Nephrology Training in the Time of COVID-19
The 2021 ASN Nephrology Fellow Survey
Nephrology Training Has Been Minimally Affected by the Pandemic
ASN Data Subcommittee
Kurtis A. Pivert, MS ![]()
Suzanne M. Boyle, MD, MSCE ![]()
Anna M. Burgner, MD, MEHP
Lili Chan, MD, MS ![]()
Susan Halbach, MD, MPH ![]()
Koyal Jain, MD, MPH, FASN ![]()
Benjamin Ko, MD ![]()
Hitesh H. Shah, MD, FASN ![]()
Joshua Waitzman, MD, PhD ![]()
Stephen M. Sozio, MD, MHS, MEHP, FASN ![]()
Disclaimers
This report’s findings are solely those of the authors and do not reflect the views of the Johns Hopkins University School of Medicine (JHUSOM) or the ASN Alliance for Kidney Health. Please provide your comments and feedback on this report to workforce@asn-online.org.
Suggested Citation
Pivert KA, Boyle S, Burgner AM, Chan L, Halbach SM, Jain K, Ko BS, Shah HH, Waitzman JS, Sozio SM. Nephrology Training in the Time of COVID-19: The 2021 ASN Nephrology Fellow Survey. Washington, DC: ASN Alliance for Kidney Health, 2021. Available at: https://data.asn-online.org/reports/fs_21.
Executive Summary
As the annual American Society of Nephrology (ASN) Nephrology Fellow Survey entered its eighth year, the project explored continued response to the COVID-19 pandemic and its impact on training and careers of fellows. This year, 501 of the 920 current adult, pediatric, and adult/pediatric nephrology fellows who received the survey participated, for a gross response rate of 54.6% (the highest response in the survey’s 8-year history). A majority of respondents were international medical graduates (IMGs, 54%), male (56%), white (36%) or South Asian (32%), and in their second year of fellowship (51%).
Our analysis of the 2021 ASN Nephrology Fellow Survey revealed five key insights into how nephrology fellows are navigating COVID-19 and pandemic-related changes to training and providing patient care.
Nephrology Training Has Been Minimally Affected by the Pandemic
A majority (83%) believed their training programs had successfully maintained their education even though nephrology conferences, which quickly pivoted to video in the initial days of the pandemic, remain online for 64% of respondents. Fellows’ sense of community, breadth of clinical exposures, ability to advance their research, and relationships with mentors were likewise highly ranked. Most participants (87%) believed they would be prepared for independent practice upon graduation.
Telehealth Adoption Continues
Telehealth uptake remained strong into the pandemic’s second year with 83% of fellow respondents seeing some patients virtually in the outpatient setting, and 36% using telehealth for some cases on inpatient wards.
COVID-19 is Challenging Fellows’ Well-Being
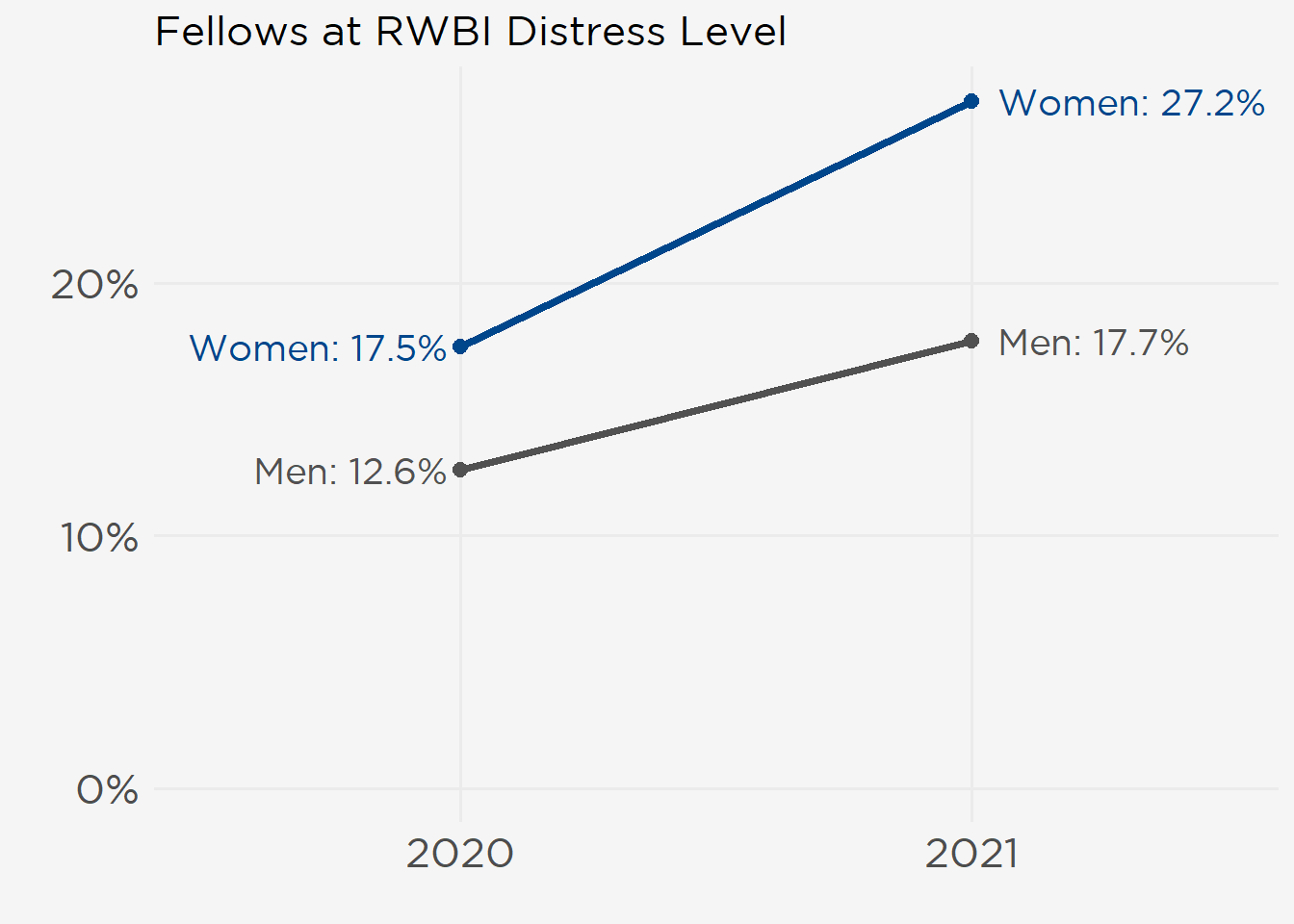
As the pandemic continues more fellows are vulnerable for burnout and poor mental quality of life (QOL). The proportion of fellows at risk for distress as measured by the Resident Well-Being Index (RWBI) increased 47% between 2020 (15% of respondents at risk) and 2021 (22% of respondents). This year more women met the distress threshold than men (55 women, 27%; 46 men, 18%) (see figure at right).
Employment Perceptions Improved Yet Local Job Market Remains Tight
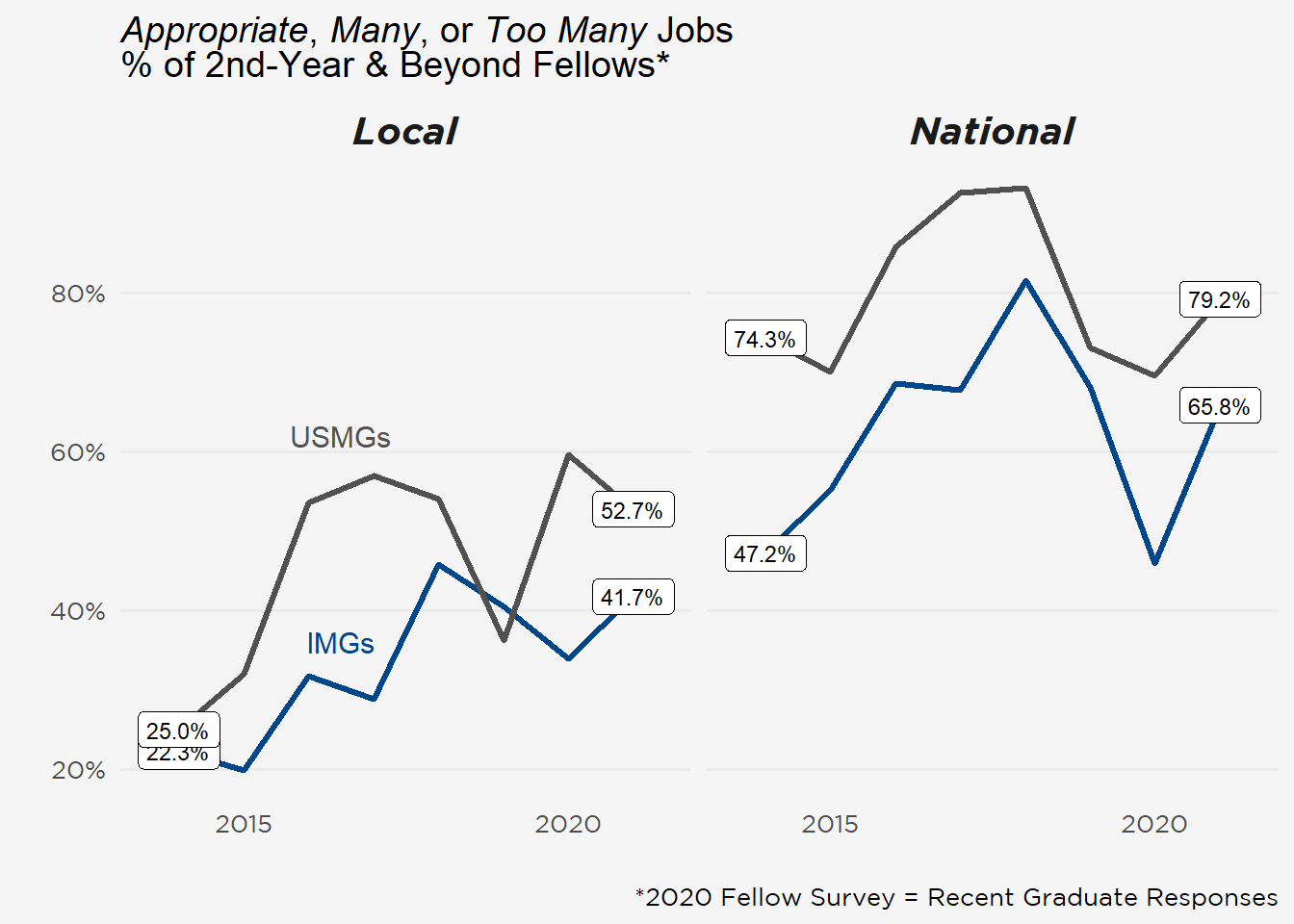
Less than half (47%) of fellows in their second or greater year of training perceived an “Appropriate,” “Too Many,” or “Far Too Many” number of local jobs (within 50 miles of their fellowship) despite steady improvements since the survey started in 2014 (see figure below). While national market impressions have been more positive, they’ve varied in a narrower range. Clinical nephrology (91%), joint nephrology–other specialty (12%), and research (11%) positions were the top jobs sought after fellowship.
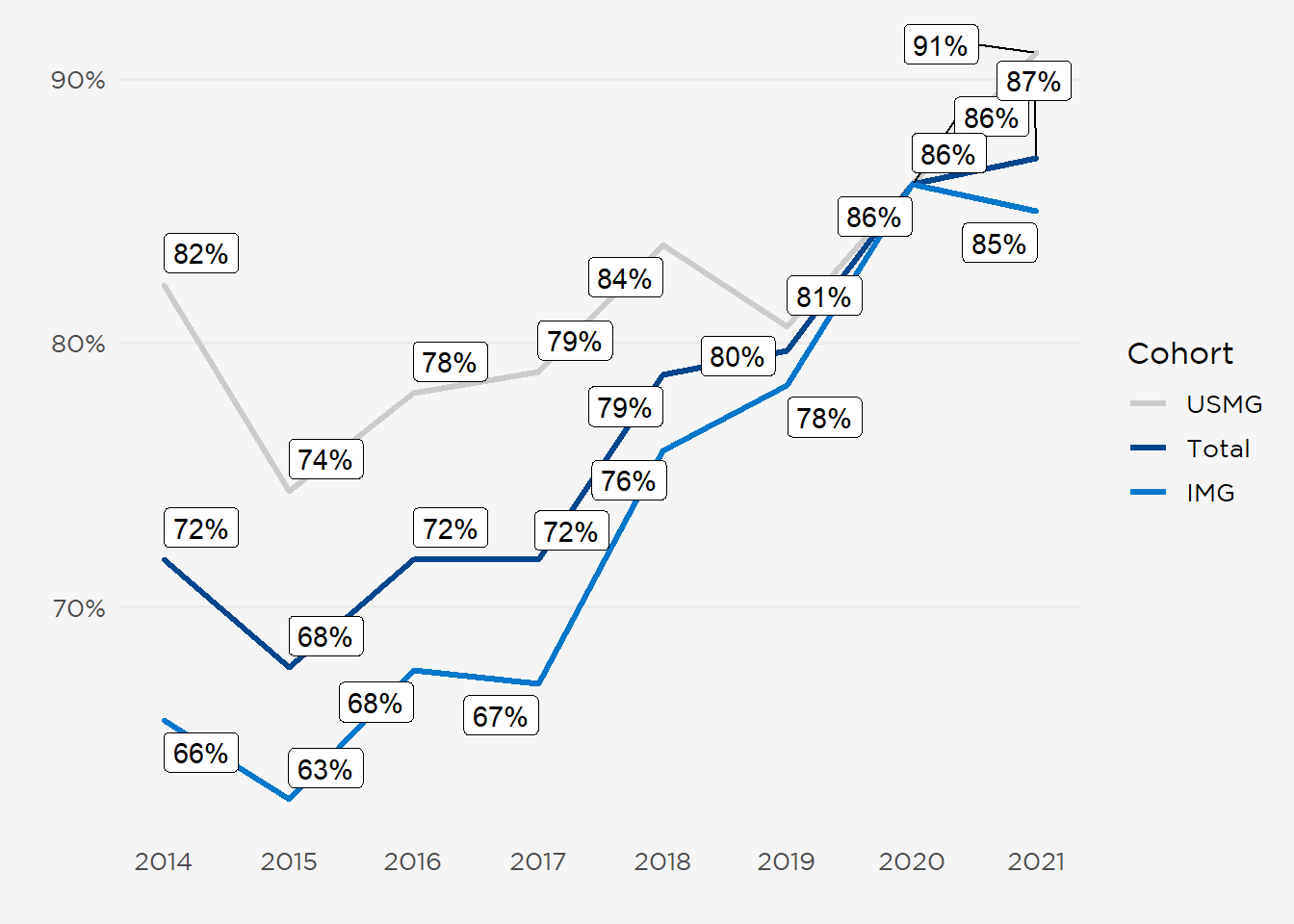
Most Fellows Recommend Nephrology
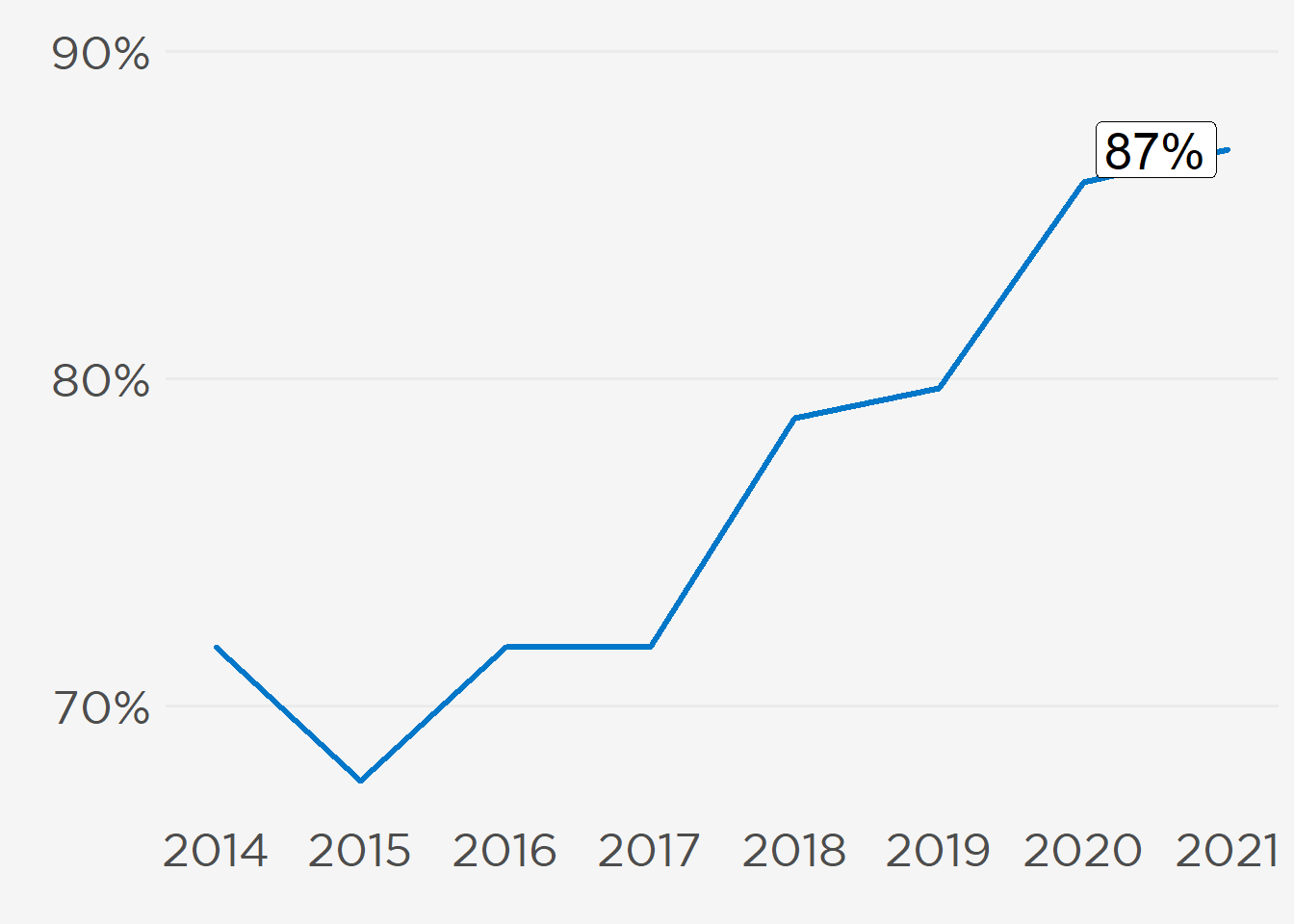
A record 87% of fellow participants (see figure at right) would recommend nephrology to medical students and residents, including 85% of international medical graduates (IMGs) and 91% of US medical graduates (USMGs). Longitudinal patient relationships, case variety, and providing public health to underserved communities were among the reasons cited for recommending the specialty.
I. Sustaining Education Through a Pandemic
COVID-19 has altered not only patient care but also medical education. Nephrology conferences, which quickly migrated to video in early 2020, remained exclusively online for two-thirds of fellows (65%) (Figure 1). Telehealth retained traction for outpatient encounters (384 respondents seeing some patients virtually) and, to a lesser extent, inpatient visits (164 respondents using telehealth for some encounters). As COVID-19 protocols evolved from 2020 (when many trainees stopped in-person evaluations) fellows returned to all clinical settings with only a few indicating rounding was still suspended due to the pandemic (\(\le\) 13 respondents) (Table 1).
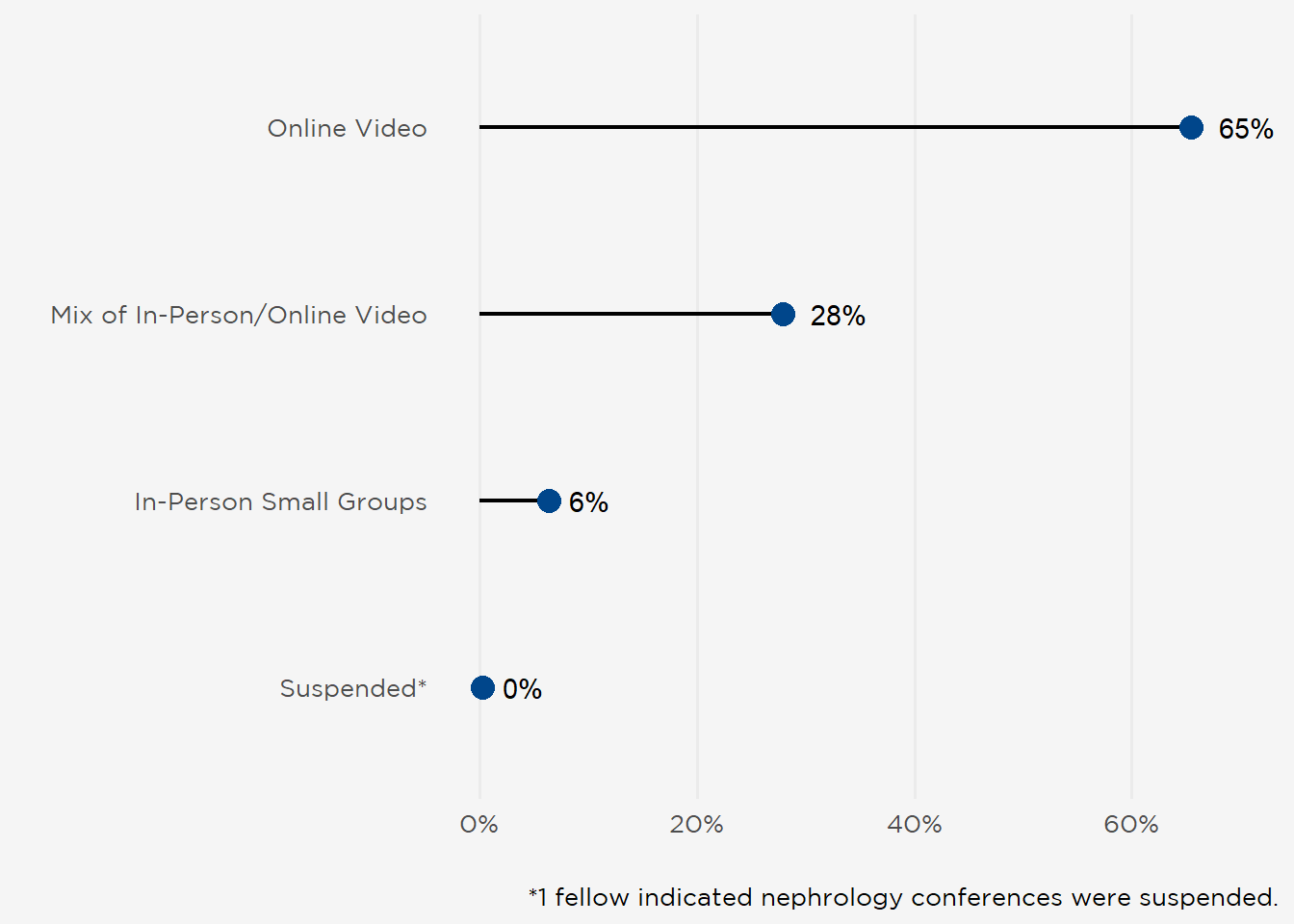
Table 1: Frequency of Telehealth Use by Clinical Setting.
| Telehealth Usage | Inpatient Consults | Outpatient Consults | Outpatient Dialysis |
|---|---|---|---|
| All Patients Telehealth | 1 | 14 | 1 |
| Some Patients Telehealth | 164 | 377 | 84 |
| No Patients Telehealth | 212 | 48 | 237 |
| On Hold Since Pandemic | 4 | 5 | 13 |
| Not Applicable/Have Not Started | 78 | 15 | 124 |
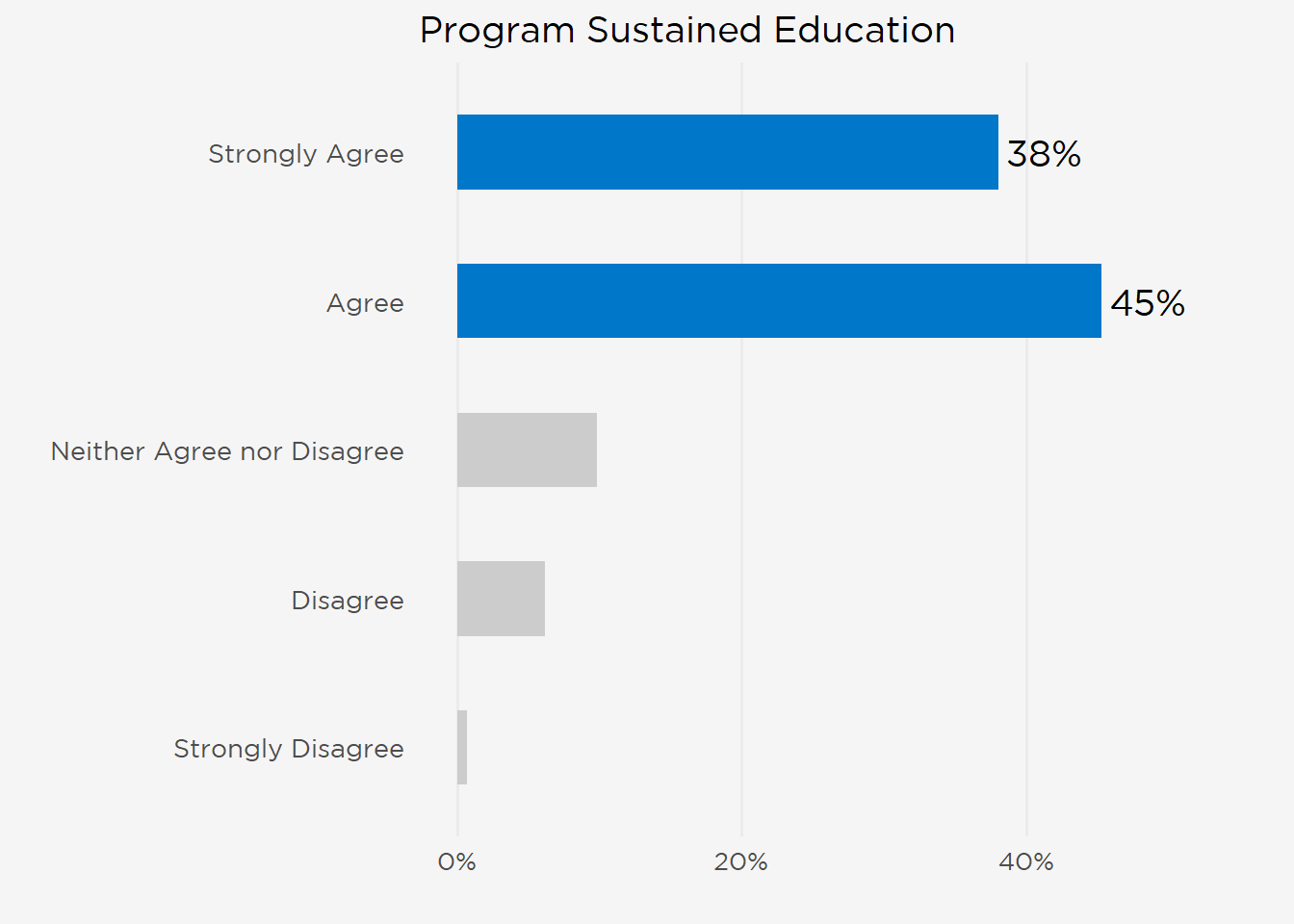
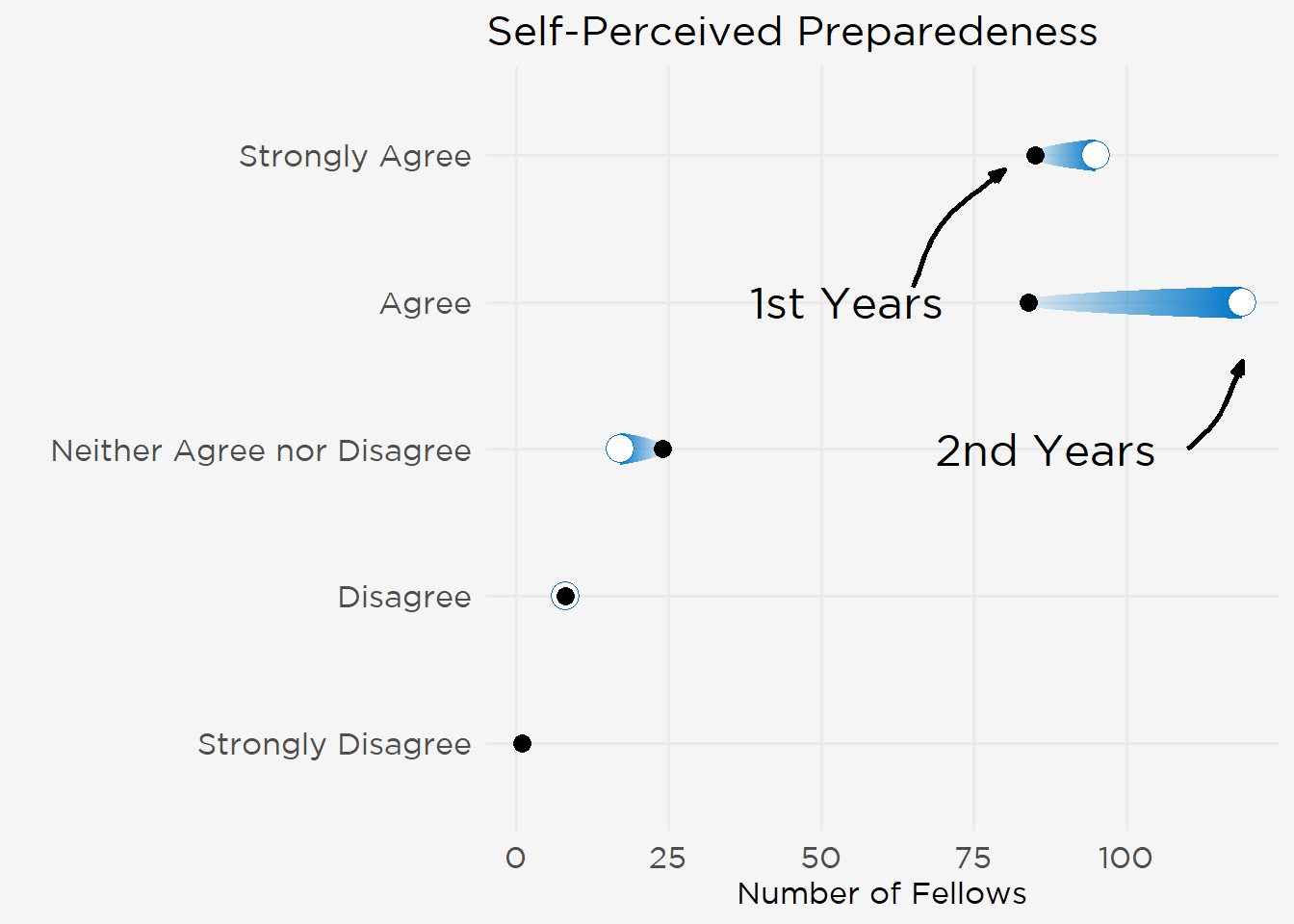
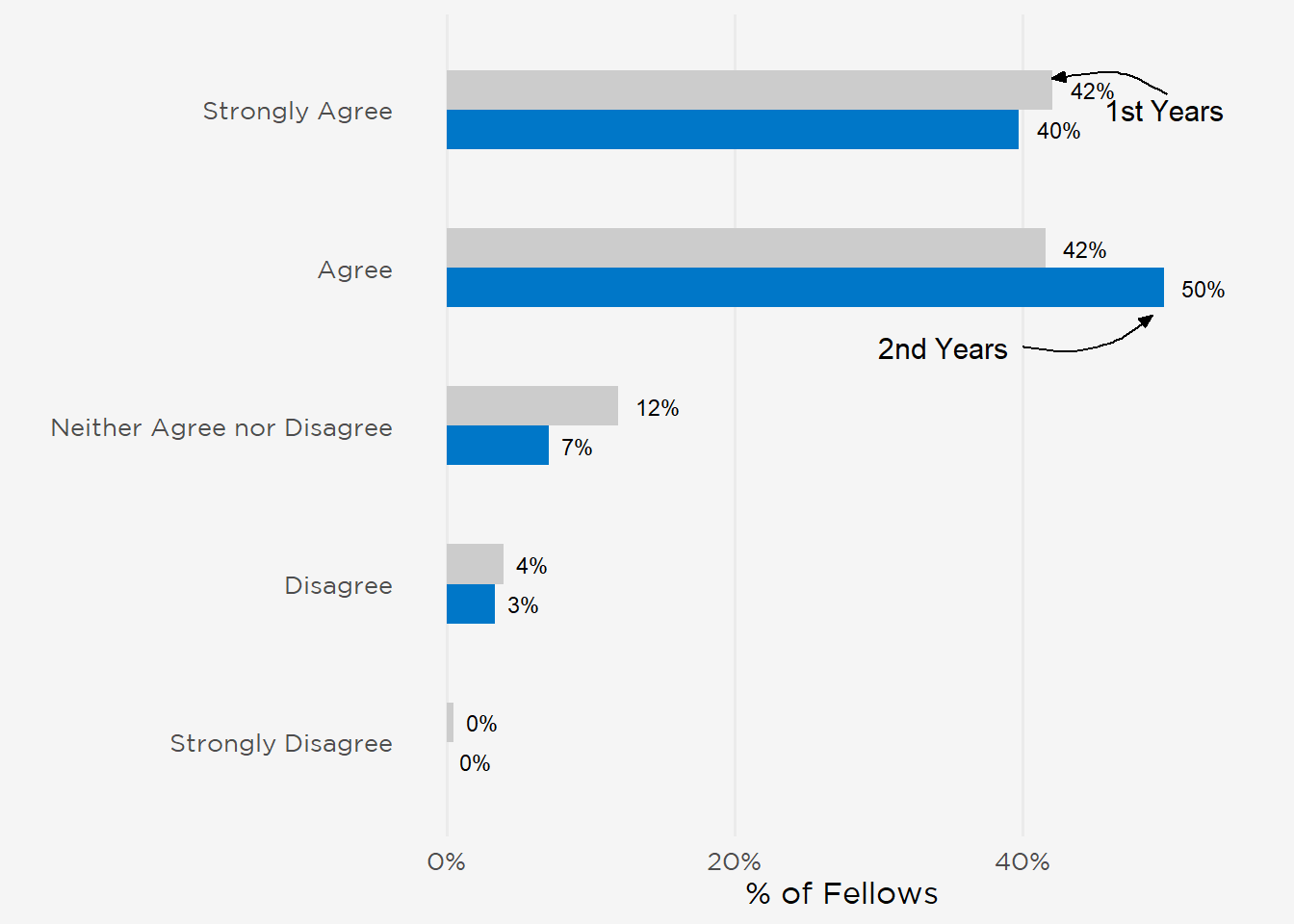
Despite these pandemic-driven changes, participants were generally positive in assessing their fellowship training. Most rated the quality of instruction as either excellent (47%) or good (36%), and 83% agreed their programs had successfully sustained their education through the pandemic. This carried over to fellows’ self-assessments of their preparedness for independent practice, 87% of whom agreed they would be prepared upon graduation (“Strongly Agree” 41%, “Agree” 46%) (Figure 2).
Figure 2: Self-Assessment of Preparedness for Independent Practice.
Other aspects of the training environment—fellows’ sense of community, breadth of clinical exposures, ability to advance their research, and relationships with mentors—were likewise ranked highly (range 76%–95% combined “Strongly Agree” and “Agree”). However, fewer fellows believed they had adequate board preparation time (70% combined “Strongly Agree” and “Agree”), and fewer participants expressed satisfaction with their work-life balance (59%) and contract negotiation advice they received (51%) (Figure 3).
Figure 3: Fellow Opinions on Aspects of Their Fellowship Programs.
II. Fellow Well-Being in a Pandemic
Nephrology fellow well-being was a principal focus of this year’s survey. Participants’ risk for psychological distress was measured using the Resident Well-Being Index (RWBI), a validated instrument that quantifies risk for a spectrum of outcomes, including burnout, medical errors, and suicidal ideation (Drybye et al. http://dx.doi.org/10.4300/jgme-d-13-00117.1). An RWBI score at or above the distress threshold (RWBI score \(\geq\) 5; score range 0–7) is associated with a three-fold higher risk of poor mental QOL and a four-fold higher risk of burnout.
One-hundred-one participants (22%) met the distress threshold out of the 463 adult, pediatric, and adult/pediatric fellows completing the 7-question RWBI instrument. Although the survey was conducted prior to the emergence of the Delta variant during a relative ebb in overall COVID-19 cases (between May 4 and June 1, 2021) a greater share of participants (22%) met the distress threshold (RWBI \(\geq\) 5) than a year ago (15% of fellows and recent graduates in August 2020). High RWBI scores (\(\geq\) 5) were more prevalent among USMGs, women, adult fellows, and 1st-year adult fellows (Table 2).
Table 2: Characteristics of Fellows at Risk of Distress.
| Fellows Meeting RWBI Distress Threshold* | ||
| Number | Percent† | |
|---|---|---|
| Medical School | ||
| USMG | 54 | 24% |
| IMG | 47 | 19% |
| Sex | ||
| Woman | 55 | 27% |
| Man | 46 | 18% |
| Fellowship | ||
| Adult | 96 | 22% |
| Pediatric | 4 | 15% |
| Adult Fellow Year | ||
| 1st | 51 | 26% |
| 2nd | 40 | 18% |
| *IMG = international medical graduate; RWBI = Resident Well-Being Index; USMG = United States Medical Graduate. †Percentages are based on number completing RWBI. | ||
III. The 2021 Job Market
The marketplace for private practice positions can often be opaque, which is why fellow assessments of local and national employment conditions are useful leading indicators of nephrologist demand. Availability of jobs within a 50-mile radius of fellows’ training program was hypothesized to be a more sensitive metric because post-fellowship employment opportunities often factor into where fellows choose to train. This year, 45% of respondents planned on working in the same state as their fellowship, 35% in the same city, and 16% at their program’s institution. Only 3% (16 fellows) planned on returning to their home countries after completing their training (Figure 4).
Figure 4: Where do you plan on working after completing your fellowship?
Fellows in their second year of fellowship or beyond (N=225) saw a tight local job market, with 53% indicating there were “too few” or “far too few” job opportunities within a 50-mile radius of their institution (Figure 5). Given many nephrology fellowships are situated in major metropolitan areas across the Northeast and South Census Regions, with 58% of participants within these two regions, it was hypothesized that program location may influence these views. However, analyses of local job market perceptions aggregated by either Census Region and the granular Census Division were not statistically significant (p = 0.51 and p = 0.72, respectively, Kruskal-Wallis rank sum test). Although fewer IMG fellows saw an at least appropriate number of local jobs (combined “appropriate,” “too many,” and “far too many”) (42% vs 53% of USMGs), differences in perceptions based on USMG vs IMG status also were not statistically significant (p = 0.067, Wilcoxon rank sum test).
Figure 5: Perceived Number of Job Opportunities Within 50-Mile Radius of Fellowship.
Nationally, 72% of 2nd-year and beyond fellows (N=218) believed there were an at least appropriate number of openings (Figure 6), although USMGs were again more sanguine than their IMG colleagues (79% vs 66%, respectively, reporting at least an appropriate number of jobs in the U.S. overall; data not shown). Differences in national perceptions between IMGs and USMGs approached statistical significance (p = 0.055, Wilcoxon rank sum test), yet did not differ significantly by Census Region or Division (p = 0.38 and p = 0.34, respectively, Kruskal-Wallis rank sum test). One-quarter of participants were unaware of job availability in either the local (26%) or national (27%) market.
Figure 6: Perceived Number of Job Opportunities Nationally.
Job Search
Most of the 173 fellows (157 adult, 14, pediatric, and 2 adult/pediatric) who had started their job search were seeking clinical nephrology positions (157 fellows). Joint nephrology/other subspecialty (21 fellows), research (19), general (non-nephrology) hospital medicine (16), and government (10) rounded out the top 5 job types sought in 2021.
Although IMGs applied for more jobs than USMGs (median 3 vs 2 applications, respectively) both groups received a similar number of employment offers (median 2 offers). As in previous surveys, IMG fellows were more likely to experience difficulty finding a position they considered satisfactory than USMGs (44% vs 19% experiencing difficulty, respectively). An undersupply of jobs providing visa sponsorship was the most frequently cited cause of difficulty for IMGs (58% of respondents) along with few opportunities in their desired location (56%) and practice setting (54%). Of note, just 57% of participants (82 fellows) were satisfied with their faculty’s job search advice.
First Post-Fellowship Position
At the time of survey completion 145 fellows had been offered a position—125 had accepted and 20 were still searching for another job. The remaining 28 fellows had not yet received an offer. Fellows starting practice in 2021 were:
- Entering Clinical Nephrology: Nearly all of those who accepted a position (91%, 114 fellows) were starting practice in clinical nephrology, with 4 (3%) starting a joint nephrology/other subspecialty position, 3 entering general hospital medicine (2%), and 1 (1%) each in joint clinical/research, another subspecialty, and nephrology industry positions.
- Working in Urban Areas: Most fellows were starting jobs in large cities (75%) and suburban areas (10%), with only 14% employed in either small city or rural settings. Although 9 IMG respondents obtained a visa waiver by accepting a position in rural or medically underserved areas, 2 IMGs had accepted a position outside the U.S.
- Responsible for Inpatient, Outpatient CKD, and Dialysis Care: Teaching (35%), apheresis (20%), research (18%) and dialysis medical directorship (17%) were the most common additional practice areas (Table 3).
Table 3: Primary Job Responsibilities in First Post-Fellowship Job.
| Primary Responsibilities | N* | Percent |
|---|---|---|
| Inpatient care | 118 | 95% |
| Outpatient clinic—CKD | 103 | 83% |
| Outpatient dialysis | 94 | 76% |
| Education | 43 | 35% |
| Apheresis | 25 | 20% |
| Clinical research | 22 | 18% |
| Medical directorship with a dialysis provider | 21 | 17% |
| Kidney biopsy | 17 | 14% |
| Dialysis catheter placement | 17 | 14% |
| Outpatient clinic—Transplant | 12 | 10% |
| Joint venture with a dialysis provider | 11 | 9% |
| Interventional nephrology | 8 | 6% |
| Basic science research | 1 | 1% |
| Other | 1 | 1% |
| *N = 124 Fellow Respondents | ||
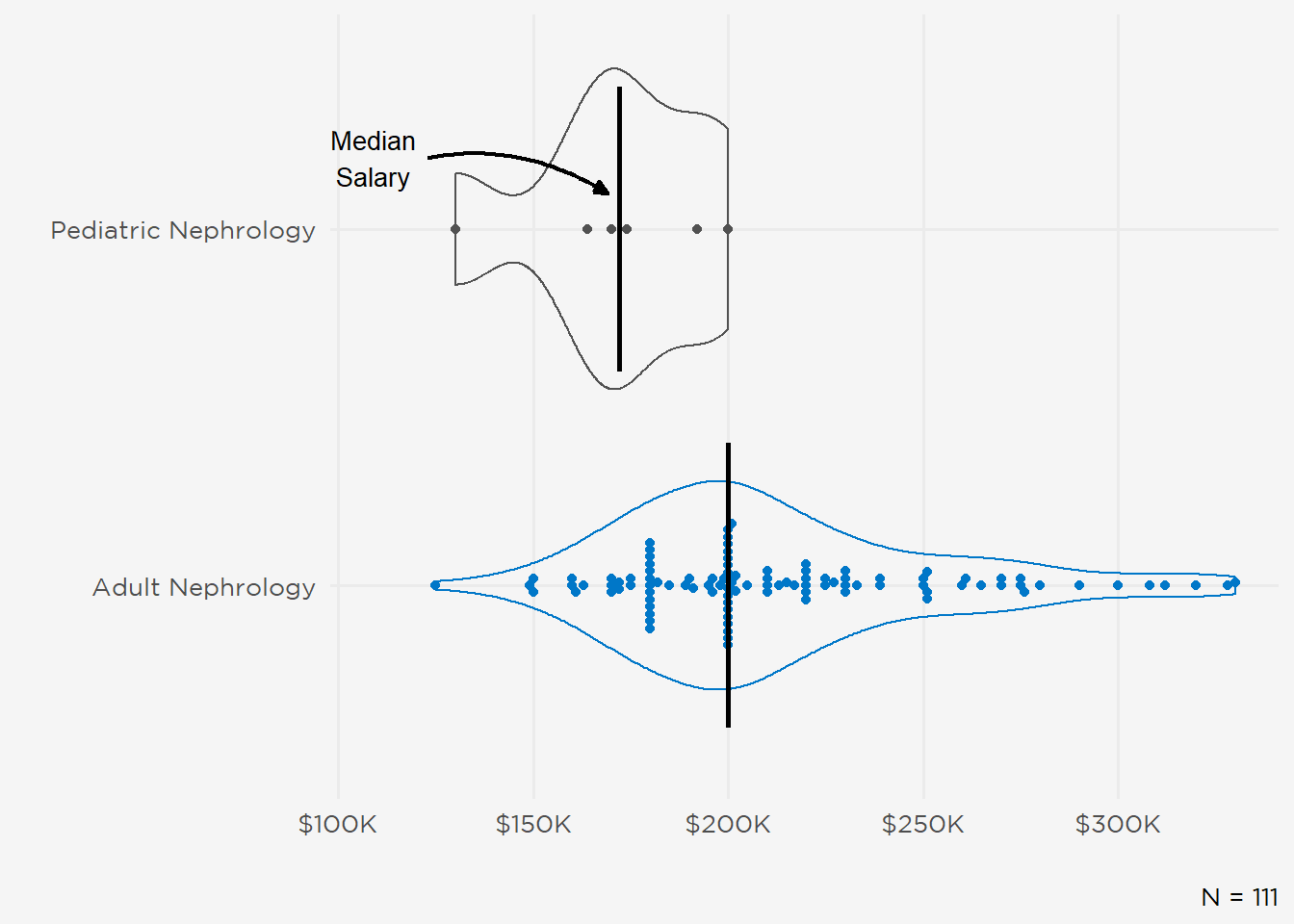
Median starting base salary was $200,000 with an interquartile range (IQR) of $47,800. IMGs reported slightly higher base pay (median $202,000; IQR $71,000) than USMGs (median $200,000; IQR $40,000) (Figure 7). However, there were no gender differences in median base compensation (median $200,000 for both women and men) (Figure 8). Starting salaries for pediatric nephrologists were lower than adult nephrologists (median $172,000 vs $200,000) (Figure 9). One-half of newly employed fellows expressed satisfaction with their starting salaries (extremely satisfied, 18%; somewhat satisfied, 38%). Twenty-two percent were neutral (neither satisfied nor dissatisfied) and another 22% were dissatisfied (17% somewhat, 5% extremely dissatisfied). Note several zero outliers (the default value in the survey instrument) were censored.
Figure 7: Expected Base Salary for IMG vs USMG Respondents.
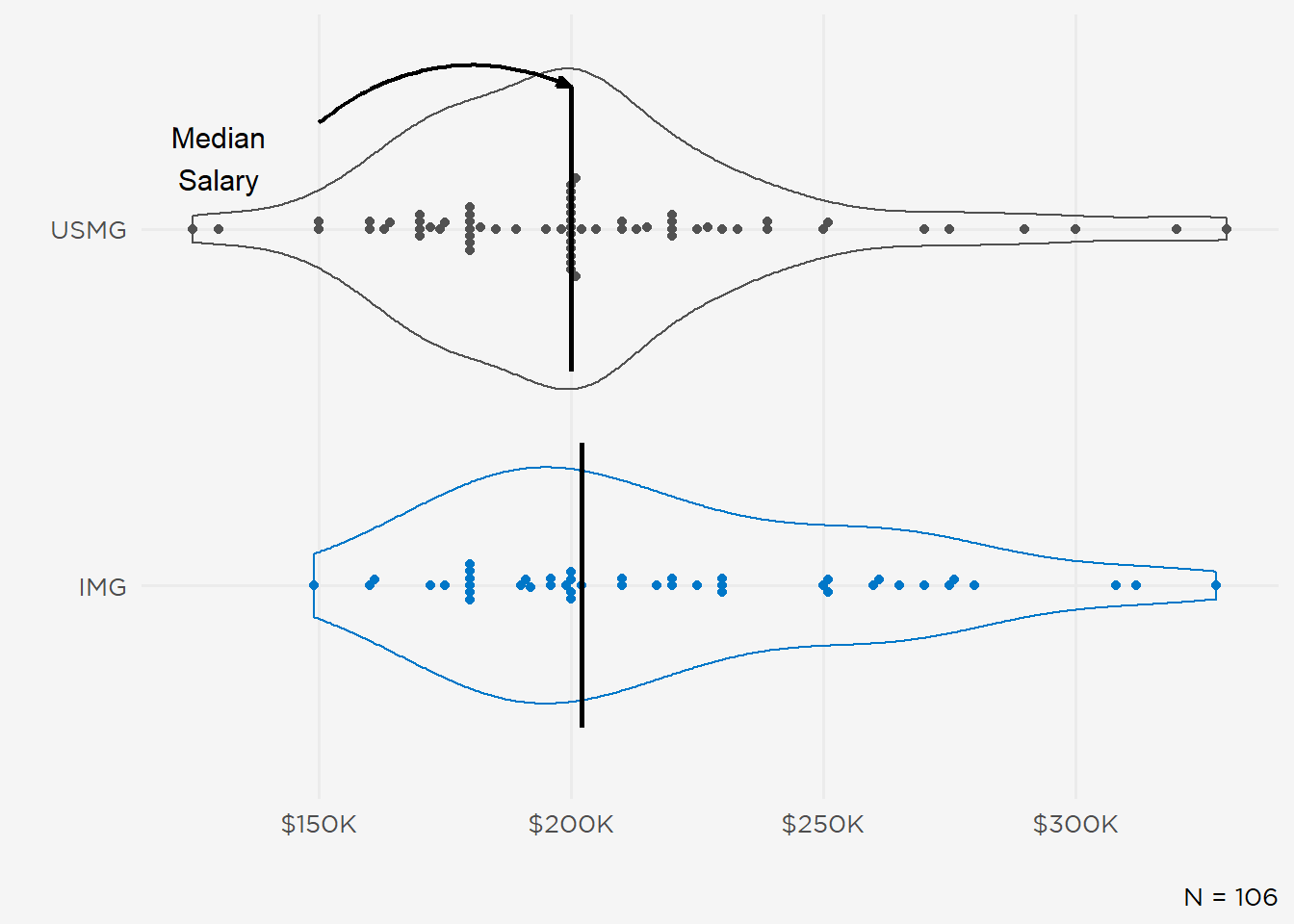
Figure 8: Expected Base Salary by Gender.
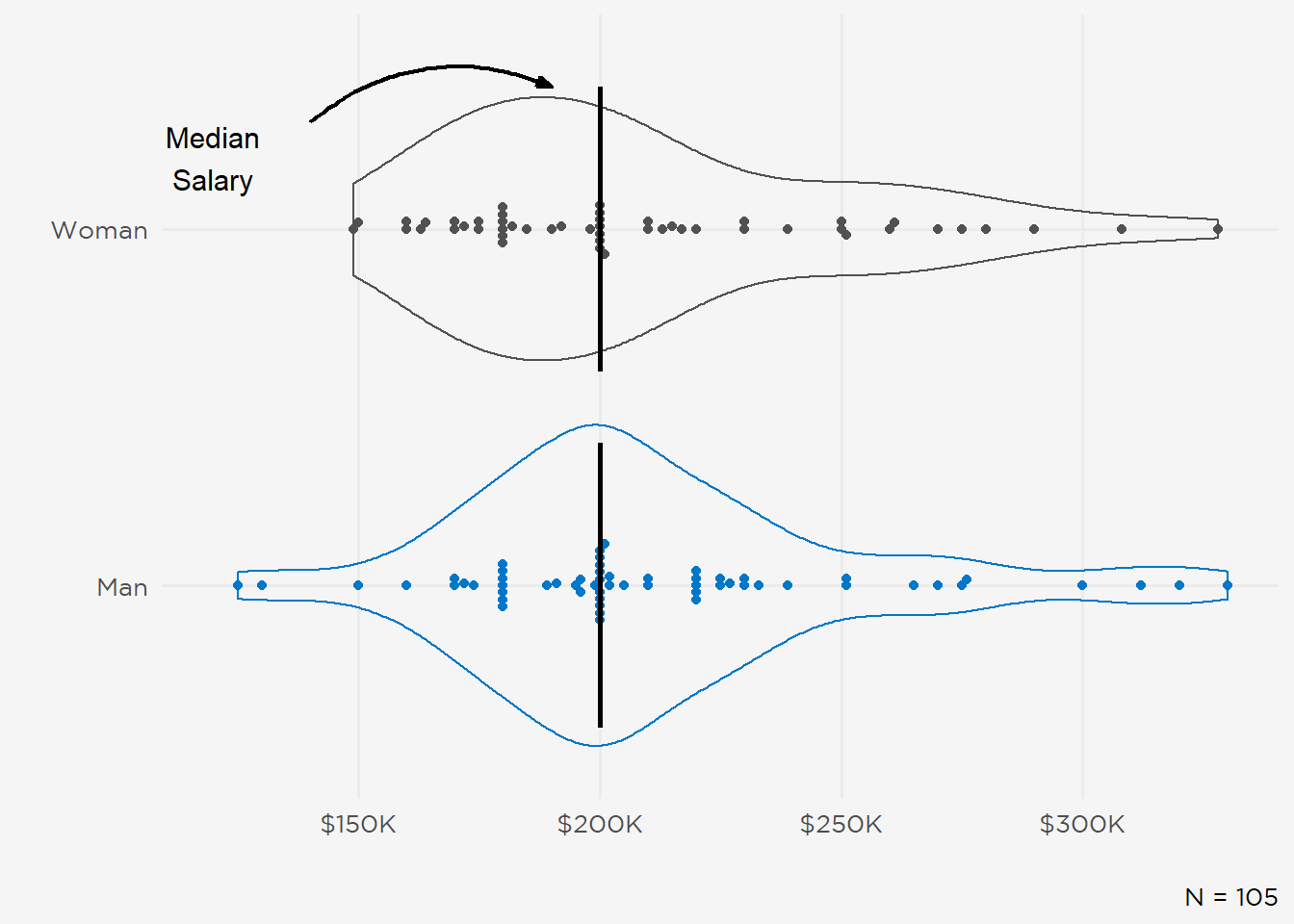
Figure 9: Expected Base Salary by Fellowship.
Employment Incentives
Income guarantees, maintenance of certification (MOC) and continuing medical education (CME) support, signing bonuses, and career development resources were the most common incentives (each reported in aggregate by \(\geq\) 34 respondents) (Figure 10). Additionally, 57 fellows received incentive income (median $10,000), with higher levels reported by USMGs and men (median $15,000 for USMGs and men; median $10,000 for IMGs and women). Overall, incentives were a key factor in determining whether fellows accepted a job offer, with 47% indicating they were “Very” or “Extremely” important.
Important Factors When Evaluating Job Offers
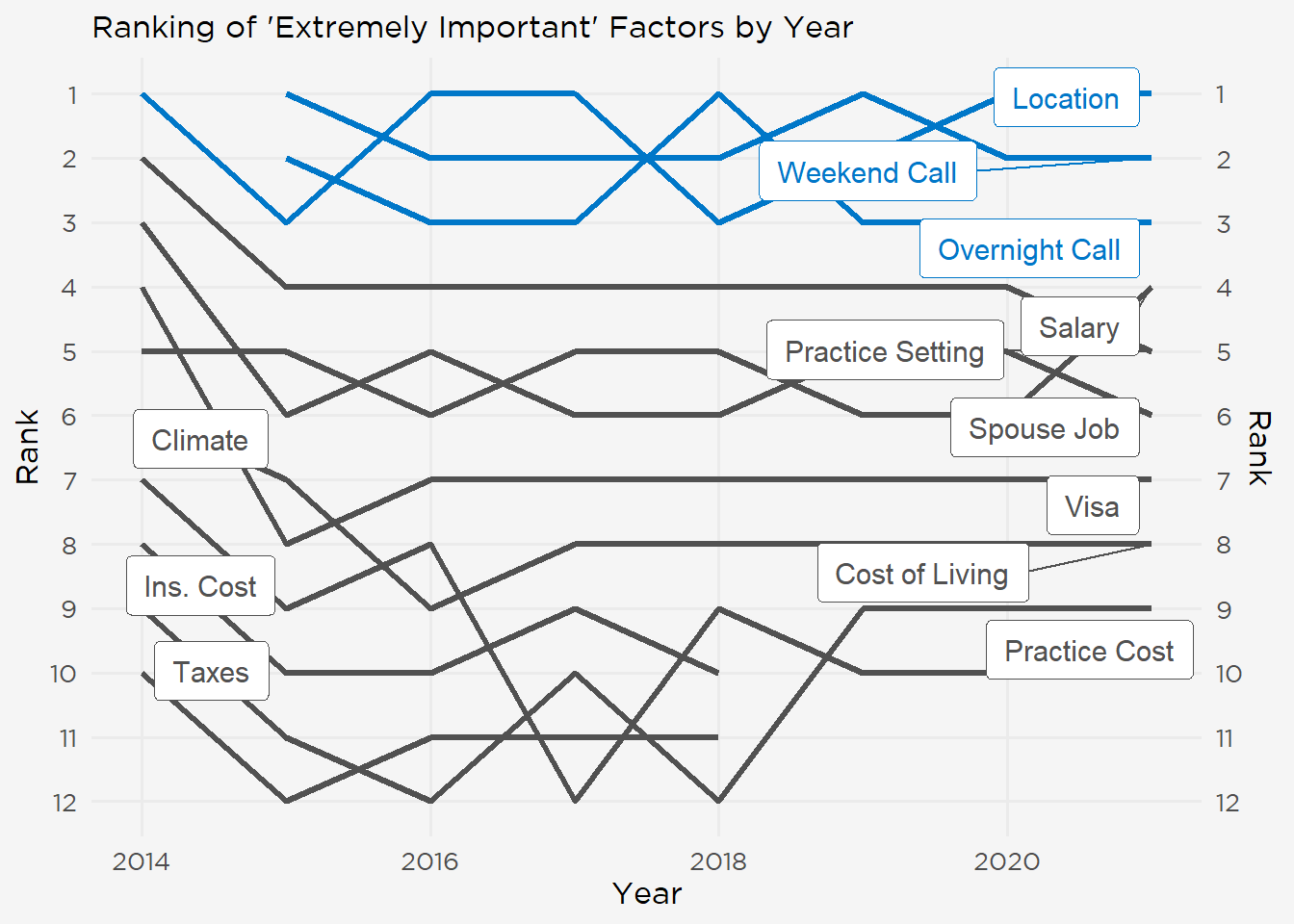
Since the fellow survey started in 2014, job location has been among the factors fellows rated “Extremely Important” in weighing employment offers, with call schedule (both weekend and overnight, added in the 2015 survey) rounding out the top 3 (Figure 11). In comparison, salary has wavered between fourth and fifth position over the same time period. Consistently lower-rated factors (e.g., climate or taxes) have been removed from the survey.
Figure 10: Employment Incentives Received by Fellow Respondents.
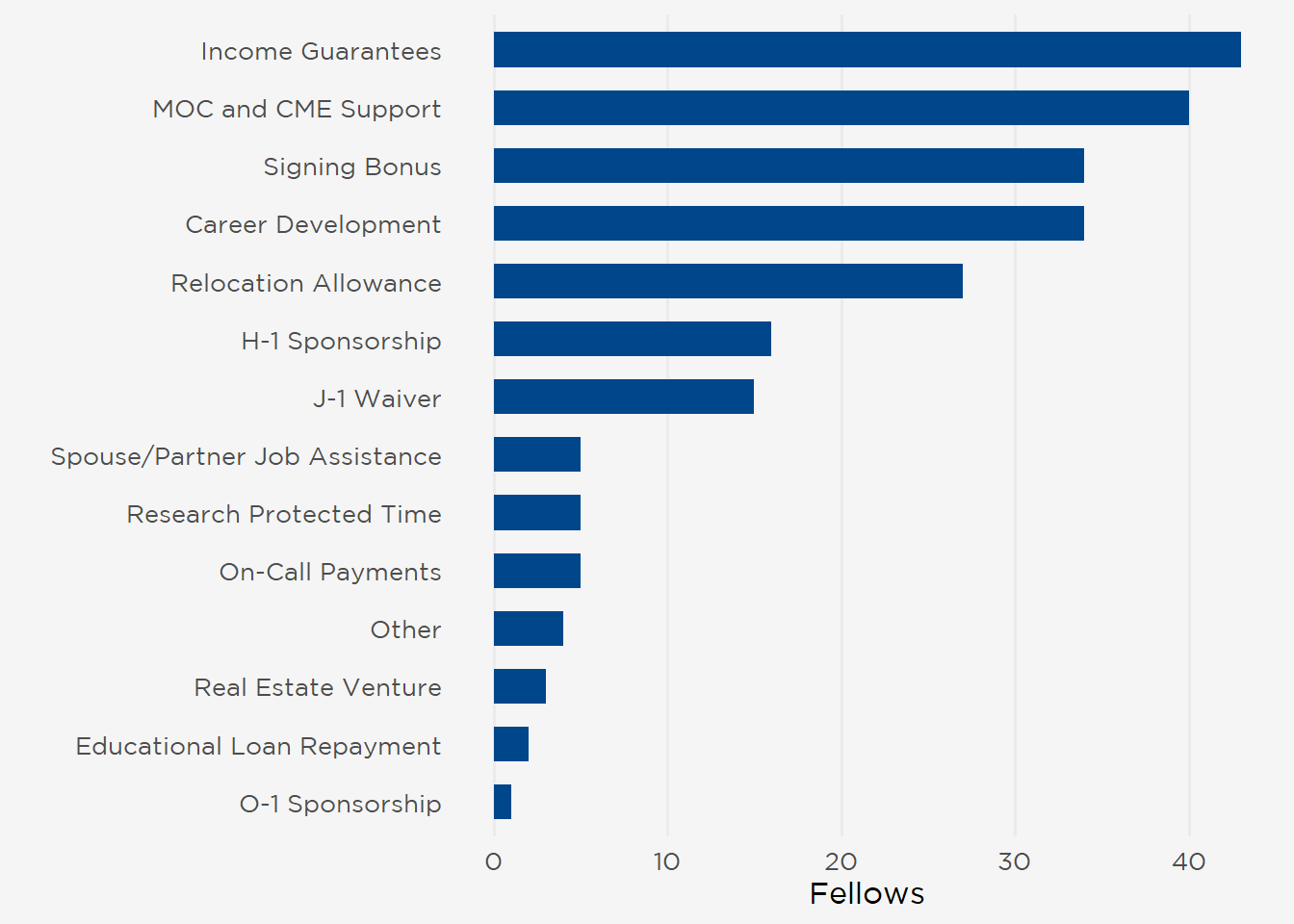
Figure 11: Important Factors in Job Search 2014–2021.
IV. Nephrology Perceptions and Motivations
Training in the middle of a global pandemic did not diminish fellows’ views on their chosen specialty. A record 87% of participants would recommend nephrology to medical students and residents (85% of IMGs and 91% of USMGs) (Figure 12). Several themes emerged in the free text responses explaining why fellows would or would not encourage others to pursue nephrology.
Figure 12: Proportion of Fellows Recommending Nephrology.
Not Recommend Nephrology—Themes
Compensation—Starting salary has consistently been cited as a detracting factor since the fellows survey’s inception in 2014.
Too much work for too little payment and recognition.
U.S. Healthcare Payment systems do not respect our time and effort since we do not perform any expensive therapeutic procedures. Historically, nephrology lost out on controlling dialysis in a more ethical and responsible manner by relinquishing control to the U.S. government. Moving forward, with greater advocacy, there’s hope that we can reclaim more respect as reflected by adequate compensation for our time and effort.
Not paid enough for the amount of work done (call, windshield time).
Difficulty of Fellowship and Practice—The complexities of renal physiology and broad range of nephrology practice were among the new factors cited this year.
The field is complex, the training is difficult, the pay is abysmal.
Lifestyle and Work-Life Balance—The stereotype of nephrologists having busy work schedules and poor work-life balance is another common explanation for avoiding the subspecialty, but this is now being associated with an increase in stress among fellows during the pandemic.
Because of the level of burn out among fellows.
People I see currently working in nephrology don’t seem happy. They work many hours and remuneration does not match what they do nor what it is required to know to practice nephrology. I don’t regret going into nephrology and I enjoy learning about it and practicing as a fellow but it seems that many nephrologists are stuck working many hours to make a living and survive.
Lack of Therapeutics—This year, more participants indicated the paucity of viable alternatives to renal replacement as a disincentive to practicing nephrology.
There are no interventions or treatments that we can offer to the patients. Everyday inpatient or clinic visit is just monotonous and involves a lot of “continue to monitor.” Lifestyle is horrible driving around town asking hospitalists for consults and payments are lower that any other specialty. Most of the things that you learn in nephrology have no practical implications. Whereas other specialties have moved on to very advanced practices nephrology is stuck in “spinning urine.”
No Respect/Cheap Labor—Undervaluing of nephrology by other specialists has been a consistent complaint among those not recommending the specialty.
Compensation is very low for the amount of work you put into it, not respected by other specialties especially critical care.
Training is not what is offered, we are just cheap labor. the main commitment is to get the work and consults done; education is not a priority when you have overwhelming amount of work.
Very hard specialty, very time consuming, not enough respect, hard to find a job, at risk of being abused during employment.
Fuzzy area of competence overlapping with other specialties.
Recommend Nephrology—Themes
Nephrology is Pure Medicine—Fellows continue to view nephrologists as the ultimate internists.
It encompasses almost every aspect of medicine. Inpatient, outpatient, critical care, pathology, microscopy. It allows you to assess, diagnose and treat starting with bedside care to benchside microscopy/pathology to final diagnosis and treatment.
It is another form of holistic medicine that incorporates all subspecialties allowing us to maintain contact with general medicine. Additionally the knowledge we gain with practicing nephrology is at another level compared to basic training vs other subspecialties. Also, some of the most interesting diagnostic dilemmas stem out of Nephrology and often the unifying diagnoses are made by Nephrology which makes it very exciting.
Its very satisfying. Knowing the pathophysiology helps you appreciate the degree of illness and render appropriate care. Nephrology is one of the few subspecialties which gives you this opportunity.
Longitudinal Relationships—Long-term patient relationships are repeatedly noted as a positive motivating factor.
Patient care (love that it is longitudinal), interesting and variable cases, rising interest in society for kidney care.
Subspecialization and Variety—The mix of practice settings and patients available in nephrology is a strong differentiator for fellows, for both those who would and would not recommend the specialty.
I love nephrology because I will be able to help many patients with kidney disease to avoid/postpone having ESKD, HTN, mineral bone disease and also help to those who already have ESKD with HD and transplant. Also a good communication with other specialties like ICU, rheumatologists, and cardiology.
High needs subspeciality, good case mix, ability to work inpatient/outpatient. Lifestyle generally seems better overall however I do explain to interested residents that balance of inpatient/outpatient/dialysis and home life varies greatly from region to region.
Interesting and Intellectually Challenging—Fellows recommending nephrology point to its complexity and challenges as stoking their passion for the field.
It’s the best. People get turned off by dialysis (not sure why? I think they don’t like the idea of it or something, maybe they see non compliant patients in the hospital and that is all they know. It’s actually a cool way of having significant continuity and building relationships) and think that we don’t do anything else. We do so much more! So much cool electrolyte stuff, diagnostic work up for AKI, treatment of auto immune diseases, etc. and our field is advancing! Trials are coming out all the time. It’s exciting and fun to be a nephrologist.
Providing Public Health to Underserved Communities—Another emerging motivation for nephrology is its intersection with public health and serving minoritized and underserved populations, groups with higher risk of developing kidney diseases.
Challenging field with interesting subjects of electrolytes, volume, and immunology. Great co-workers and mentors. Long term patient relationships with underserved population.
The community is engaging and brilliant, lots of room to improve and make a difference in the realm of public health.
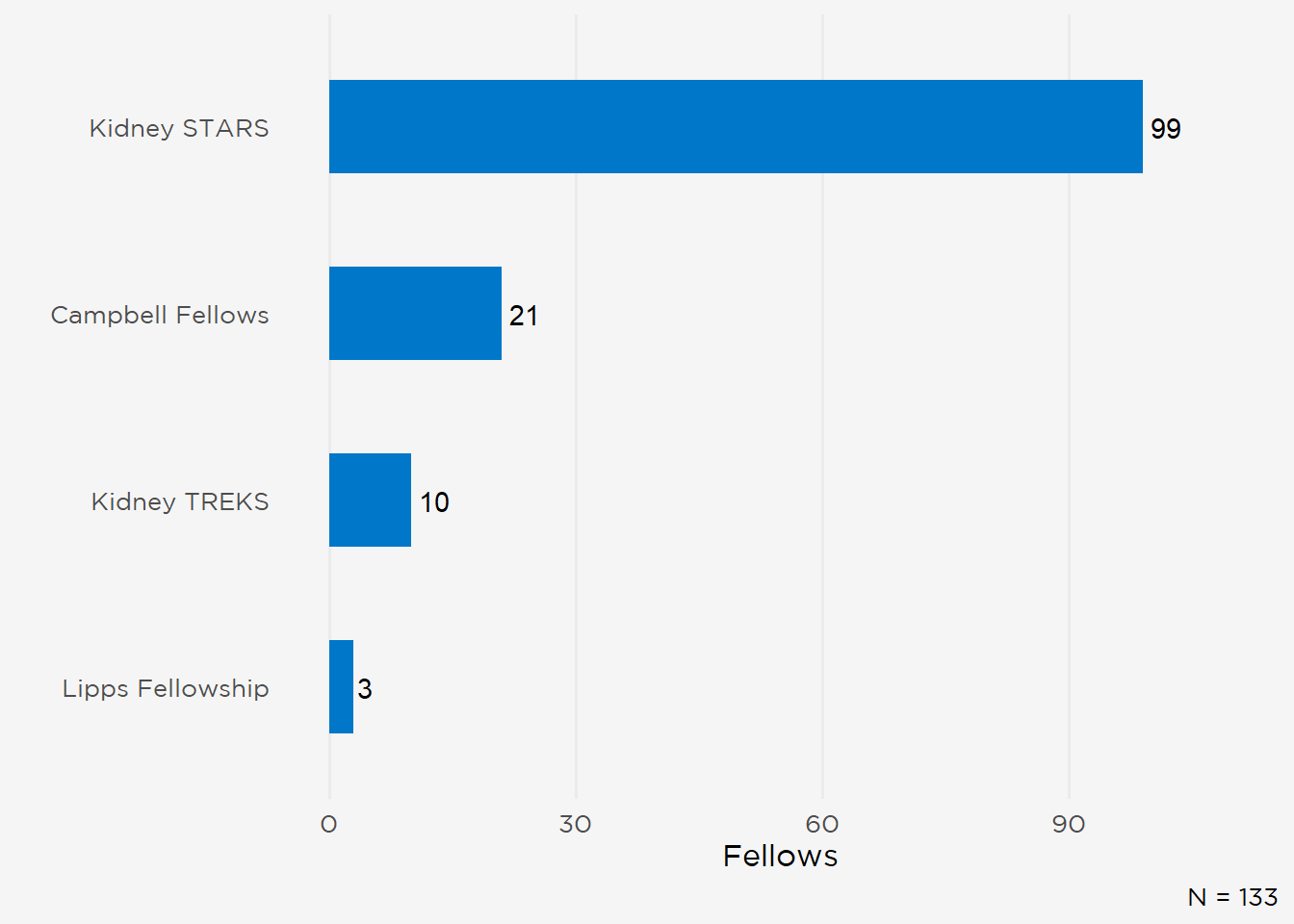
Half of this year’s respondents decided to pursue nephrology during residency, although 23% selected the specialty during medical school. IMGs were more likely to enter nephrology training after practicing in another area of medicine (17% of IMGs vs 8% of USMGs) (Figure 13). Although a substantive portion of fellows became interested in nephrology during medical school and internship, 50% of USMGs and 42% of IMGs considered another subspecialty before selecting nephrology (fellows who had practiced in another area of medicine were censored). Fewer respondents had considered primary care, although more USMGs (48 vs. 24 IMGs) had weighed a internist career (Figure 14). Of the current ASN initiatives to increase interest in nephrology, approximately 20% of all respondents (100 fellows) had participated in ASN Kidney STARS (Figure 15).
Figure 13: When Fellows Chose to Pursue Nephrology.
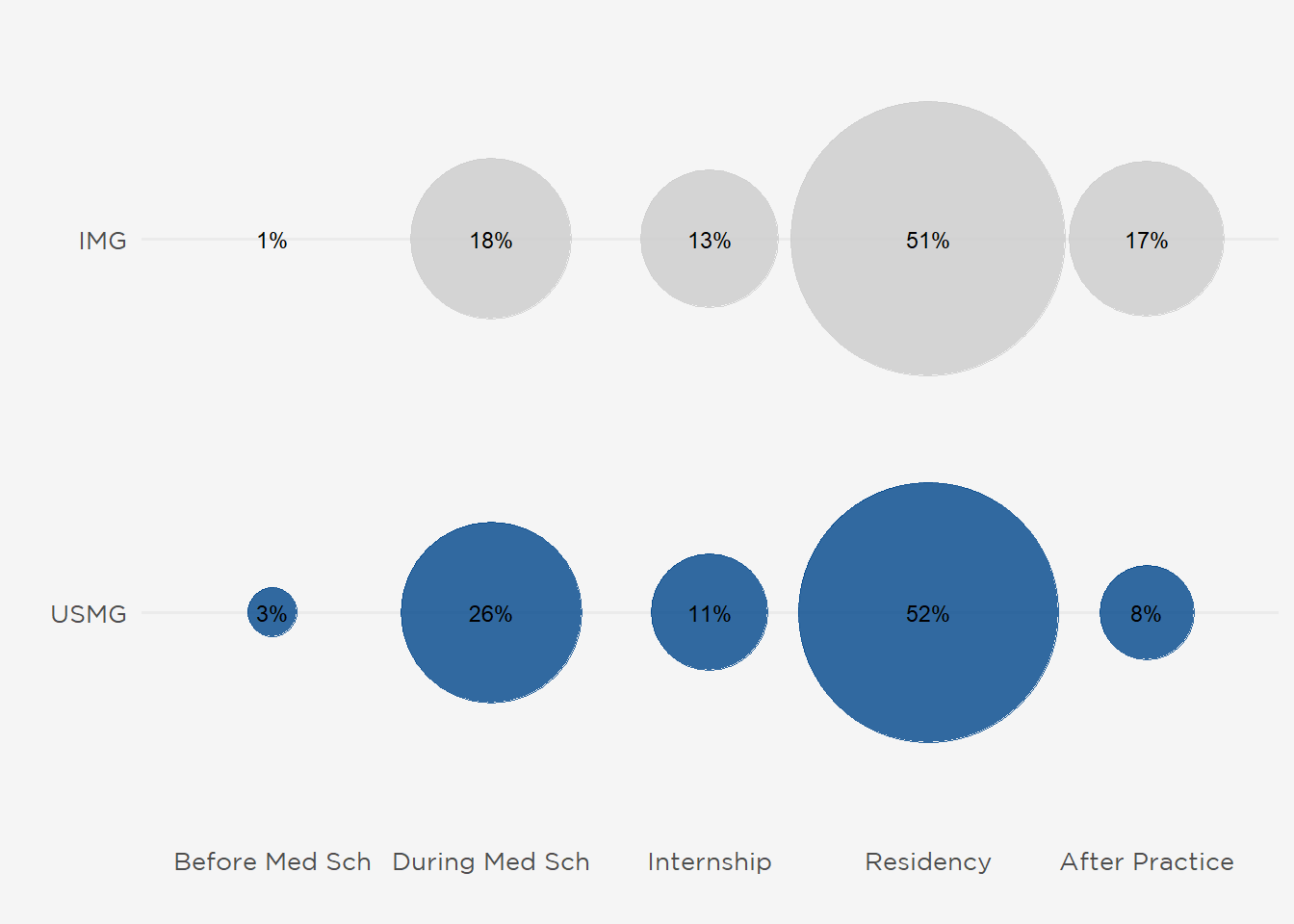
Figure 14: Did Fellows Consider Another Career Before Choosing Nephrology.
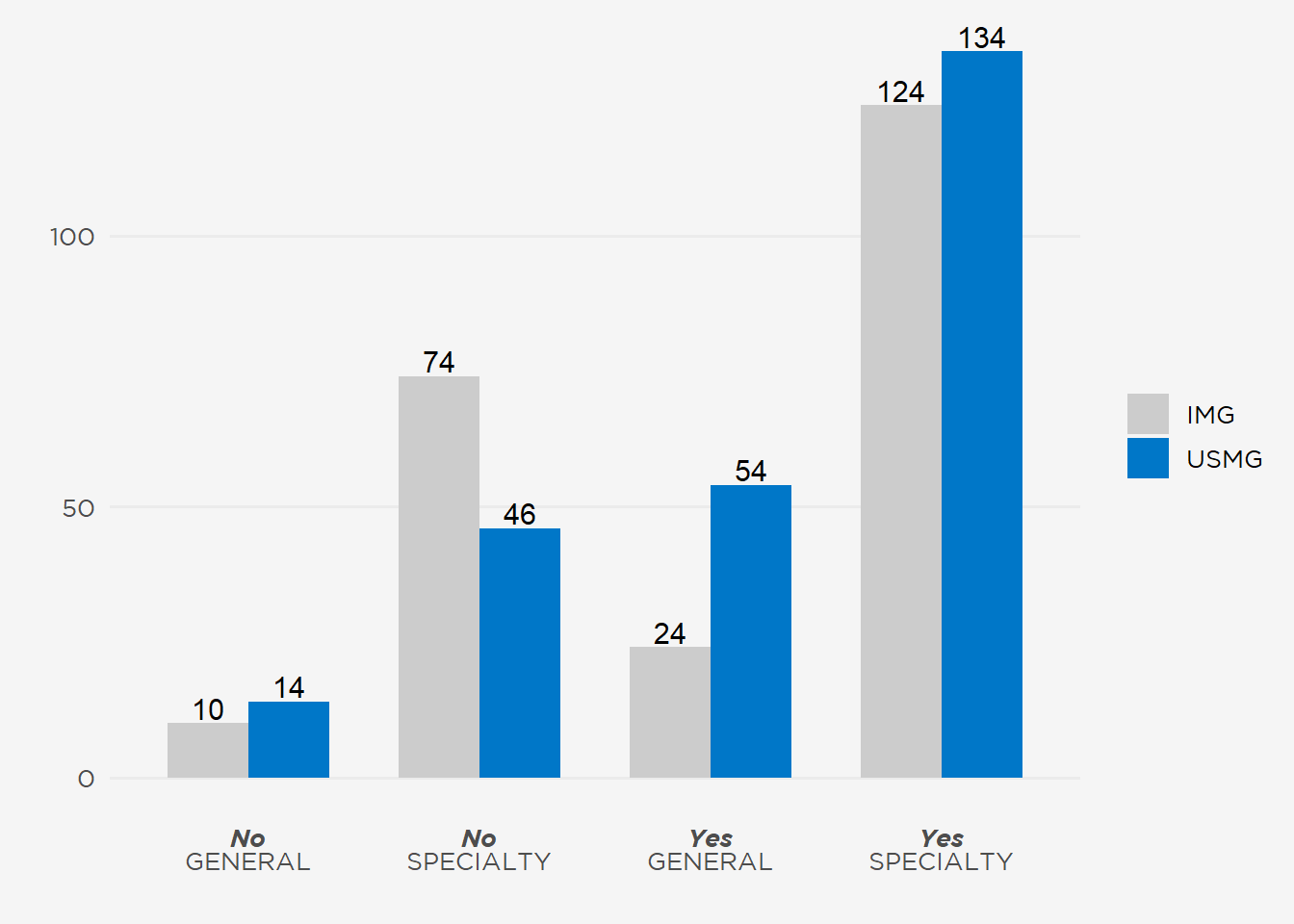
Figure 15: ASN Program Participation.
V. The Incoming Workforce
Capturing the training paths and demographics of the incoming workforce—especially race and ethnicity—are important functions of the annual fellow survey. This year’s survey found:
Fellows Are Focused on Clinical Nephrology: Only 29 of respondents (6%) were pursuing a research fellowship.
Graduates Were Entering Private Practice Over Academic Practice by 2 to 1: Although nearly half of participants were continuing their current fellowship, private practice was the most common destination for graduating fellows. Note that 10 IMG fellows were planning to complete their internal medicine residency required for nephrology board eligibility (Table 4).
Transplant and Critical Care Topped Subspecializations: Of the 79 fellows pursuing additional training, 43% were entering transplant fellowships with 27% pursuing a dual certification in nephrology and critical care (Table 5).
Current Fellows Are Neither Racially nor Ethnically Representative: Only 5% of respondents (26 fellows) are Black and 8% (41 fellows) are of Hispanic/LatinX ethnicity (Table 6).
Fellows Are Carrying a Median $210,000 in Medical Debt: USMGs (median $250,000 vs $46,000 for IMGs) were carrying substantially more debt, although levels did not differ by fellowship type (adult fellows median $210,000 vs $208,000 for pediatric fellows) or gender (median $211,000 for men vs $210,000 for women).
71 Respondents Were Ineligible for the Nephrology Boards: Fourteen percent of respondents (63 adult, 7 pediatric, and 1 adult/pediatric fellow) had not completed a U.S.–based residency and thus would not be eligible to sit for the nephrology board certification exams until they did so.
Table 4: Fellows Plans After Academic Year.
| Plans After 2020‒2021 Academic Year | Number* | Percent |
|---|---|---|
| Continue Current Fellowship | 220 | 47% |
| Private Practice | 107 | 23% |
| Additional Subspecialty Training or Fellowship | 77 | 16% |
| Academic Practice | 47 | 10% |
| Internal Medicine Residency | 10 | 2% |
| Undecided | 8 | 2% |
| *N = 469 Fellow Respondents | ||
Table 5: Additional Training Pursued by Fellow Respondents.
| Additional Training | Number* | Percent |
|---|---|---|
| Transplant Nephrology | 36 | 45% |
| Nephrology–Critical Care Medicine | 22 | 28% |
| Research | 7 | 9% |
| Other | 7 | 9% |
| Interventional Nephrology | 5 | 6% |
| Home Dialysis | 1 | 1% |
| Neurocritical Care | 1 | 1% |
| POCUS | 1 | 1% |
| *N = 79 Fellow Respondents | ||
Table 6: 2021 Nephrology Fellow Survey Respondent Demographics.*
| Variable | Adult Nephrology | Pediatric Nephrology | Meds/Peds Nephrology |
|---|---|---|---|
| Educational Status | |||
| USMG | 214 (46%) | 14 (45%) | 3 (60%) |
| IMG | 251 (54%) | 17 (55%) | 2 (40%) |
| Years of Training Completed | |||
| 1 | 206 (44%) | 5 (16%) | 1 (20%) |
| 2 | 238 (51%) | 15 (48%) | 2 (40%) |
| 3 | 11 (2%) | 11 (35%) | NA |
| 4 or more | 10 (2%) | NA | 2 (40%) |
| Gender Identity | |||
| Man | 270 (58%) | 8 (26%) | 1 (20%) |
| Woman | 189 (41%) | 23 (74%) | 4 (80%) |
| Prefer not to answer | 4 (1%) | NA | NA |
| Citizenship Status | |||
| U.S. citizen | 257 (56%) | 16 (52%) | 5 (100%) |
| Permanent resident | 45 (10%) | 3 (10%) | NA |
| H-1, H-2, or H-3 visa (temporary worker) | 41 (9%) | 2 (6%) | NA |
| J-1 or J-2 visa (exchange visitor) | 103 (22%) | 9 (29%) | NA |
| Other visa (Please specify your "other" visa type) | 2 (0%) | 1 (3%) | NA |
| Prefer not to answer | 13 (3%) | NA | NA |
| Ethnicity | |||
| Hispanic/Latinx | 37 (8%) | 3 (10%) | 1 (20%) |
| Prefer not to answer | 11 (2%) | NA | NA |
| Race | |||
| American Indian or Alaska Native | 3 (0.6%) | 0 (0.0%) | 0 (0.0%) |
| Black or African American | 24 (5.1%) | 2 (6.5%) | 0 (0.0%) |
| East Asian (e.g., China, Japan, South Korea, Taiwan) | 38 (8.1%) | 3 (9.7%) | 0 (0.0%) |
| Pacific Islander | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| South Asian (e.g., India, Pakistan, Sri Lanka) | 151 (32.2%) | 7 (22.6%) | 0 (0.0%) |
| Southeast Asian (e.g., Philippines, Vietnam, Singapore) | 28 (6.0%) | 1 (3.2%) | 1 (20.0%) |
| White | 162 (34.5%) | 15 (48.4%) | 3 (60.0%) |
| Other (Please specify) | 36 (7.7%) | 2 (6.5%) | 0 (0.0%) |
| Prefer not to answer | 27 (5.8%) | 1 (3.2%) | 1 (20.0%) |
| Census Division | |||
| East North Central | 58 (13%) | 4 (14%) | 1 (20%) |
| East South Central | 21 (5%) | 3 (10%) | NA |
| Middle Atlantic | 96 (22%) | 6 (21%) | 1 (20%) |
| Mountain | 18 (4%) | NA | NA |
| New England | 39 (9%) | NA | NA |
| Pacific | 58 (13%) | 4 (14%) | NA |
| South Atlantic | 76 (18%) | 7 (24%) | 2 (40%) |
| West North Central | 29 (7%) | 1 (3%) | NA |
| West South Central | 36 (8%) | 4 (14%) | 1 (20%) |
| *NA = not available. | |||
Concise Methods
Who were surveyed?
The 2021 Nephrology Fellow Survey was distributed to a survey frame of 920 adult, pediatric, and adult/pediatric nephrology fellows drawn from the ASN and American Society for Pediatric Nephrology member databases. The survey garnered a record-high response rate—54% of recipients—including 465 adult, 31 pediatric, and 5 adult/pediatric fellows in training.
How was the survey constructed?
The survey instrument comprised:
- Longitudinal questions drawn from the original 2014 survey focusing on job search experiences, perceptions of the specialty, practice patterns, and demographics
- The Resident Well-Being Index, a proprietary instrument licensed for use in the 2020 and 2021 surveys
- Questions developed by the ASN Data Subcommittee to measure the effects of the COVID-19 pandemic on nephrology fellows’ education and and personal health
The final instrument was piloted by ASN Data Subcommittee members and distributed via Qualtrics.
When was the survey conducted?
Invitation emails were sent on May 4 and the survey closed 28 days later on June 1, 2021.
How were responses analyzed?
The ASN Nephrology Fellow Survey was reviewed and approved by the Johns Hopkins University School of Medicine Institutional Research Board (Study # 00205206). Data obtained from 2021 responses were analyzed using R (R Core Team [2021]. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria.).
Why does ASN survey nephrology fellows in training?
Since 2014, ASN has conducted an annual fellow survey to understand:
- The composition of the incoming workforce, including race, ethnicity, and gender
- Motivating factors for choosing the specialty to tailor approaches to sustain interest in nephrology
- Potential gaps in nephrology education
- Demand for nephrologists in the U.S.
Citation
@online{a._pivert2022,
author = {A. Pivert, Kurtis and M. Boyle, Suzanne and M. Burgner, Anna
and Chan, Lili and Halbach, Susan and Jain, Koyal and Ko, Benjamin
and H. Shah, Hitesh and Waitzman, Joshua and M. Sozio, Stephen},
title = {Nephrology {Training} in the {Time} of {COVID-19}},
date = {2022-01-19},
url = {https://data.asn-online.org/posts/2021_fellow_survey/},
doi = {10.70093/s80639034},
langid = {en}
}