents cited outpatient nephrology care and hospital care among their primary job responsibilities (93.2% for each). Other responsibilities they listed included temporary dialysis catheter placement (29.1%), kidney biopsy (24.2%), medical directorship with a dialysis provider (22.2%) and clinical research (20.5%).
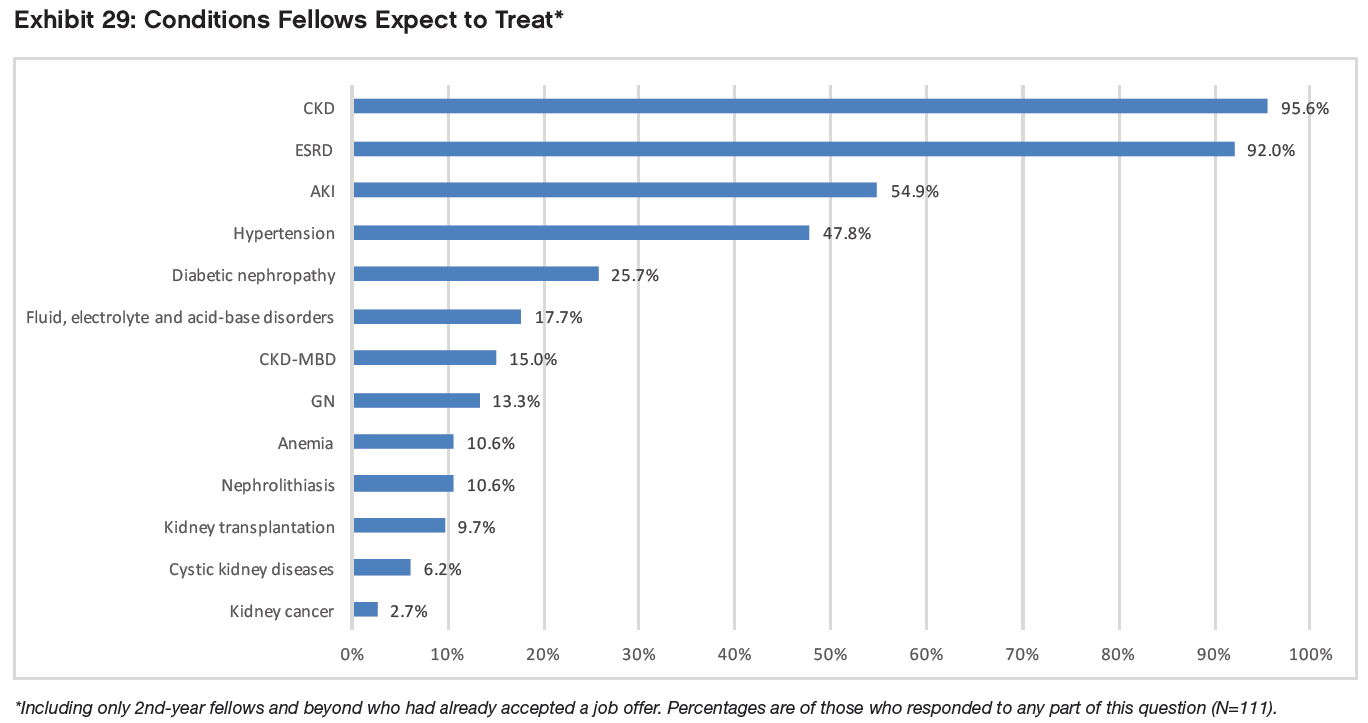
Conditions Fellows Expect to Treat
When asked to identify the top 3 conditions they expected to treat in their practice (both primary and secondary jobs), respondents who had accepted job offers most frequently cited CKD (95.6%), ESRD (92.0%), AKI (54.9%), and hypertension (47.8%)—the same conditions as in 2015 and 2016. The least frequently expected conditions were kidney transplantation (9.7%), cystic kidney diseases (6.2%), and kidney cancer (2.7%)— again, the same conditions as in 2016.
Dialysis Modalities
Among dialysis modalities (N=111), respondents who had accepted job offers were most likely to expect to work with in-center hemodialysis (99.1%), followed by home peritoneal dialysis (72.1%), and home hemodialysis (41.4%). A much smaller group (18.9%) said they anticipated working with nocturnal in-center hemodialysis.
Additional Instruction Desired in Fellowship
When asked about fellowship topics they would most like to receive additional instruction in during fellowship the highest response rates were for home hemodialysis (52.8%), kidney US interpretation (48.5%), peritoneal dialysis (47.5%) and acute GN diagnosis/management (35.9%).
Deciding to Pursue Nephrology
The majority (62.5%) of fellows did not make the decision to pursue nephrology as a specialty until their residency, and 50 fellows (12.1%) had practiced another area of medicine before deciding to take up nephrology.
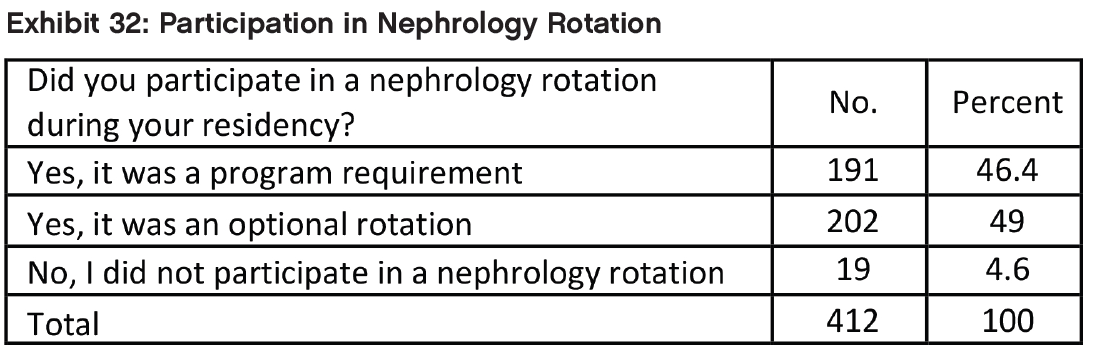
Almost all fellows (95.4%) had participated in a nephrology rotation, although it was a program requirement for fewer than half of them.
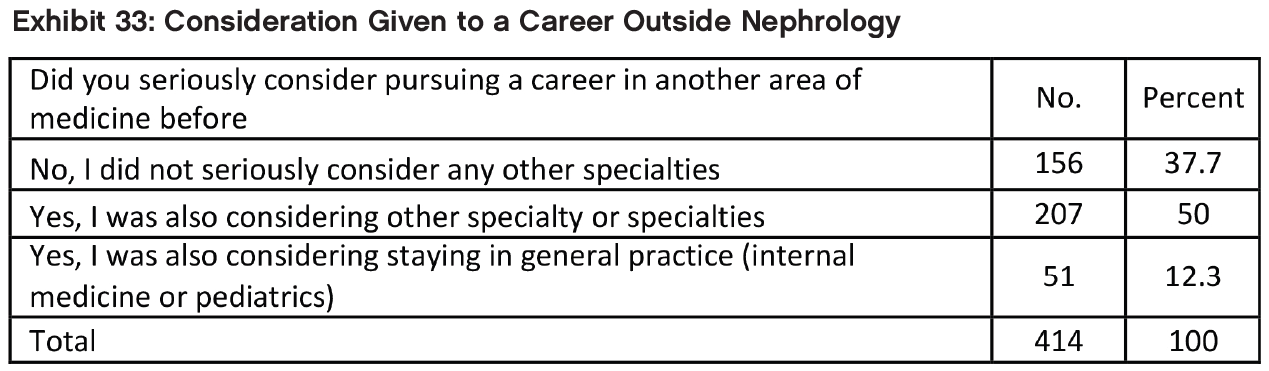
The majority of respondents (62.3%) had seriously considered another specialty before deciding to pursue nephrology. In the 104 written responses, the most frequently mentioned alternative specialties were pulmonary and critical care (30.7% of 140 total specialty mentions), cardiology (14.3%) and hematology/oncology (13.6%). Gastroenterology, endocrinology and hospital medicine (in decreasing order of frequency) were also mentioned.
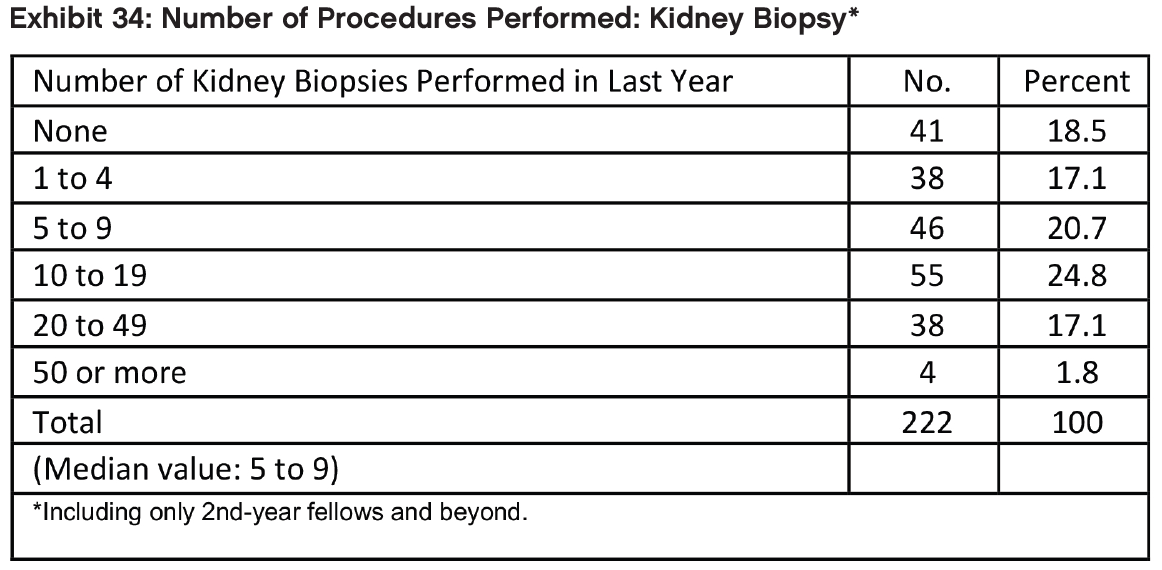
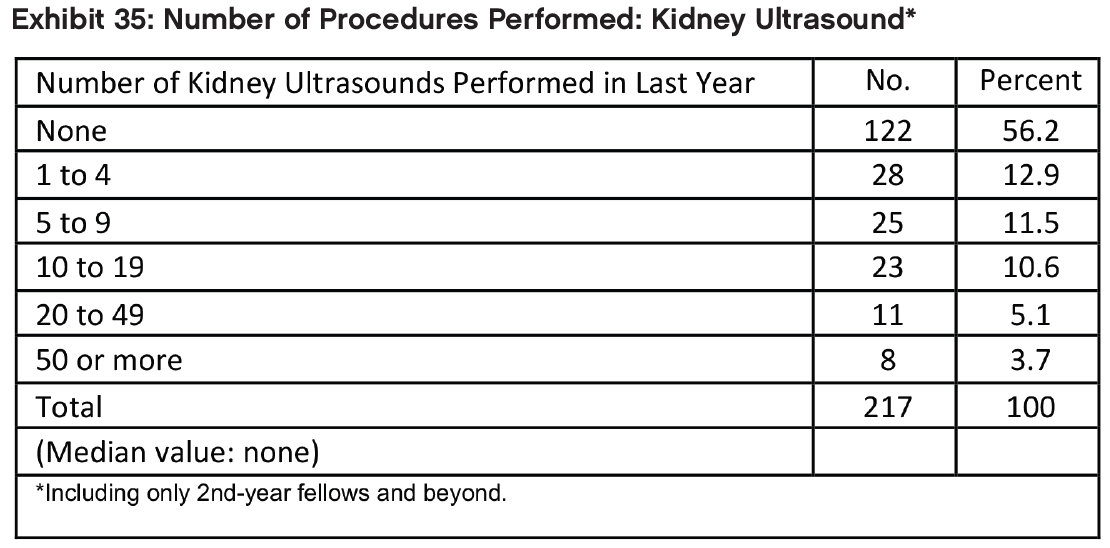
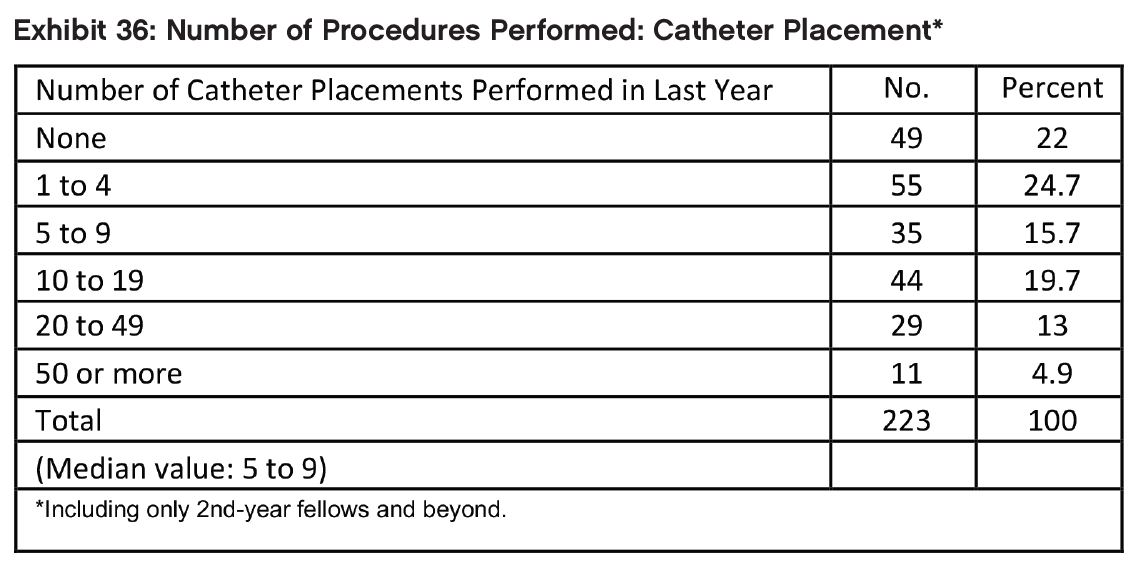
Procedures
Kidney biopsy and catheter placement by fellows in their second year and beyond followed similar patterns in terms of frequency of being performed, with the median for both in the range 5 to 9 procedures in the past year. Kidney ultrasound was performed less frequently with a majority performing no kidney ultrasounds in the past year.
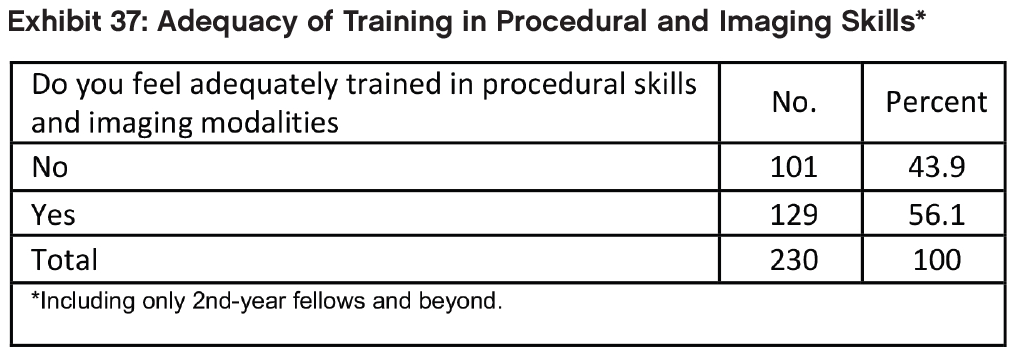
Respondents in their second year and beyond who felt adequately trained in procedural and imaging skills were in the majority (56.1%), and some of those who felt adequately trained felt they could say this in relation to some but not all procedures. Analysis of 120 positive freehand responses indicated that the key to adequate training appeared to be frequent exposure to the procedures combined with good supervision and teaching. Among the 154 negative freehand responses, inadequate preparation was attributed to minimal exposure and being too rushed to take on responsibility for procedures; in some cases, fellows were not interested in procedures and did not feel they were relevant to their future practice.
Reflections on Fellowship
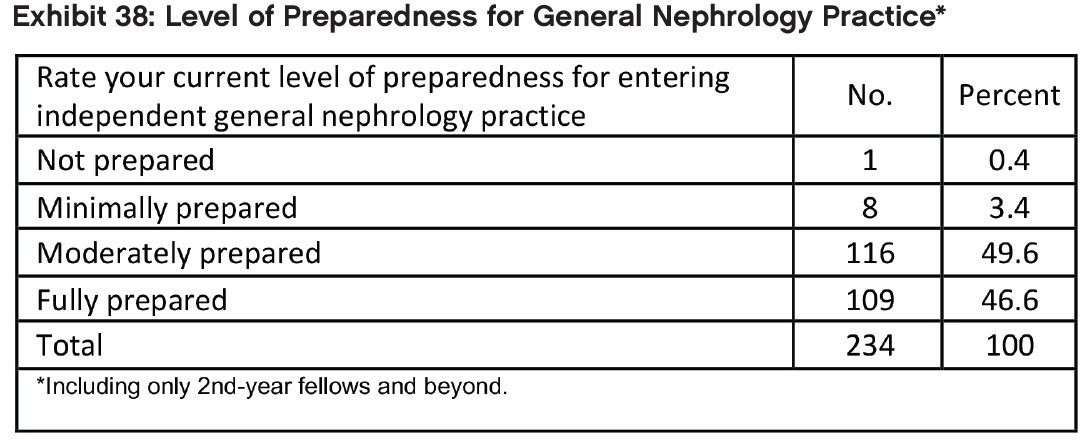
The vast majority of respondents (96.2%) in their second year and beyond rated their level of preparedness for general nephrology practice as “fully prepared” or “moderately prepared”, though less than half felt “fully prepared”. Only 3.8% felt either “minimally prepared” or “not prepared”.
Only a minority of respondents (46.0%) in their second year and beyond felt their work-life balance during fellowship had been good or very good. About 1 in 6 (16.9%) regarded their work-life balance as being poor or very poor.
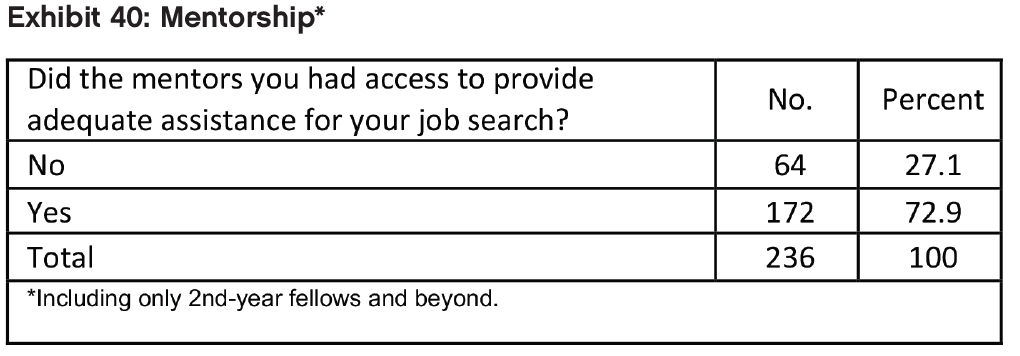
Almost three-quarters (72.9%) of respondents in their second year of fellowship and beyond reported they had benefited from adequate access to mentors in their job search.
When Did You Benefit Most/When Would You Have Benefited Most from Mentorship?
Among the 93 freehand responses provided there were many positive responses about mentors providing assistance and advice through every step of the job search process: providing contacts, making referrals, CV preparation, provision of letters of recommendation, help in finding job offers, developing interviewing skills, assessing opportunities and negotiating contracts. There were also many negative responses citing these same issues as those for which mentorship would have been appreciated but was not forthcoming. There was a strong sense from the positive respondents that their mentors cared deeply about the fellows’ future, and a sense from the negative respondents that their mentors did not.
Would Fellows Recommend Nephrology?
Despite their mixed assessments of the nephrology job market, a majority (71.8%) of fellows indicated they would recommend nephrology to current medical students and residents, the same as in 2016. However, IMGs were significantly less likely than USMGs to report that they would recommend the specialty to others (67.1% vs. 78.9%, respectively, p<0.05). We found no statistically significant difference between male and female fellows’ likelihood of recommending nephrology (p=0.72).
Fellows who said they would recommend nephrology to medical students and residents cited many of the same factors mentioned by 2015 and 2016 respondents as reasons for their positive assessments: the intellectual challenge/ interest of the field, variety of activities, and long-term patient relationships.
Fellows who said they would recommend nephrology to medical students and residents made the following comments to support their assessments:
Nephrology is a comprehensive true internal medicine subspecialty that gives you the ability to see patients in the outpatient setting, inpatient setting, dialysis units, and even transplant. That range is quite rare amongst IM subspecialties.
Nephrology is mentally challenging and requires indepth knowledge of pathophysiologic mechanisms in order to understand clinical manifestations of disease and provide treatment. In this sense it is extremely rewarding and I would recommend the field to any medical student or resident for this reason.
It’s great. I love kidneys. Opportunities in nephrology are burgeoning. There are myriad subspecialty opportunities and increasingly it’s easy to find nephrology jobs that have good work-life balance including part-time and nephrospitalist positions that can accommodate starting a family.
It’s a demanding but satisfying field of medicine which allows for personal/professional relationships with your pts as well as an acute/critical care dimension to inpt medicine.
I think Nephrology is a wonderful subspecialty and is unfortunately not popular. The physiology is dynamic and ever-changing; the pathology is always interesting and there’s always a patient who defies the odds. Nephrologist have the ability to work in multiple different environments and tailor their practice to their needs. I recommend and encourage it to all whom I rotate with and encourage them to participate in ASN Kidney STARs (I was a previous STAR and this really facilitated my interest).
A very exciting and interesting specialty, plenty of opportunities to build relationships with patients & families and be their advocate.
IT is a intellectually stimulating field that helps to have a better understanding of the pathology and thus in turn you can treat your patient as a whole and not just in your sub-specialty.
Nephrology presents diverse set of opportunities with regards to dialysis, transplant, interventional, and critical care. The field satisfies an intellectual curiosity, while allowing one to still remain a consummate Internist.
Love the renal physiology and derive extreme satisfaction from having specialized in such an intellectually stimulating field. However, the scarcity of job opportunities is a bummer and makes you question your choices. But, I guess you have to work extra hard to do something you love.
Good subspecialty if you enjoy continuity of care with patients across a wide spectrum of disease. Intellectually stimulating, will continue to use your internal medicine knowledge daily. Variety of practice settings (inpatient, critical care, outpatient clinic, dialysis, interventional).
Nephrology is a discipline that encompasses a great balance of diverse patient care settings–inpatient and outpatient, as well as stable illness and critical illness. The practice of nephrology is intellectually stimulating, as each patient necessitates an individualized care plan, based on the unique properties of their disease.
Nephrology is a field that combines complex pathophysiology with rewarding clinical experiences. Your patients rely on your expertise and come to trust you as they would a primary care physician. The community of dialysis techs, RN’s, NP’s, MD’s etc allow for a team based approach to patients with each bringing important skills to the table.
I chose nephrology due to the wide variety of patient care settings and the challenging work involved. I still find these aspects of nephrology satisfying. In my institution, however Internal Medicine has a higher starting salary which is disappointing after spending additional time in training and gaining expertise.
I would recommend it to students/residents who have a real interest in the job. It is not the most lucrative job in medicine and the patients can be difficult. However, you deal with such a wide variety of diseases in a wide variety of practice settings while providing a good opportunity to live a balanced life outside of work.
It makes you a holistic physician.
Fellows who said they would not recommend nephrology to medical students and residents also cited many of the same factors as in 2015 and 2016: the heavy workload, low compensation, difficult schedule relative to hospital medicine and other specialties, undervaluing of the specialty by other specialties, and lack of opportunities that support visas.
Fellows who said they would not recommend nephrology to medical students and residents made the following comments to support their assessments:
Although nephrology is intellectually stimulating and rewarding from a clinical aspect. The compensation is definitely on the lower side for starting salaries. It is only when a partnership is achieved that our salaries become somewhat competitive with other specialties. Medical directorships are being held onto by older associates too long, this contributes to the pay gap between newly graduated nephrologists and our more experienced colleagues. It seems that for the amount of hours nephrologist work including drive time, our work/ lifestyle does not compare to other specialties.
If you have a J1 visa -> No / Your possibility of work as a nephrologist are close to zero / if you want/can to go back to your country then yes * If you are a citizen or resident -> Yes
Field currently in flux, I would recommend it to the right individual, but there are some drawbacks currently. The hours are long and there are not enough staff support. I would not blanket discourage going to the field but I don’t think blind enthusiasm is the right way to go. trainees need to understand the drawbacks and advantages, although I think people tend to overstate the lack of jobs.
I explained earlier, nephrologist work very hard, sees patient in clinic, hospital, dialysis units, have to think carefully before every medical decision unlike cardiology/GI/pulmonary, have to travel multiple times a day from place to place and still paid the least amount despite providing best care to patients. So you know, I love nephrology but it ain’t worth doing all this hard work and getting no respect like all other medical community and paid poorly. I would rather be hospitalist and provide the same best care to my patients and enjoy free time/money.
I like nephrology, but unfortunately at the end if you have a family you found IM salary better than nephrology, for example I got offer for nephrology job in suburb of small city for 160k and another job of IM around the same area for 250k. the other thing I would like to be in academic place and I don’t mind the money for this place but because I need visa sponsor it almost impossible for me to get an academic job.
I myself like the specialty but not sure if I can convince residents and med students to take up Nephrology. The reimbursements/salaries are not great compared to several other specialties where lifestyle is comparable or where work load is similar. Compensation is not attractive while hours, patient volume and frequency of urgent/overnight calls is considerable. So this is not a lifestyle-friendly specialty with unattractive pay. Residents and students know this very well and have done their own research! So except for love for the subject it is hard to convince them. I think until the reimbursements improve things are not going to change for the current volume and complexity of care we provide.
Nephrology is an interesting intellectual specialty. However, the workload (both during fellowship and in private practice) takes away each enjoyable aspect from it. If you get 10 consults a day then even your quality of consults goes down. Dialysis patient are complicated and I feel like we are the primary care provider for them but we don’t get reimbursed for all that. The cut in the reimbursement in dialysis patients made things worse. Even if you are attending, you might get called at night anytime when you are on call and your regular days are too long so you don’t have lifestyle. I feel like we are being punished for choosing this specialty. We need a better system (perhaps mid-levels to cover night calls/ weekends or something to improve the lifestyle and the workload). Also, weekend calls are so ridiculously busy and it is the same in private practice (which also need a better system). I honestly don’t think the current system is even safe to the patients (with the workload, night calls and weekends calls). Perhaps we don’t need to see patients everyday or something needs to be done. Interventional Nephrology opportunities are very limited and there are less and less jobs for it
The specialty itself is intellectually interesting and engaging. The actual practice is disappointing. There seems to be very little respect for our discipline. The hours are long. The pay is not equivalent to other specialties with similar hours and required investment. The return is not great.
Unpredictable hours sacrificing life style, older nephrologist sees new fellows as cheaper labor and will provide little room for economic growth and if starting as solo, [it is] extremely difficult because the more experienced neph have been in the area for many years and won’t let the new Nephro expand easily
Among the medicine subspecialties, I would argue that Nephrology is ‘cerebral’ … those who are drawn to it have a passion for pathophysiology and enjoy critical thinking. The current unpopularity of nephrology is likely due to a paucity of job opportunities coupled with low wages. Starting salaries have remained stagnant despite rising workloads, especially in popular urban/ suburban areas. A current trend I have noted is of trained nephrologists practicing as hospitalists – citing better income and reduced workload as the reasons for doing so. I believe if one is willing to leave saturated areas, you can find a good location to practice as a nephrologist with an acceptable income and a decent lifestyle