2025 ASN Nephrology Fellow Survey: First Look
Insights from the 12th Annual ASN Nephrology Fellow Survey
2025 ASN Nephrology Fellow Survey—At a Glance
Between April 29 and May 22, 2025, 387 adult, pediatric, and adult/pediatric fellows participated in the 12th annual ASN Nephrology Fellow Survey (39% response rate), including 38% of current adult and 45% of current pediatric trainees.
Graduating adult fellows were entering practice across 38 states, reporting a median base starting salary of $249,000 (interquartile range [IQR], $84,500), a 4% increase over the 2024 Fellow Survey.
Median starting salary for adult fellows was $250,000 for men and $240,000 for women. However, when calculated on a per full-time equivalent (FTE) basis, the difference in earnings reversed, with a mean $271,000/FTE for women and $269,000/FTE for men.
Nearly half of current pediatric trainees responded (comprising 46 pediatric and 2 adult/pediatric fellow participants). Nine graduating fellows entering practice (in clinical nephrology, research, or medical education) reported a median base starting salary of $195,500, a 2.8% increase from the 2024 survey.
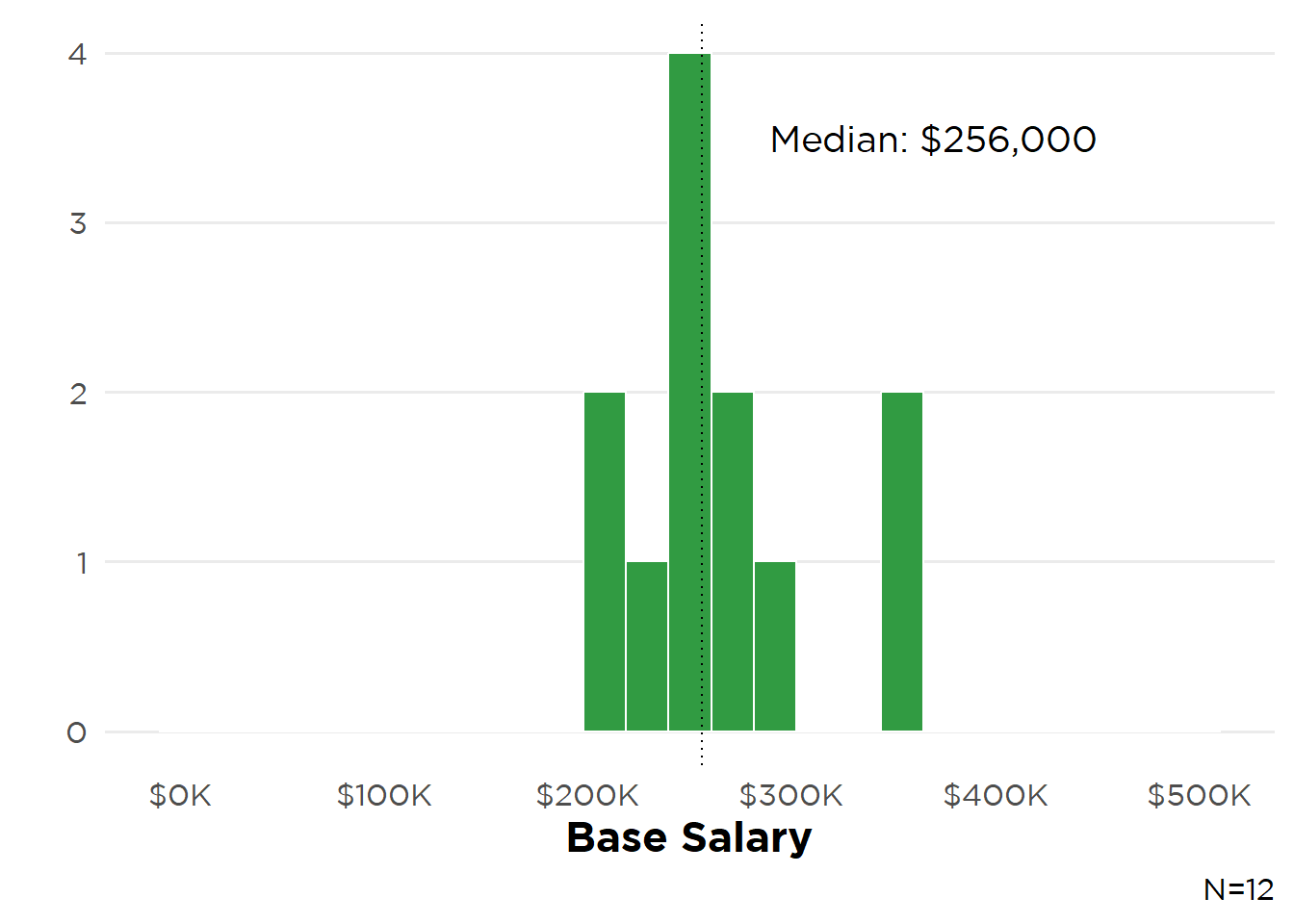
2025 was the second year of the ASN Transplant Nephrology Fellow Survey. Fifteen of the 22 identified transplant nephrology fellows participated (response rate 68%). Nearly two-thirds were motivated to pursue the subspecialty by positive experiences during their transplant rotation (67%) and inspiration from their mentors (60%). The 14 transplant fellows entering practice reported a median base starting salary of $256,000. However, salary varied by practice type, with those in dedicated transplant nephrology positions reporting a median $250,000 versus $230,000 for those in joint transplant/general nephrology jobs.
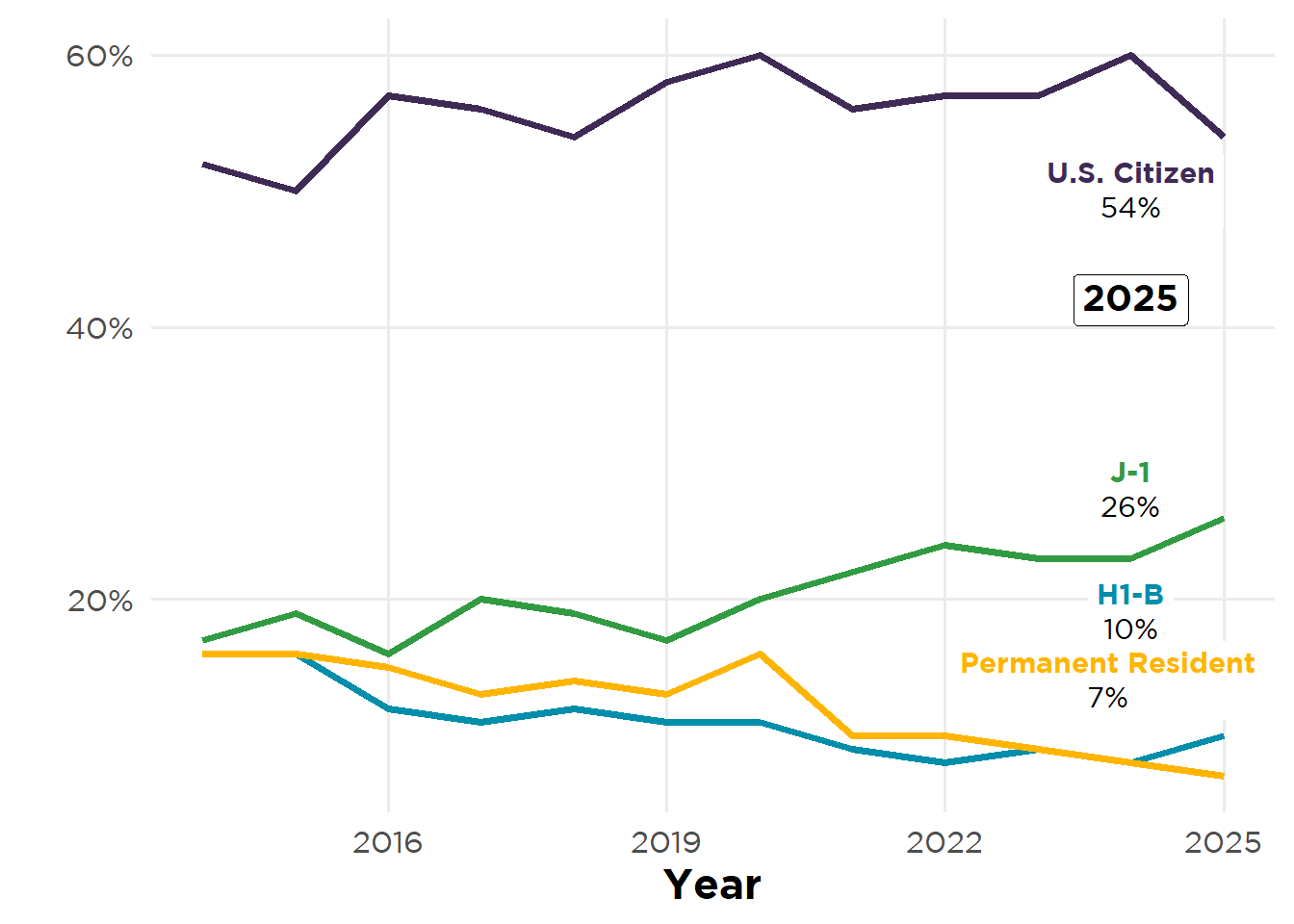
Over the past 12 years survey respondents have been generally representative of the overall fellow population in terms of gender, race, ethnicity, and medical school location. Yet aggregated by citizenship/visa status, the survey has received a greater proportion of responses from U.S. citizens than from trainees on J-1 or H1-B visas (see figure below). (This may be partly due to the increasing number of U.S. citizens who earn their medical degree abroad subsequently entering nephrology.) Because international medical graduates [IMGs] comprise a majority of adult nephrology fellows—and many of these trainees provide much-needed care in underserved areas through J-1 visa waiver programs—future reports will analyze responses by both medical school location and visa status to quantify any potential shifts in this important demographic.
ASN Nephrology Fellow Survey—Respondent Citizenship 2014–2025
I. Incoming Workforce Demographics
In 2025, 39% of current adult, pediatric, and adult/pediatric nephrology fellows (387 of 996) participated in the 12th ASN Nephrology Fellow Survey (Table 1). Respondents comprised 38% of adult fellows and 45% of pediatric fellows. Compared with data from the Accreditation Council for Graduate Medical Education (ACGME) Data Resource Book for 2023–2024, the respondents’ demographics were generally similar to their source population. However, there was overrepresentation of White adult fellows and Asian and Black/African American pediatric fellows, and underrepresentation of Hispanic/Latina/Latino pediatric fellows (Table 2). Among USMG respondents, 22% were osteopathic medical school graduates, less than the 37% of US medical graduates in training reported by ACGME.
Table 1: 2025 Nephrology Fellow Survey Participant Demographics
| Characteristic | Adult (N=339) | Pediatrics (N=46)† | Adult/ Pediatrics (N=2)†‡ |
|---|---|---|---|
| Educational Status | |||
| USMG | 143 (42%) | 33 (72%) | — |
| IMG | 196 (58%) | 13 (28%) | — |
| Years of Training Completed | |||
| 1 | 165 (49%) | 18 (39%) | — |
| 2 | 169 (50%) | 16 (35%) | 2 (100%) |
| 3 | 4 (1%) | 12 (26%) | — |
| 4 or more | 1 (0%) | — | — |
| Gender Identity | — | ||
| Man | 202 (60%) | 12 (26%) | — |
| Woman | 133 (39%) | 32 (70%) | — |
| Prefer not to answer | 3 (1%) | 2 (4%) | — |
| Citizenship Status | |||
| U.S. citizen | 184 (54%) | 40 (87%) | 2 (100%) |
| Permanent resident | 23 (7%) | — | — |
| H-1, H-2, or H-3 visa (temporary worker) | 35 (10%) | 3 (7%) | — |
| J-1 or J-2 visa (exchange visitor) | 89 (26%) | 2 (4%) | — |
| Prefer not to answer | 7 (2%) | — | — |
| Other | — | 1 (2%) | — |
| Ethnicity | — | ||
| Hispanic/Latina/Latino | 37 (11%) | 4 (9%) | — |
| Prefer not to answer | 13 (4%) | 2 (4%) | — |
| Race | — | ||
| American Indian or Alaska Native | 1 (0%) | 0 (0%) | — |
| Asian Total | 166 (49%) | 15 (33%) | — |
| –East Asian | 29 (9%) | 6 (12%) | — |
| –South Asian | 120 (36%) | 7 (14%) | — |
| –Southeast Asian | 17 (5%) | 2 (4%) | — |
| Black or African American | 21 (6%) | 6 (12%) | — |
| Pacific Islander | 0 (0%) | 0 (0%) | — |
| Prefer not to answer | 29 (9%) | 5 (10%) | — |
| White | 120 (36%) | 24 (48%) | — |
| Census Region | |||
| Northeast | 101 (31%) | 11 (24%) | — |
| South | 110 (34%) | 17 (37%) | — |
| North Central | 72 (22%) | 11 (24%) | — |
| West | 42 (13%) | 7 (15%) | — |
| *Percentages may be reported as 0% and/or not total to 100% due to rounding. †— = not recorded or not reported. ‡Multiple values were censored due to small number of respondents. |
|||
Table 2: Respondent Demographics vs. Fellow Population
| Adult Fellows | ||
|---|---|---|
| Variable | ASN Survey | ACGME* |
| Mean PGY-4 Age | 34 | 34 |
| IMGs | 58% | 61% |
| Women | 39% | 39% |
| Asian | 49% | 45% |
| Hispanic/Latina/Latino | 11% | 11% |
| Black or African American | 6% | 6% |
| White | 36% | 25% |
| *Adult nephrology fellows reported in ACGME Data Resource Book Academic Year (AY) 2023-2024. | ||
A majority of respondents were U.S. citizens (59%), with a third training on J-1 (24%) or H1-B (10%) visas (Figure 1). While nearly all adult fellows were in general nephrology training, 9% were enrolled in subspecialty programs—nephrology–critical care medicine (18 fellows), research (12), and interventional nephrology (1 fellow) (Figure 2). USMG participants continued to carry a heavy educational debt load— median $220,000—more than five times that of IMGs (median $40,500) (Figure 3). Nineteen-percent of respondents had participated in Kidney STARS and 12% were Campbell Fellows (Table 3). More USMG fellows chose nephrology earlier in their educational continuum (28% in pre-med/medical school) while 18% of IMGs chose nephrology after practicing medicine independently (Figure 4).
Figure 1: Citizenship Status
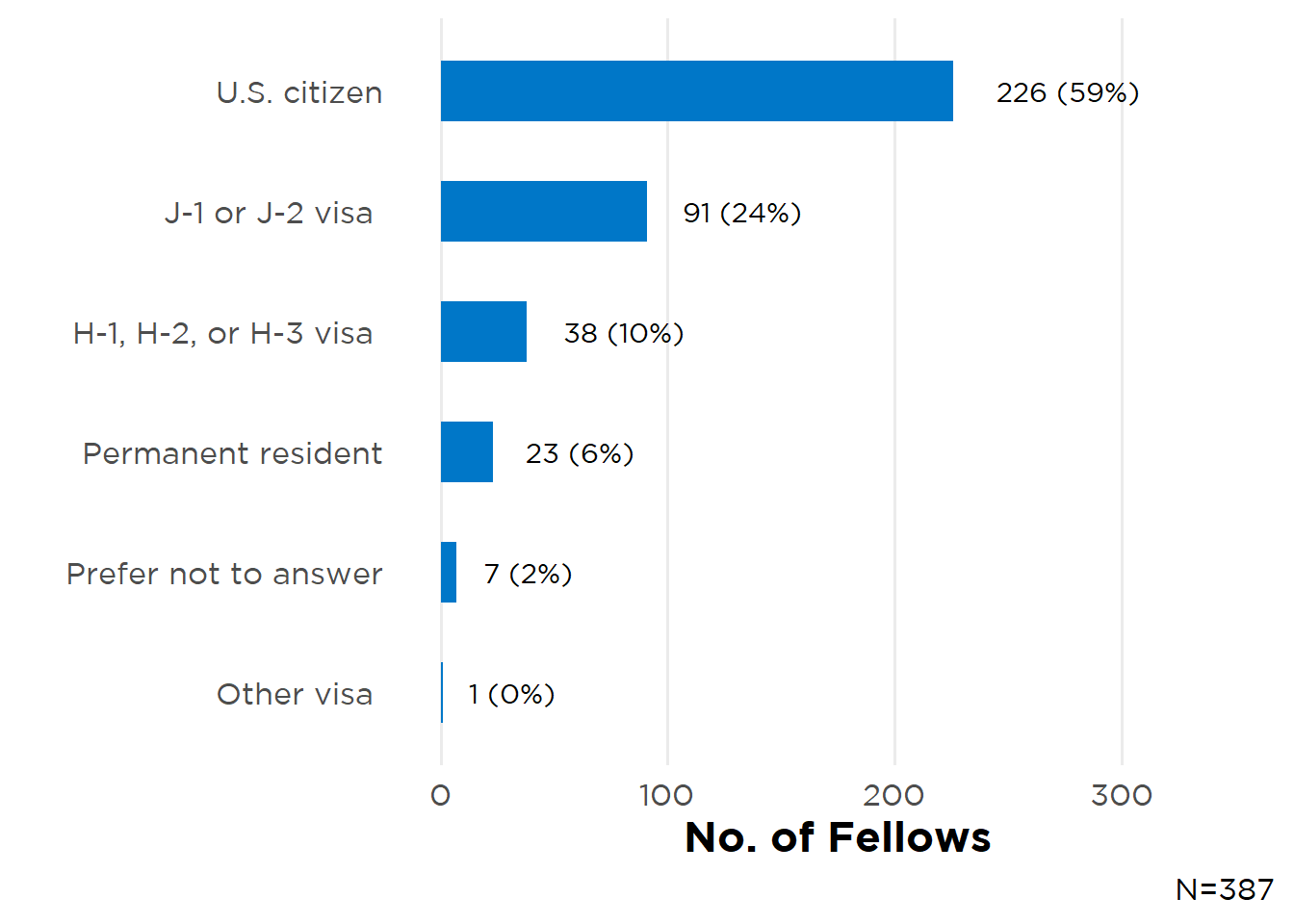
Figure 2: Current Adult Fellowship Type
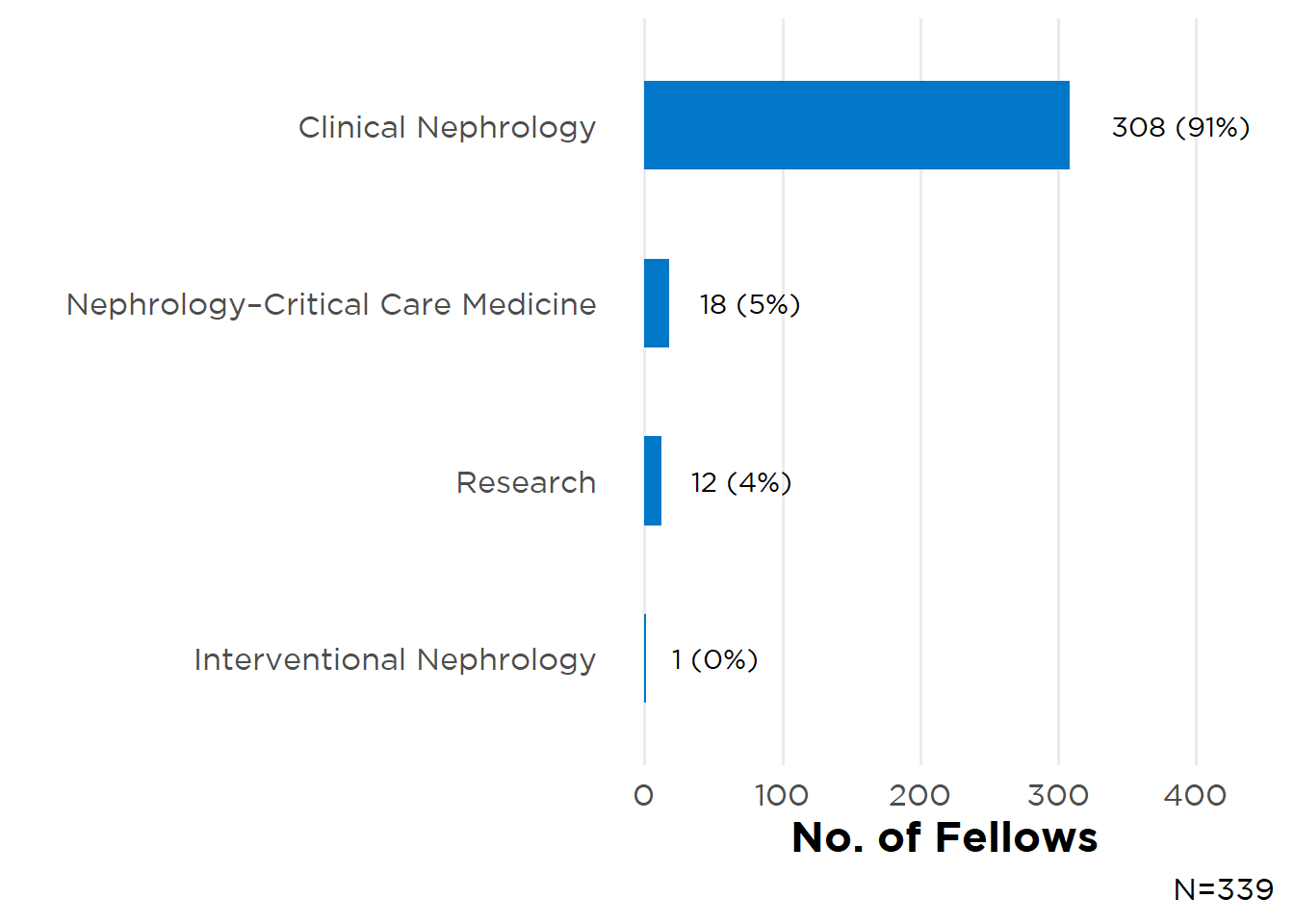
Figure 3: Educational Debt by Medical School Location
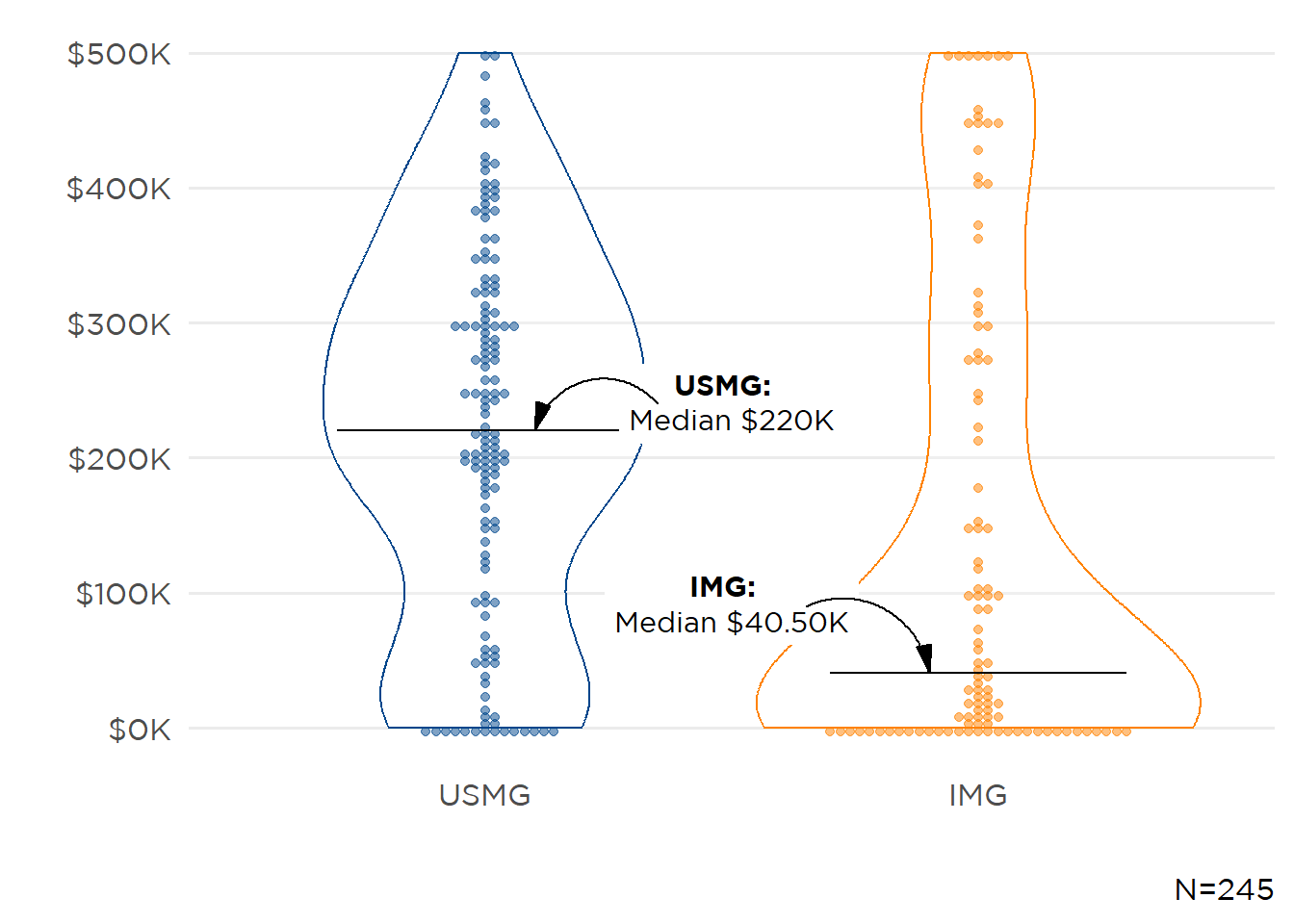
Figure 4: Choosing Nephrology
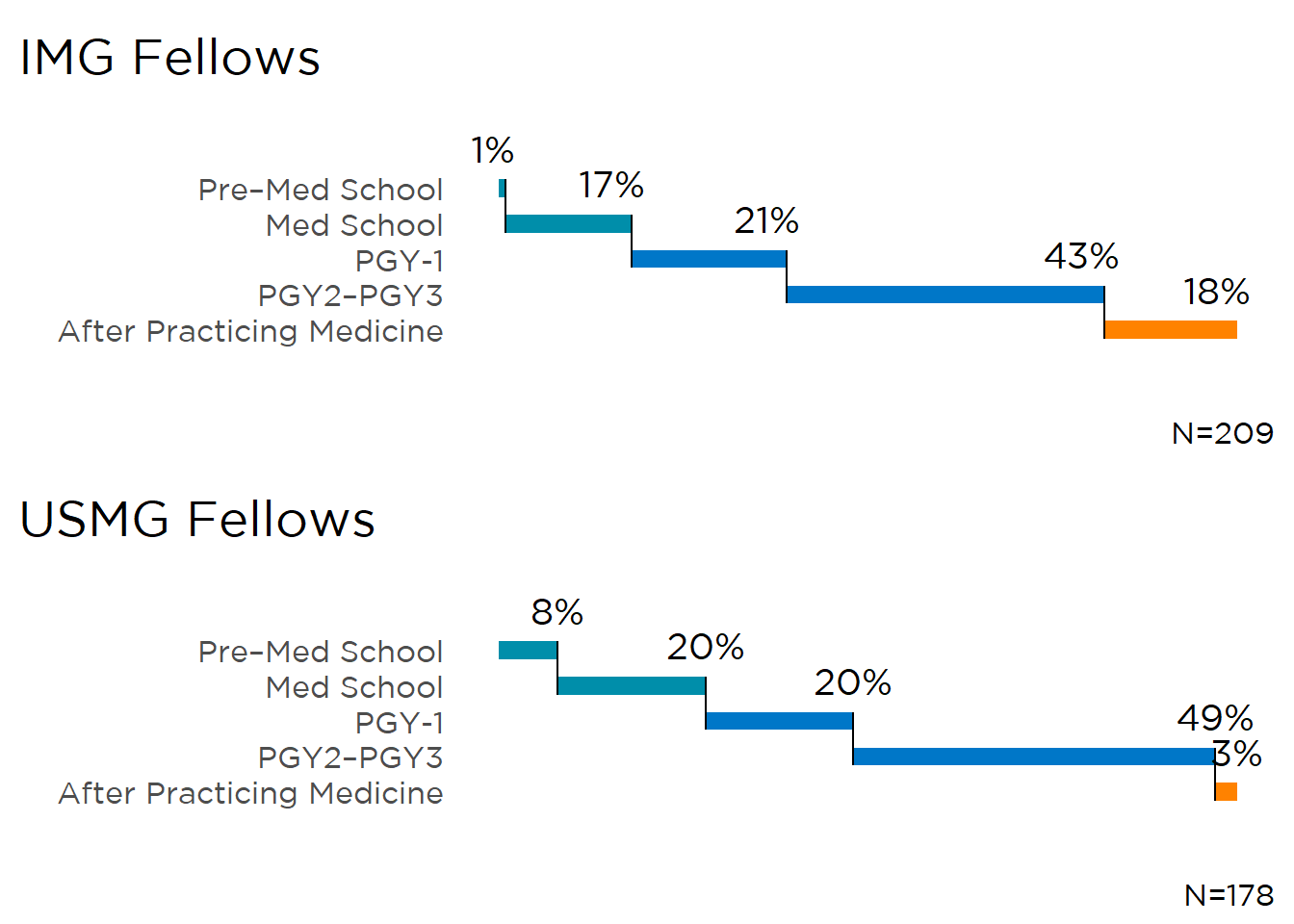
Table 3: ASN Program Participation
| ASN Program | Description | N (%)* |
|---|---|---|
| Kidney STARS | Free Kidney Week Registration & Networking Opportunities | 73 (19%) |
| Campbell Fellows | Travel Support Program for Fellows | 45 (12%) |
| Kidney TREKS | 1-week Research Course Retreat & Long-Term Mentorship Program | 12 (3%) |
| Lipps Research Fellowship | Research Fellowships Funding Fellows Conducting Original, Meritorious Research Projects | 2 (1%) |
| *N=387 | ||
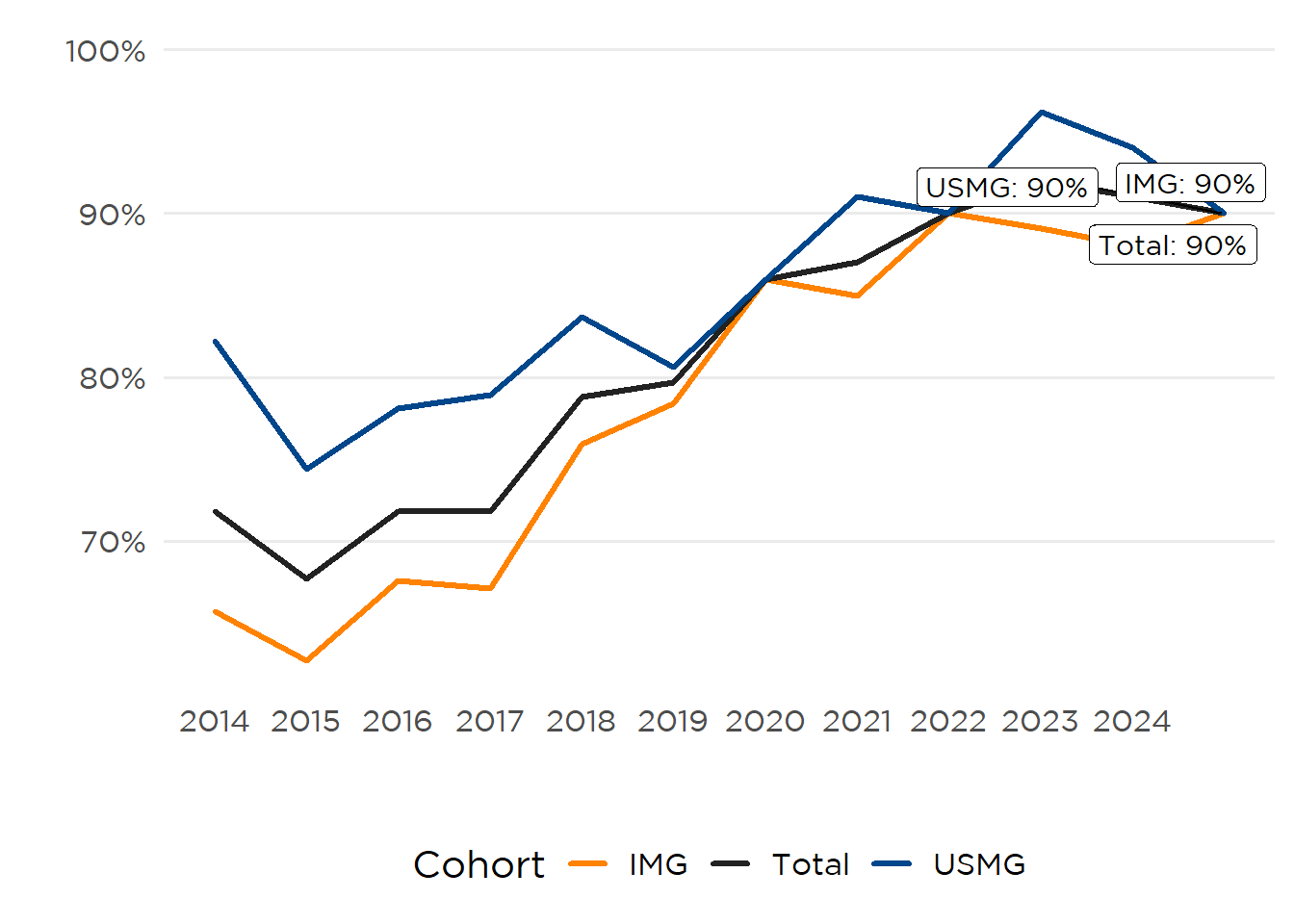
Regardless of fellowship or medical school location 9 of 10 nephrology fellow respondents would recommend the specialty to medical students and residents (Figure 5).
Figure 5: Percent Respondents Recommending Nephrology
This year, nephrology fellow participants recommending the specialty cited the:
Intellectual Challenge Fellows described nephrology as an “intellectually rigorous” and “cerebral” specialty, requiring mastery of complex physiology, pathophysiology, and integration across many domains of medicine.
Diverse Practice Settings and Patient Populations Respondents indicated that the ability to work across multiple practice settings (hospital, clinic, and dialysis center) and the inherent clinical variety (e.g., CKD, hypertension, GN, and transplant) prevents monotony and supports broad professional satisfaction.
Longitudinal Relationships and Patient Impact Many respondents value the opportunity for “continuity with patients” and forming “long-lasting connections.” The specialty enables physicians to make a significant difference in patients’ lives, especially those with chronic conditions.
Advancements and Growing Opportunities Fellows indicated the specialty is growing, with “an abundance of well-compensated job openings,” recent “boom in new therapies,” and plentiful research opportunities. The field is described as both “expanding” and offering a strong job market due to the rising burden of kidney diseases.
See Perspectives—Would Recommend Nephrology.
Fellows who would not recommend nephrology indicated:
Poor Compensation Relative to Workload Respondents not recommending nephrology indicated the specialty offered relatively lower salary and financial incentives compared with other medical subspecialties—especially for high intensity and broad scope of work—despite requiring similarly lengthy and demanding training. This can be a deterrent for students evaluating time invested versus future earnings.
Challenging Work-Life Balance and High Burnout Risk Fellows pointed to demanding schedules, often inflexible call requirements, and stress that comes with balancing multiple care settings (inpatient, outpatient, dialysis).
Lack of Prestige, Respect, and/or Procedural Opportunities Some reported feeling underappreciated by patients and colleagues, and lamented having fewer procedural or interventional options compared with other specialties.
Difficult Training/Job Market and Limited Career Advancement The path to partnership in private practice is perceived as long and arduous, with limited high-paying jobs (especially in desirable locations).
Perspectives—Would Recommend Nephrology
It is a very good [field] to practice if you love medicine, interactive thinking, you love when you master the philology of fluids, electrolytes, body adaptations and then you enjoy each and every case, you feel satisfied when you manage difficult cases and help medicine team, also teach them its a very enjoyable field.
You feel satisfied when you manage difficult cases.
Nephrology is a full-rounded medical field that is complex and intellectually challenging with diverse clinical pathology that allows for integration of many sciences such as physiology, pharmacology and pathology like no other field
Nephrology lets us build long-term relationships with our patients who we take care throughout the different stages of their kidney disease creating a meaningful and long-lasting connection that not many subspecialties have.
There is a lot of exciting research in nephrology, with more and more novel therapies available where there previously were only limited options.
Perspectives—Would Not Recommend Nephrology
One drawback is the extended training period, comparable to other pediatric subspecialties, without the same level of financial compensation.
I would be very honest about the downsides that we’re underpaid and overworked.
The degree of workload… seems incongruent with a good work life balance…logistically speaking I think it might make sense to pursue a career as a hospitalist.
Not a rewarding field, poor compensation, constant stress dealing with labs, prescriptions, outpatient and inpatient mix—you work like 2 or 3 doctors. It’s like a PCP job but worse compensation, more hours in the job.
No respect in nephrology by other colleagues. Low pay for amount of work we do. No procedure. A lot of guessing and speculation … and rarely we do anything apart from ‘supportive care.’
The starting income is low even in private practice and to get to the potential salary goal may take many years. Also academic institutions may play the game of numbers (patients to see) to improve income.
Unfortunately, Nephrology by the masses, is similar to the middle child: in-between other specialties that get the most attention.
II. Future Plans
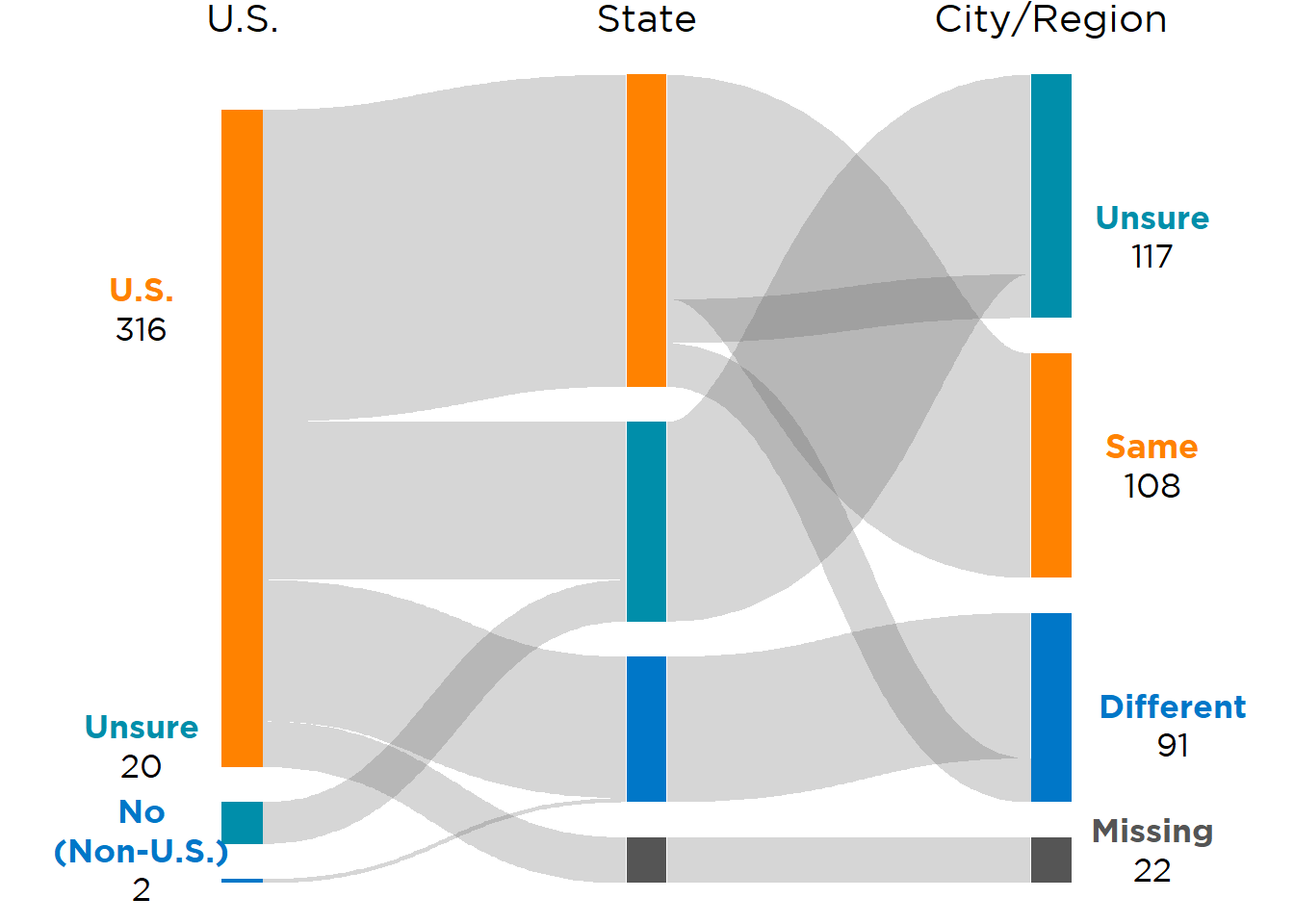
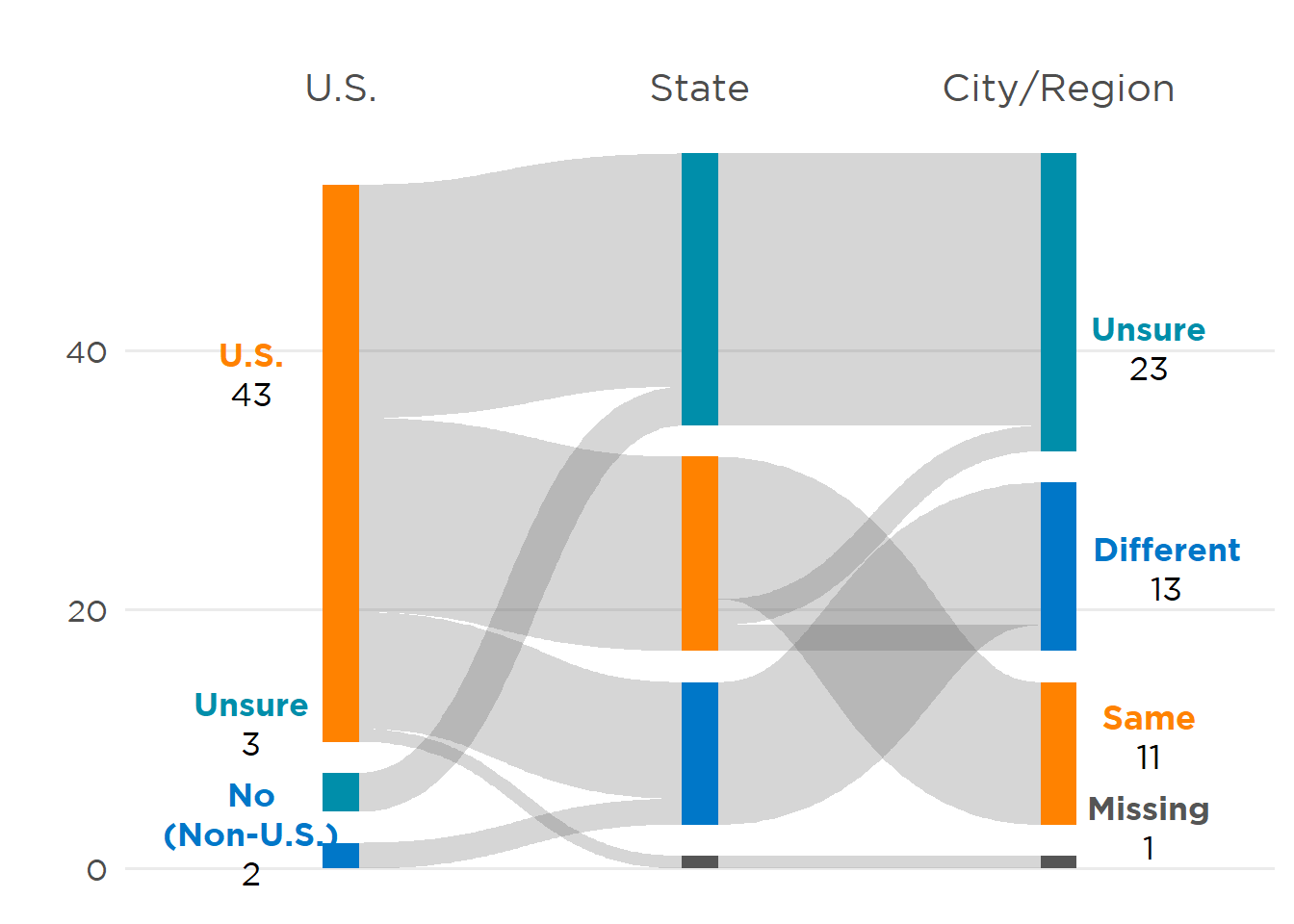
Half of the participating adult nephrology fellows (168) were continuing their current fellowship (Figure 6). Of the 171 graduating fellow respondents, 37% were entering private practice, 25% academic practice, 23% pursuing additional post-fellowship training, and 5% starting an internal medicine (IM) residency. Since the 2019 Fellow Survey, between 4 and 15 fellow respondents have indicated they were entering an IM residency post-fellowship. Of the 40 pursuing further training, 45% were entering a transplant nephrology fellowship, 28% critical care, 13% interventional nephrology, 5% glomerular disease, 5% research, and 3% onconephrology. All but 4 adult respondents planned to enter their first post-fellowship job in the U.S., with 44% planning to remain in the same state, and 32% in the same city/region as their training institution (Figure 7).
Figure 6: Future Plans
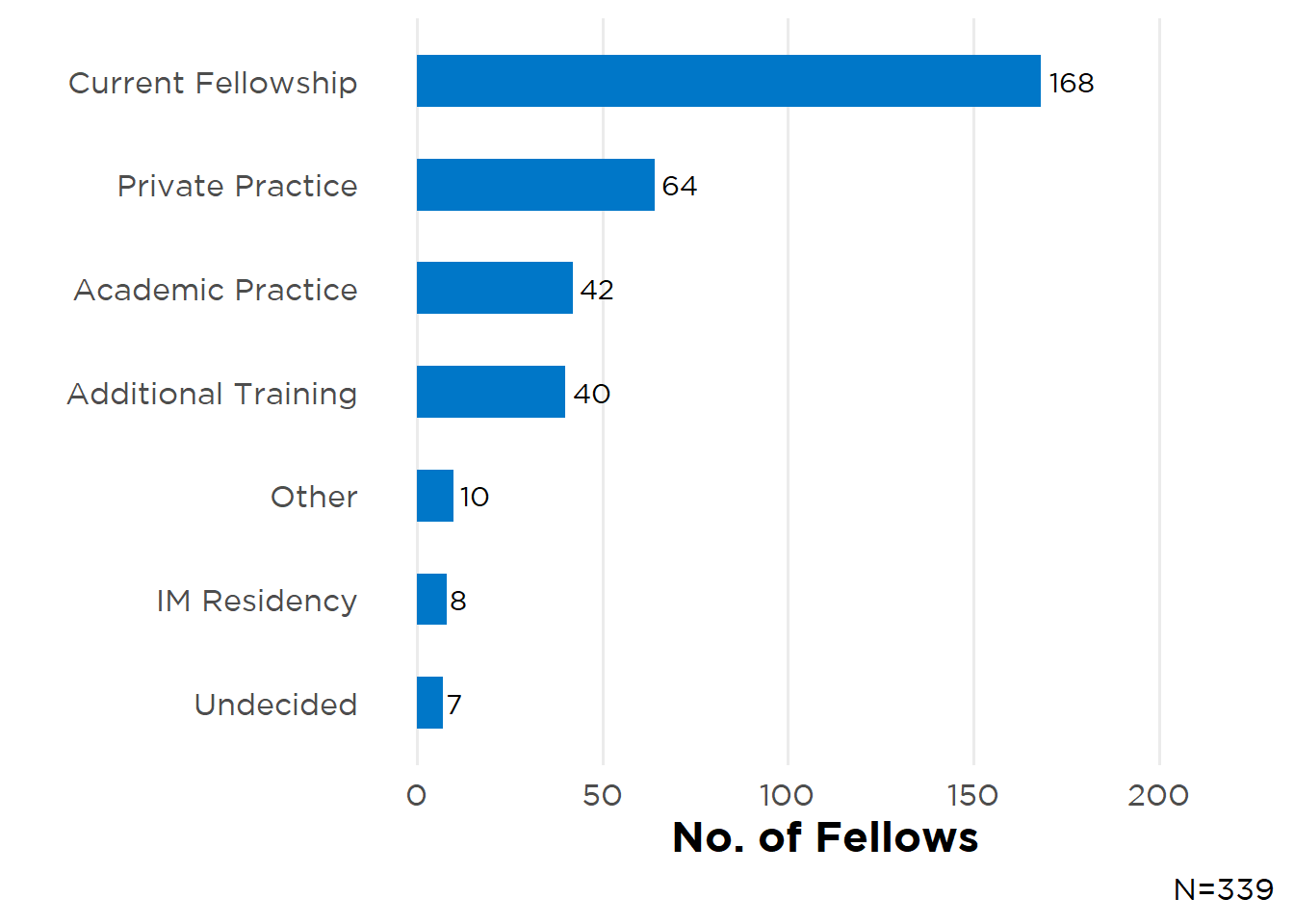
Figure 7: Planned Post-Fellowship Job Location
Job Market Perspectives
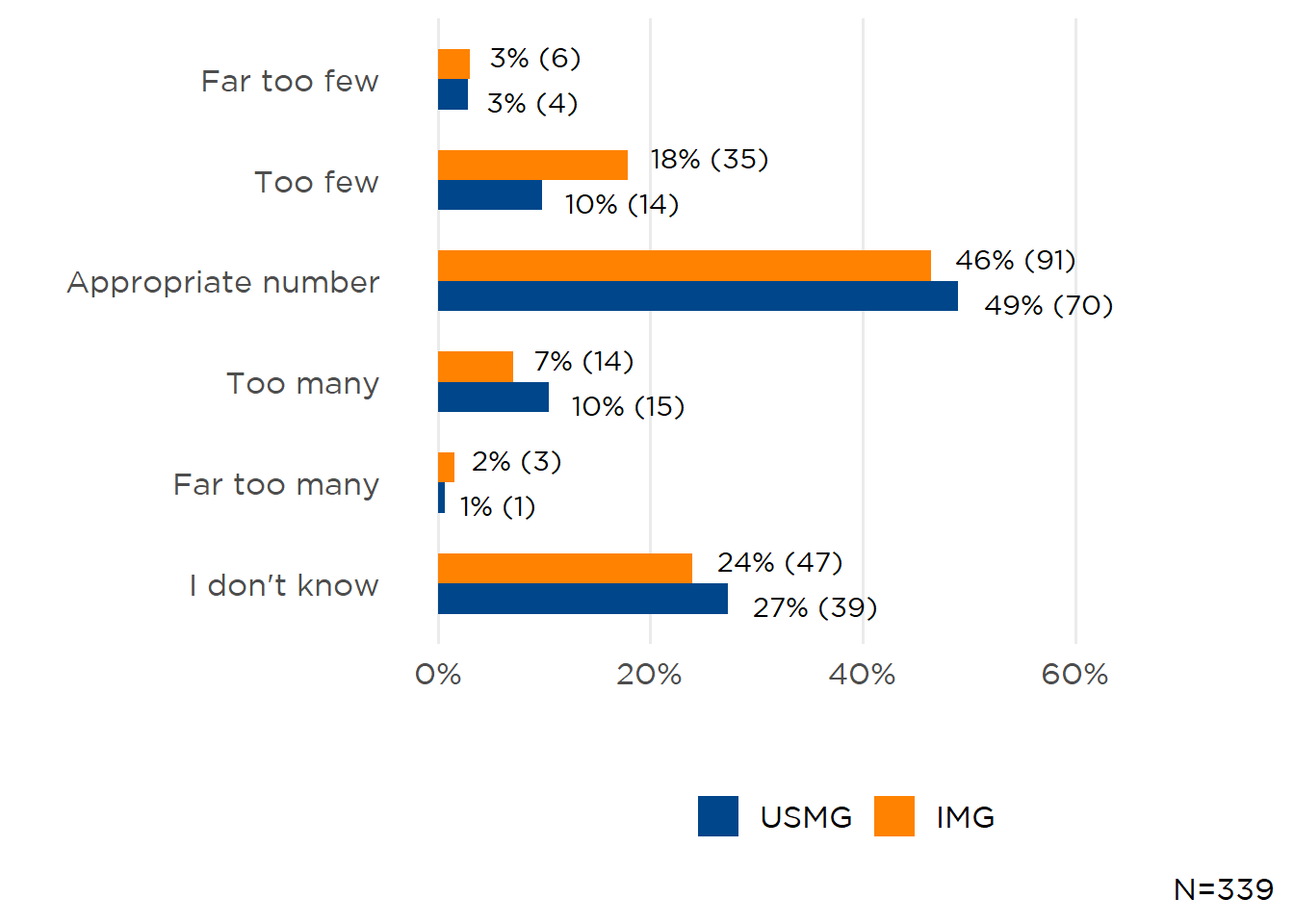
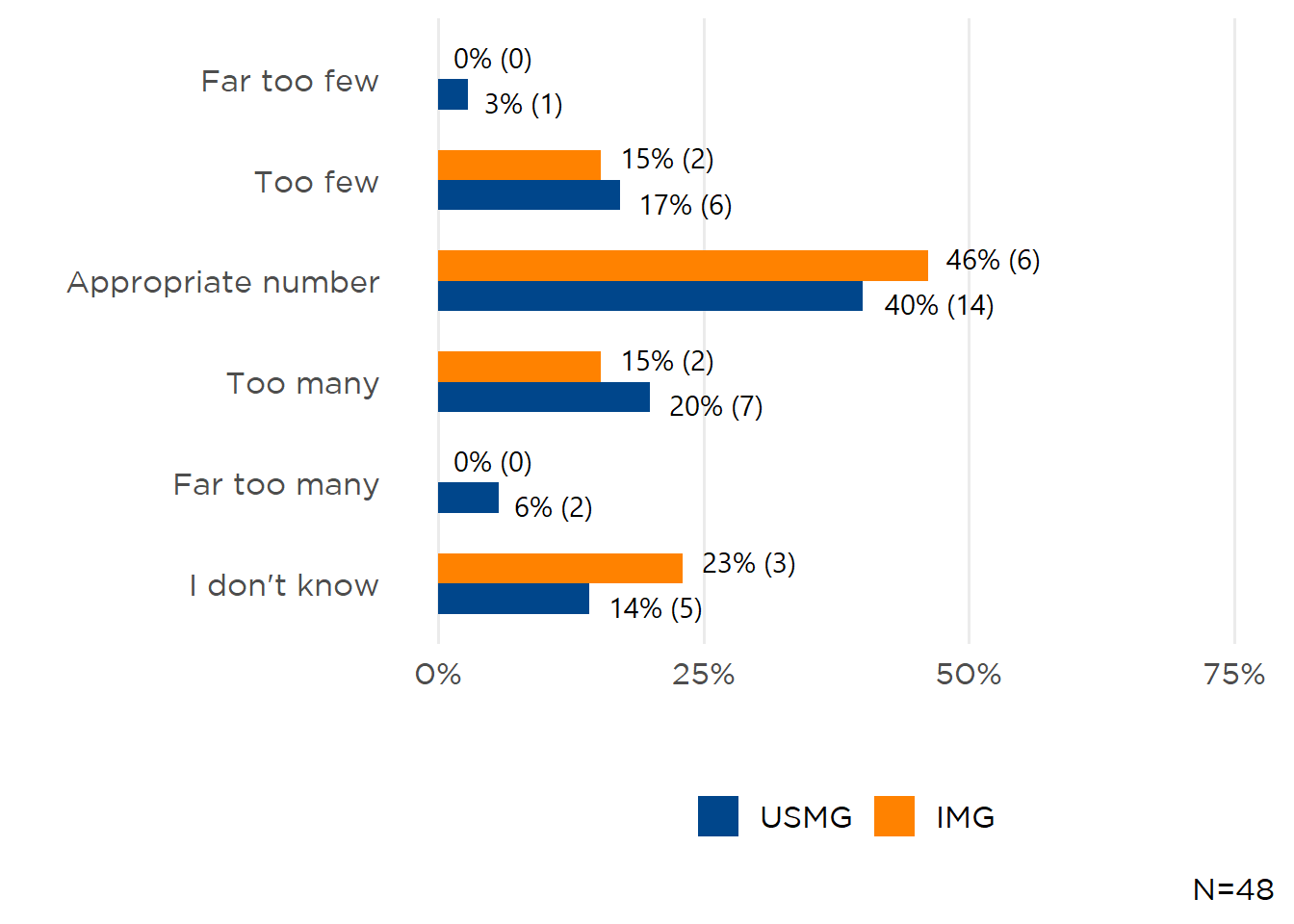
Although subjective, fellows’ perceptions of nephrology employment opportunities are a leading indicator of the strength of the local (within 50 miles of their training program) and national nephrology job market. IMGs continue to be more pessimistic than USMGs about the availability of local opportunities, with 35% assessing an appropriate number of positions and 38% saying there were “Far too few”/“Too few” (Figure 8) compared to 57% of USMGs perceiving that an appropriate number of local opportunities exist, and only 23% saying there were “Far too few”/“Too few.” Nationwide, nearly half of both IMG (46%) and USMG (49%) participants perceived an appropriate number of opportunities even though 21% of IMGs still saw “Far too few”/“Too few” jobs (Figure 9). Of note, nearly a quarter of respondents were unsure of the strength of both the local and national nephrology job market. Of those unsure of the local market, 31% of respondents were PGY-5 or beyond, and those unsure of the national market, 36% at PGY-5 or beyond.
Figure 8: Local Job Market Perspectives
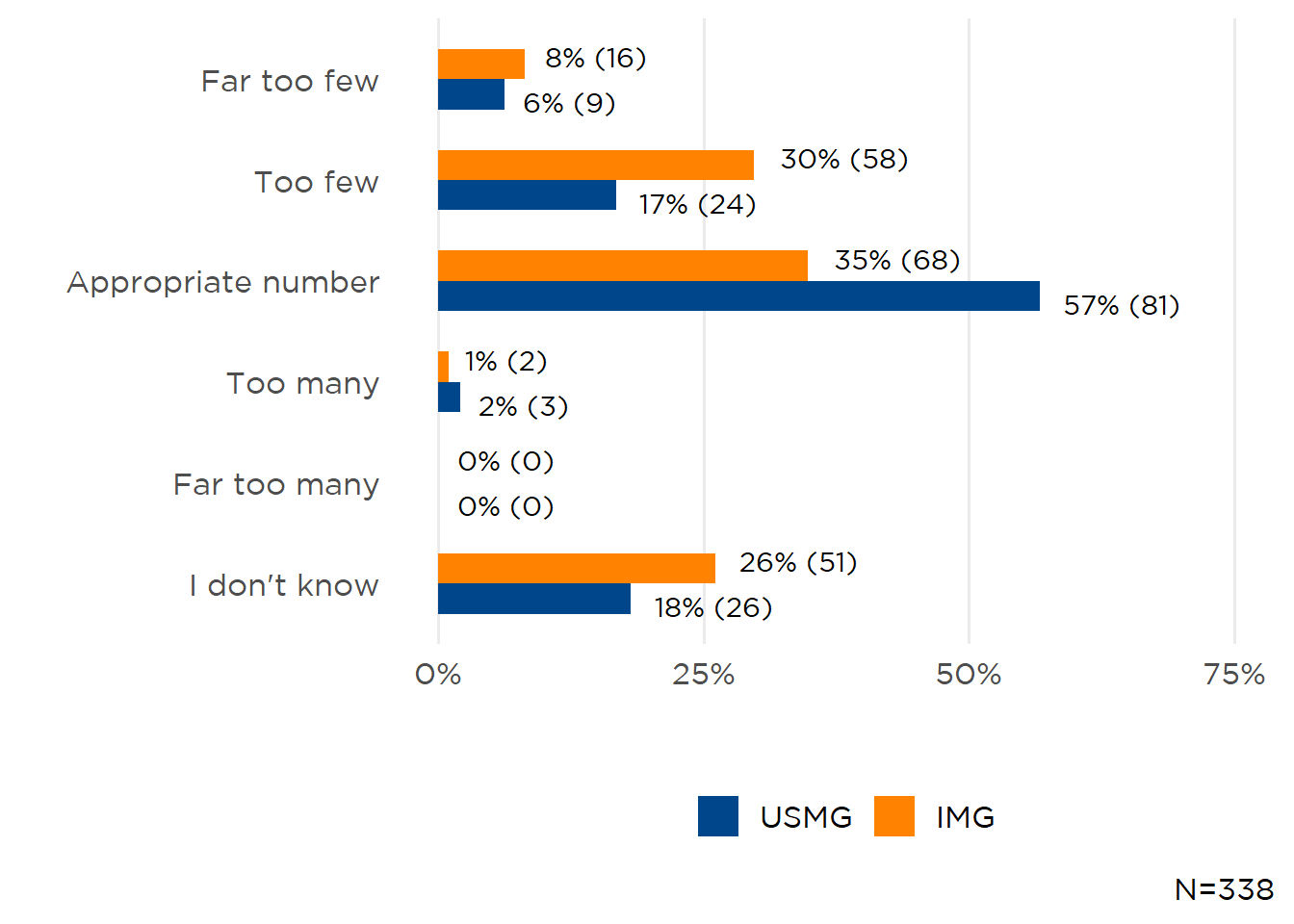
Figure 9: National Job Market Perspectives
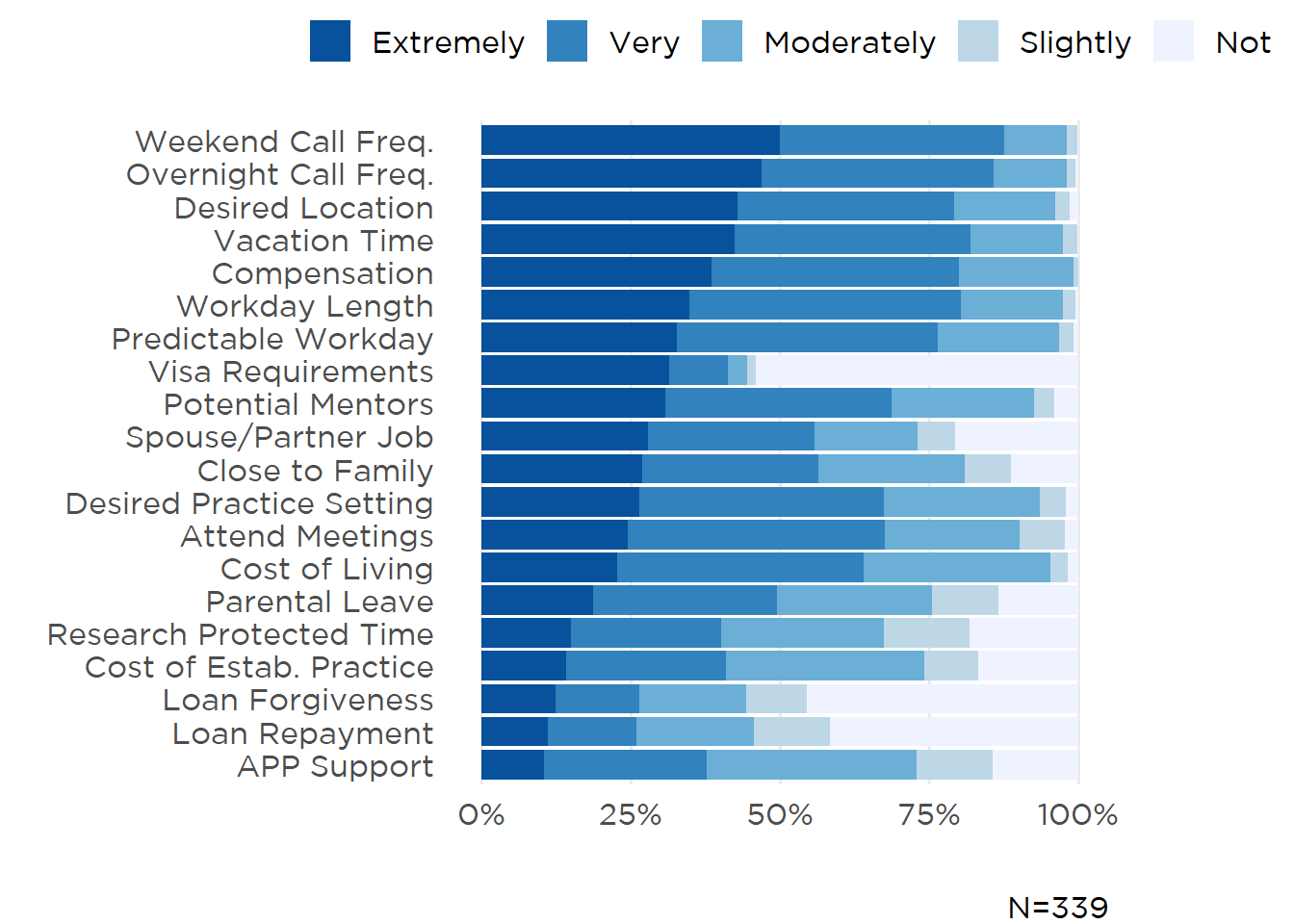
Important Factors When Choosing a Job
Lifestyle aspects of employment—night and weekend call frequency, desired locale, and vacation time—continue to top the list of factors fellow value when evaluating job offers with compensation rounding out the top 5 (Figure 10). While USMGs had the same top factors as the overall cohort, IMGs placed a greater emphasis on visa requirements (ranked third-highest) and workday length (fifth-highest).
Figure 10: Important Factors
III. Fellow Job Search Experiences
At the time of survey completion (see Methods), 123 adult fellows had initiated their job search, mainly focused on clinical nephrology positions (106 fellows, 86%) (Table 4). Eleven were searching for a nephro-hospitalist position and one a general hospital medicine position. Only 4% of fellows sought a research-focused position. One-third (36%) experienced difficulty in finding a position they considered satisfactory, with a lack of jobs offering adequate salary most cited by both IMGs and USMGs (Table 5).
Table 4: Positions Sought
| Positions Sought | |
|---|---|
| Job Type | N |
| Clinical Nephrology | 106 |
| Medical Education | 19 |
| Hospitalist—Nephrology | 11 |
| Dual Nephrology/Other Specialty | 6 |
| Nephrology—Research | 5 |
| Hospitalist | 1 |
| Non-nephrology—Research | 1 |
| *N=111. | |
Table 5: Reasons Cited for Difficulty in Finding a Satisfactory Nephrology Position*
| Unable to Find a Job: | IMG (N=27) | USMG (N=16) |
|---|---|---|
| Offering adequate salary/compensation | 21 (78%) | 11 (69%) |
| In a desired location | 17 (63%) | 13 (81%) |
| In a desired practice setting (e.g., hospital, group practice) | 14 (52%) | 7 (44%) |
| That met visa status requirements | 8 (30%) | 3 (19%) |
| Other | 6 (22%) | 3 (19%) |
| Offering employment opportunities for spouse/partner | 0 (0%) | 1 (6%) |
| *N=43 | ||
IV. Entering Practice
Adult fellow respondents had applied for a median of 4 positions and received a median 3 employment offers. One-hundred-twenty-two adult fellows had been offered a position and had either accepted (n=100) or were continuing their search (n=15). Half were entering private practice (n=55), with 40% starting in academic hospitals, 9% in non-academic hospitals, and 2% in government (Figure 11). Nearly 9 in 10 fellows (89%) were entering clinical nephrology positions (Figure 12) where they would be responsible for CKD, in-center hemodialysis, CKRT, and PD (all ≥75% of respondents) (Table 6). One of the least-represented practice domains was research, with only 18% of fellows participating in clinical research and 3% of fellows with responsibilities in basic or translational research.
Figure 11: First Position Employer
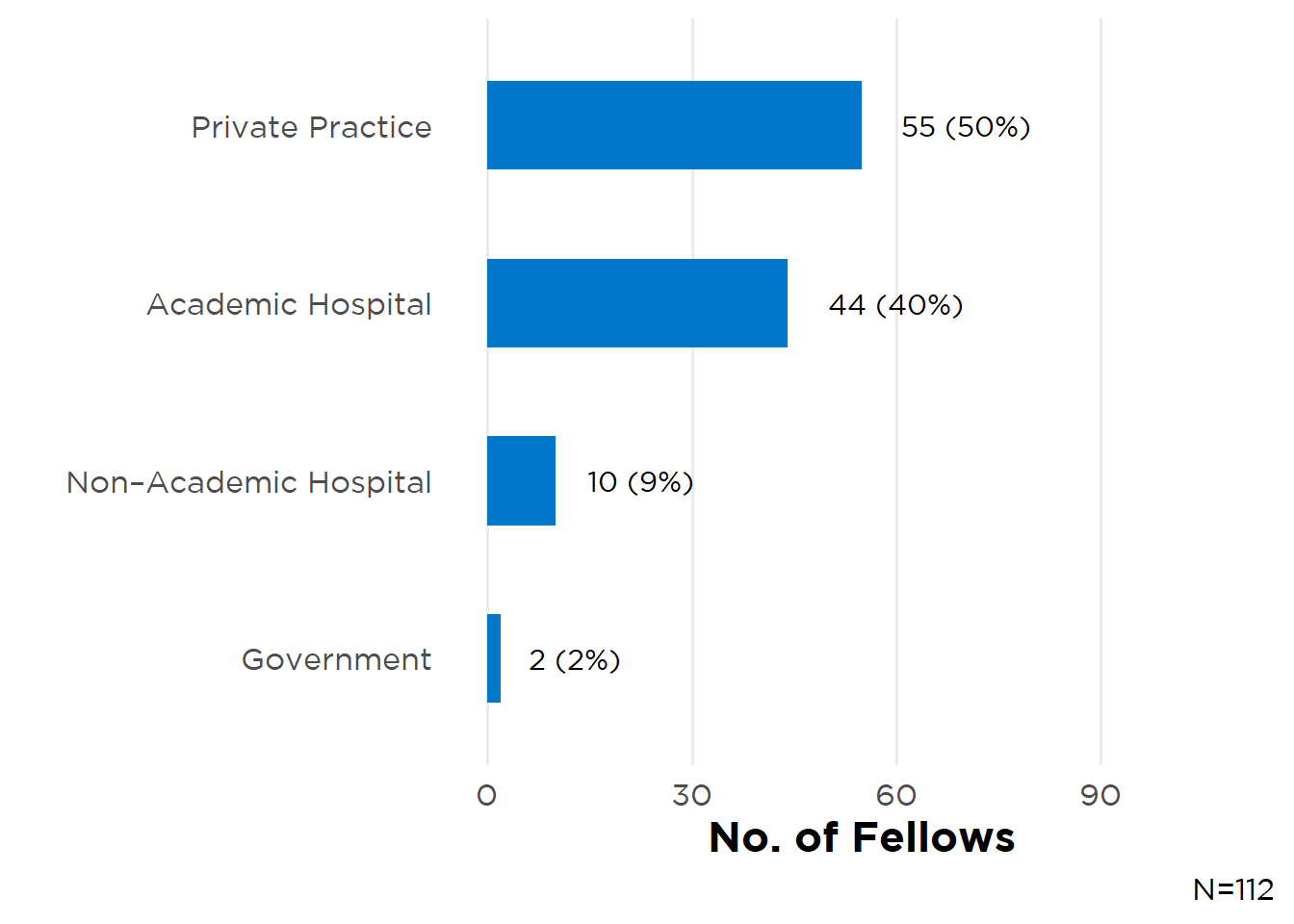
Figure 12: First Position Focus
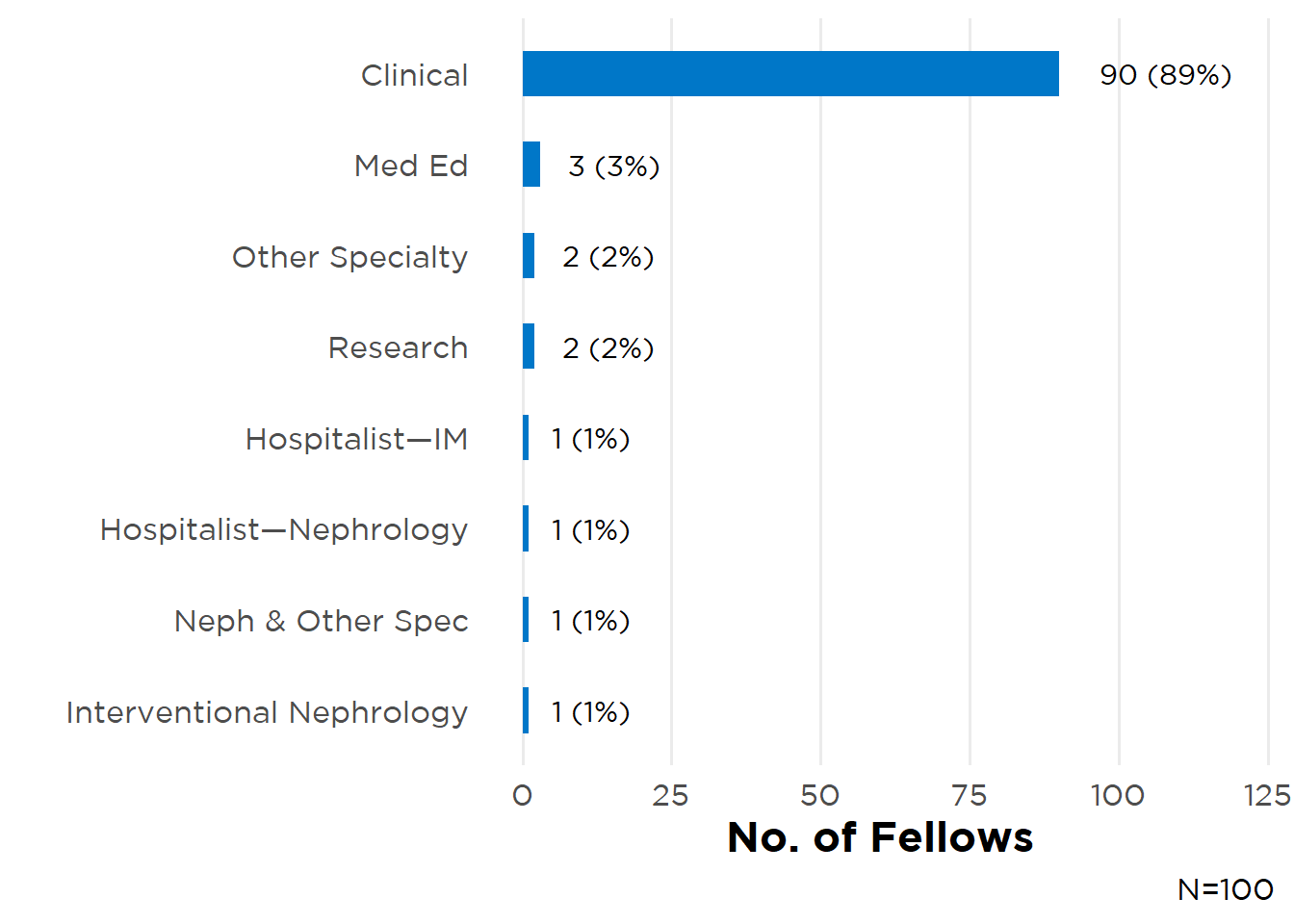
Table 6: Responsibilities in Practice
| Responsibility | N (%)* |
|---|---|
| General Nephrology Outpatient Clinic | 106 (95%) |
| CRRT | 93 (83%) |
| Outpatient—In-center HD | 92 (82%) |
| PD | 87 (78%) |
| Home HD | 68 (61%) |
| Education | 52 (46%) |
| Dialysis Medical Director | 32 (29%) |
| PLEX | 29 (26%) |
| Clinical research | 20 (18%) |
| Hypertension Specialty Clinic | 19 (17%) |
| Joint Venture—Dialysis | 19 (17%) |
| Apheresis | 19 (17%) |
| Kidney biopsy | 17 (15%) |
| POCUS | 16 (14%) |
| Nephrolithiasis Specialty Clinic | 14 (12%) |
| Glomerular Disease Specialty Clinic | 14 (12%) |
| Dialysis catheter placement | 10 (9%) |
| Transplant Outpatient Clinic | 9 (8%) |
| Interventional nephrology | 4 (4%) |
| Other | 3 (3%) |
| Translational research | 2 (2%) |
| Basic science research | 1 (1%) |
| *N=112 | |
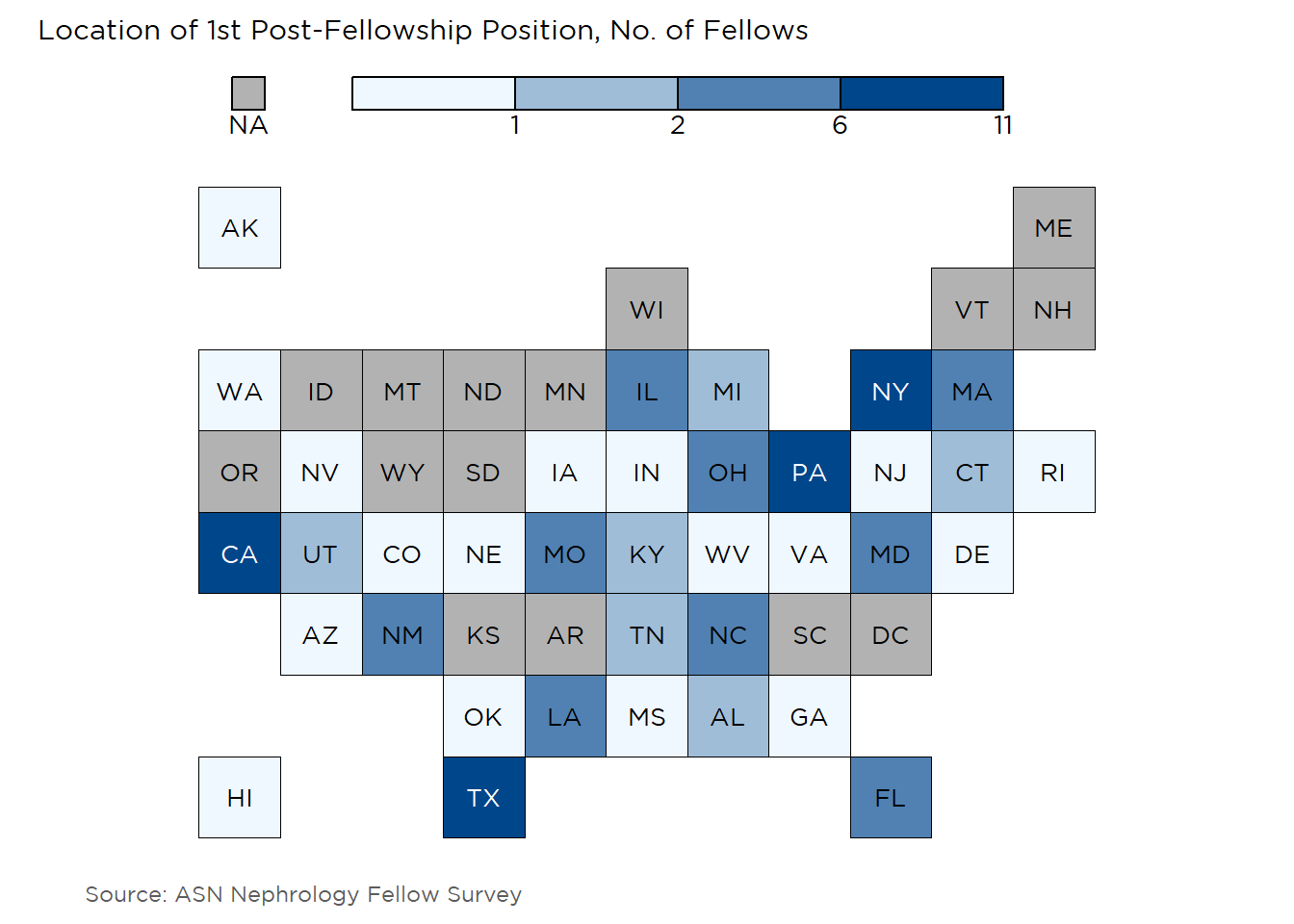
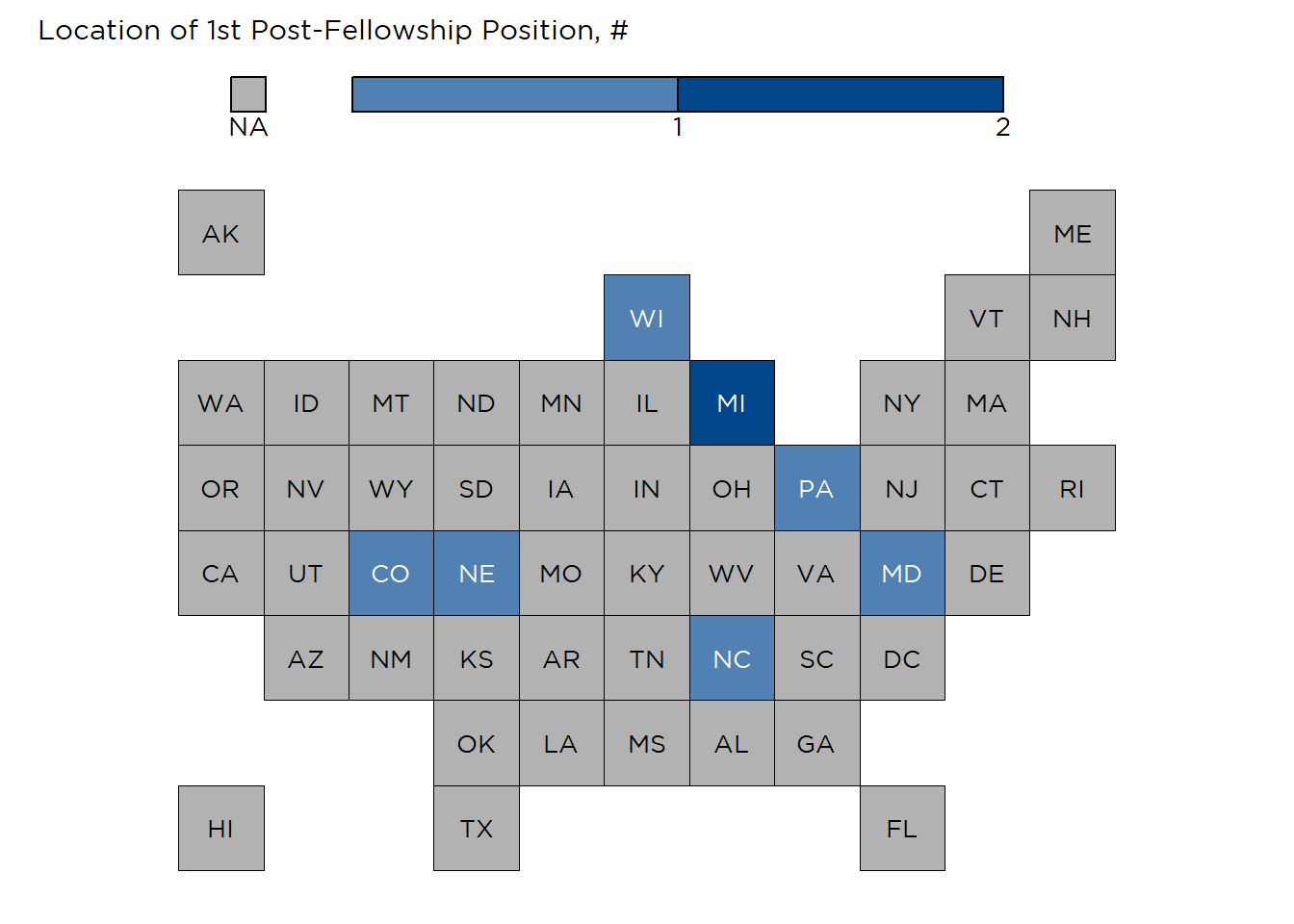
Adult nephrologists were starting practice in 38 different states (Figure 13), with relatively higher density in the Northeast region and fewer entering practice in the Midwest. Most (58%, 66 respondents) were starting in a large city, followed by small city (20%, 23), suburban areas (14%, 16), and rural practice (7%, 8 fellows).
Figure 13: Location of First Post-Fellowship Positions
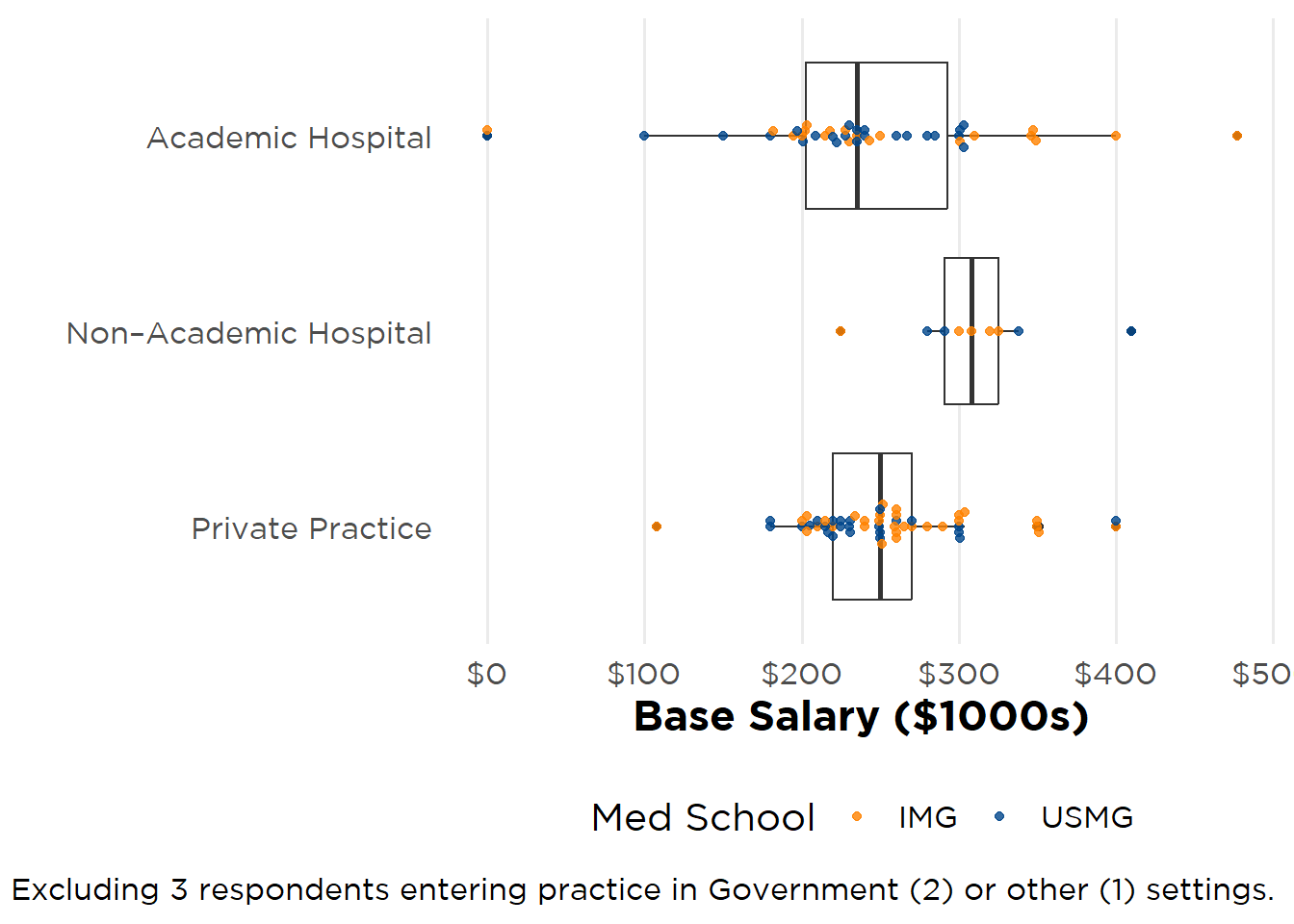
Overall median base salary for respondents’ first post-fellowship position was $249,000 (IQR $84,500), a 4% increase from the 2024 survey. Women reported a median starting salary that was $10,000 lower than men (Figure 14A and Figure 14B), and IMGs (Figure 15A) continued to report higher starting salaries than USMGs (Figure 15B). Four out of five adult fellow participants were starting in full-time (1 FTE) positions, although there was a greater percentage of men working in 1-FTE positions (86%) than women (78%). When assessing base salary per FTE ($1000s/FTE), the difference in earnings between men and women narrowed and reversed, with a mean $269,000/FTE for men and $271,000/FTE for women. This suggests structural contributors (e.g., FTE design, call expectations, institutional policies) may influence early-career earnings.
Excluding one respondent practicing in another setting, fellows employed by non-academic hospitals had the highest median starting salaries ($308,000, IQR $34,000; 9 fellows), followed by private practice ($250,000, IQR $50,000; 54), academic hospitals ($235,000, IQR $90,000; 43), and government ($222,000, IQR $72,000; 2 fellows) (see Figure 16 and Figure 17).
Figure 14A: Base Salary—Women
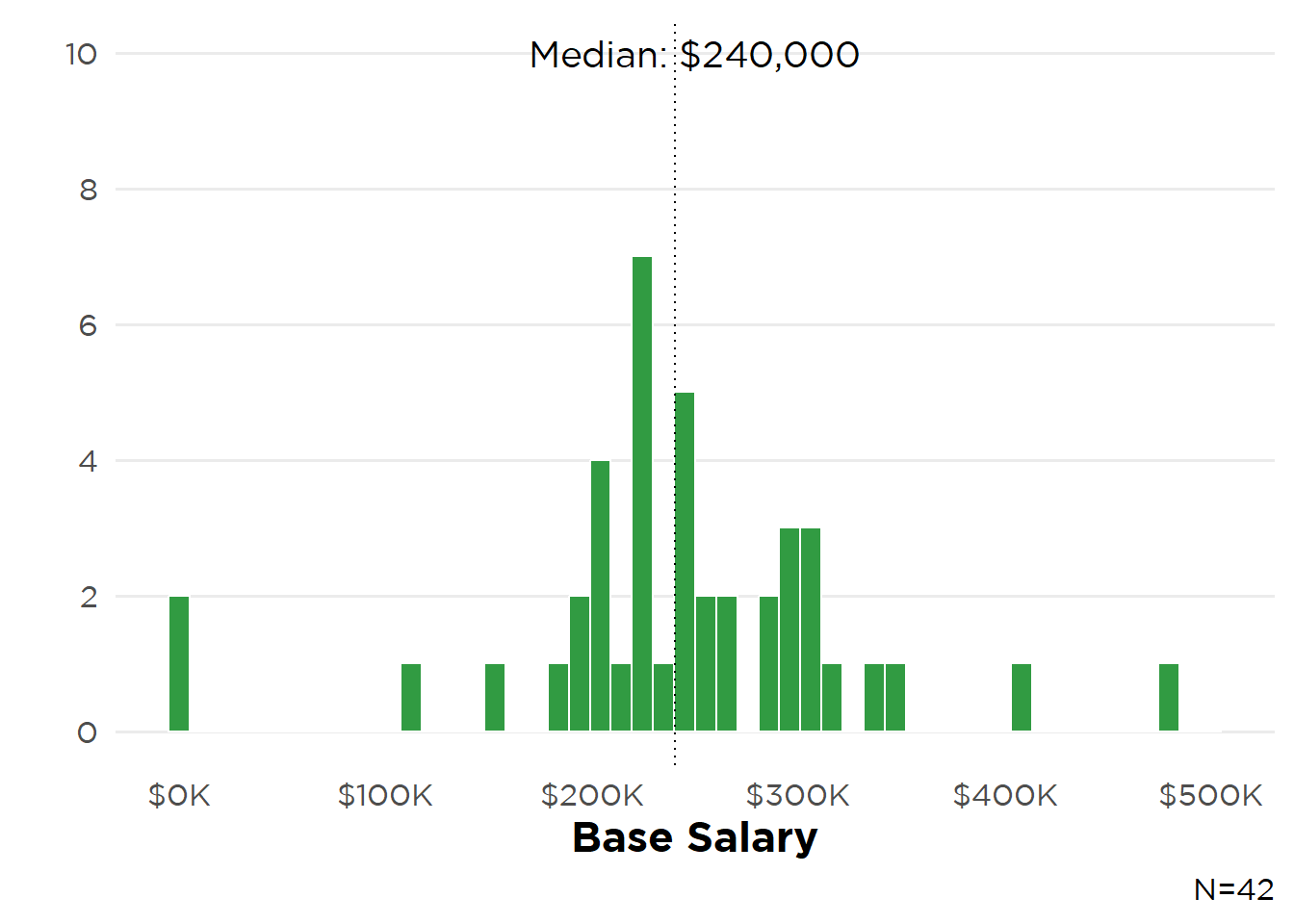
Figure 14B: Base Salary—Men
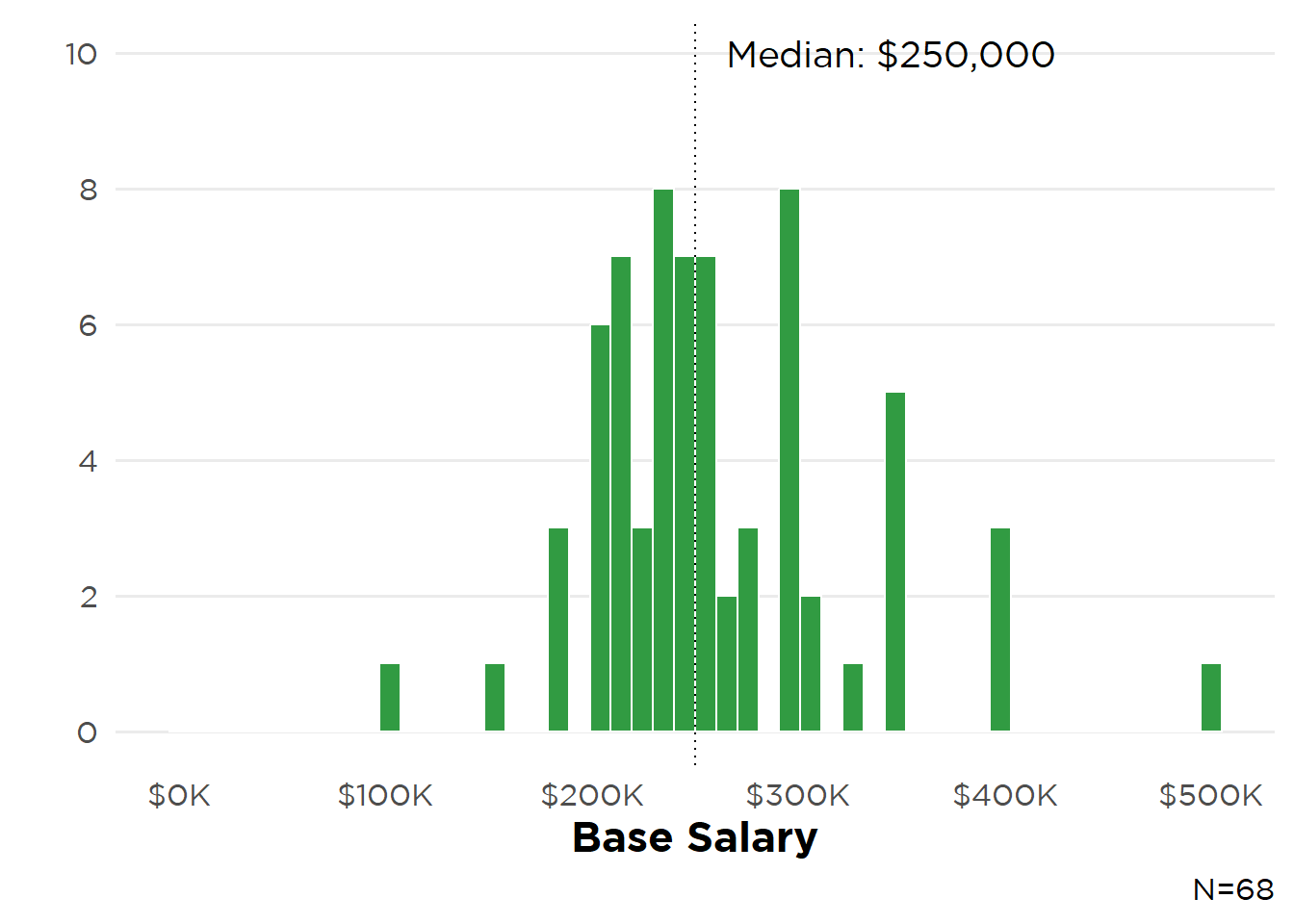
Figure 15A: Base Salary—IMGs
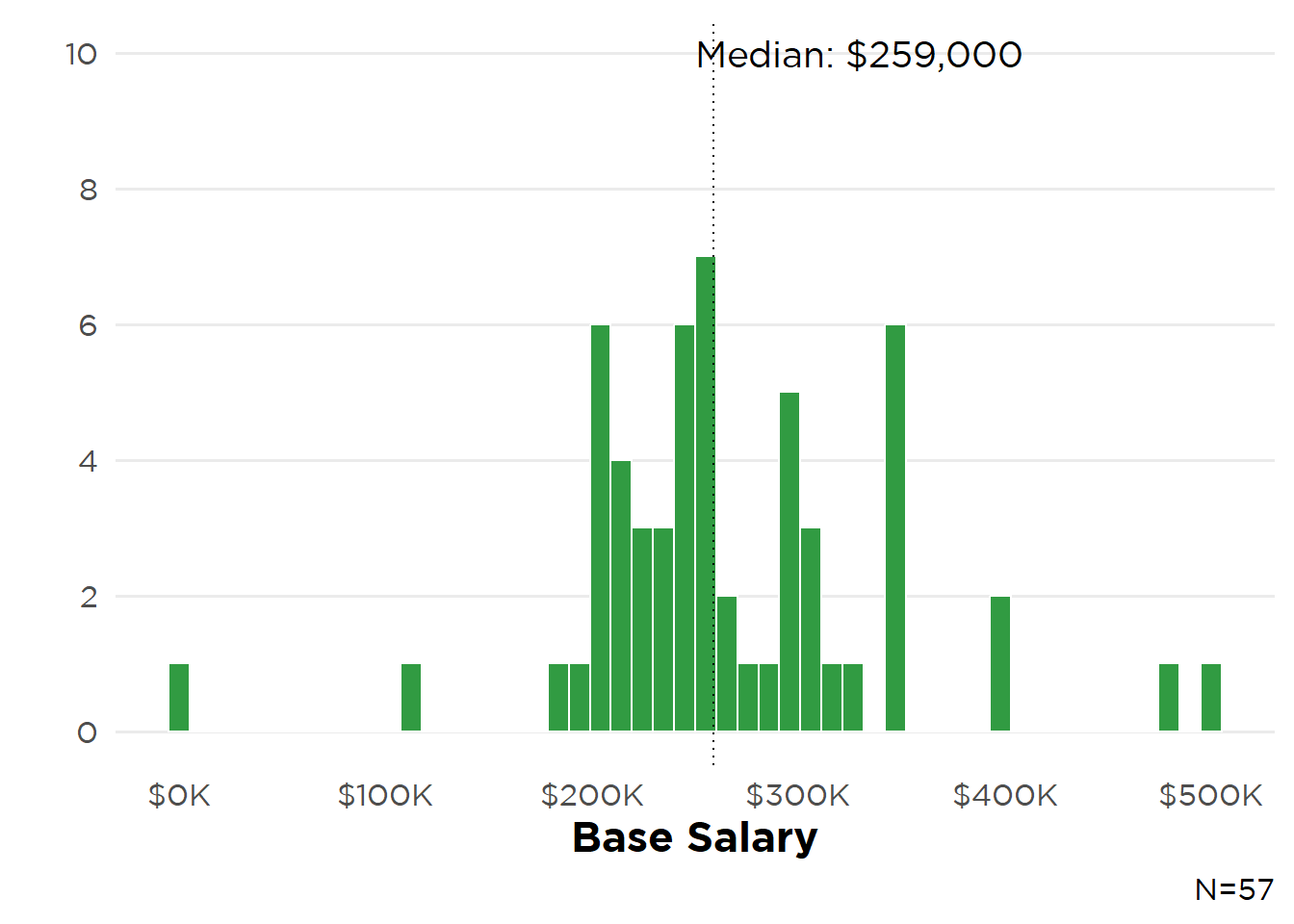
Figure 15B: Base Salary—USMGs
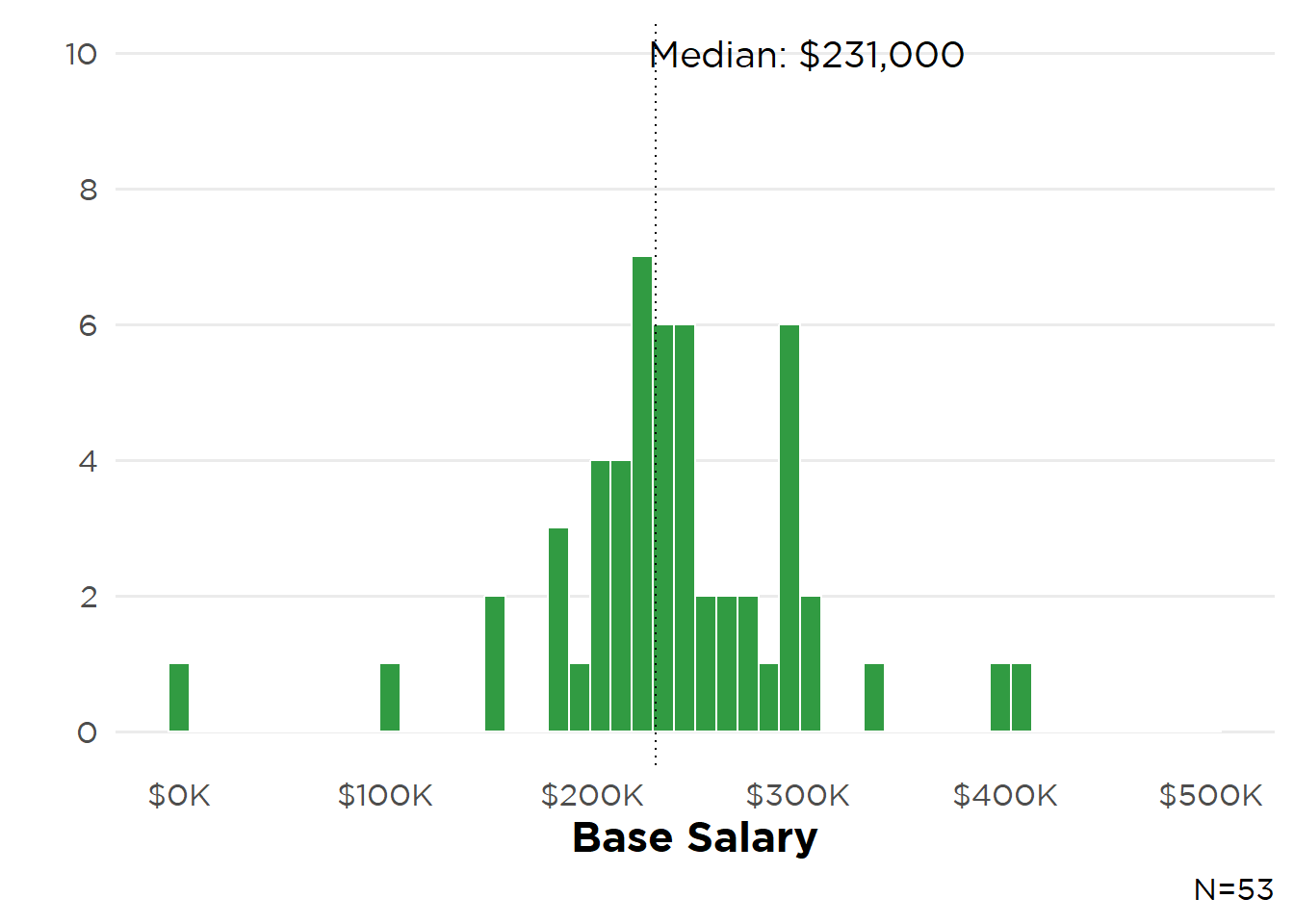
Figure 16: Base Salary—Employer and Gender
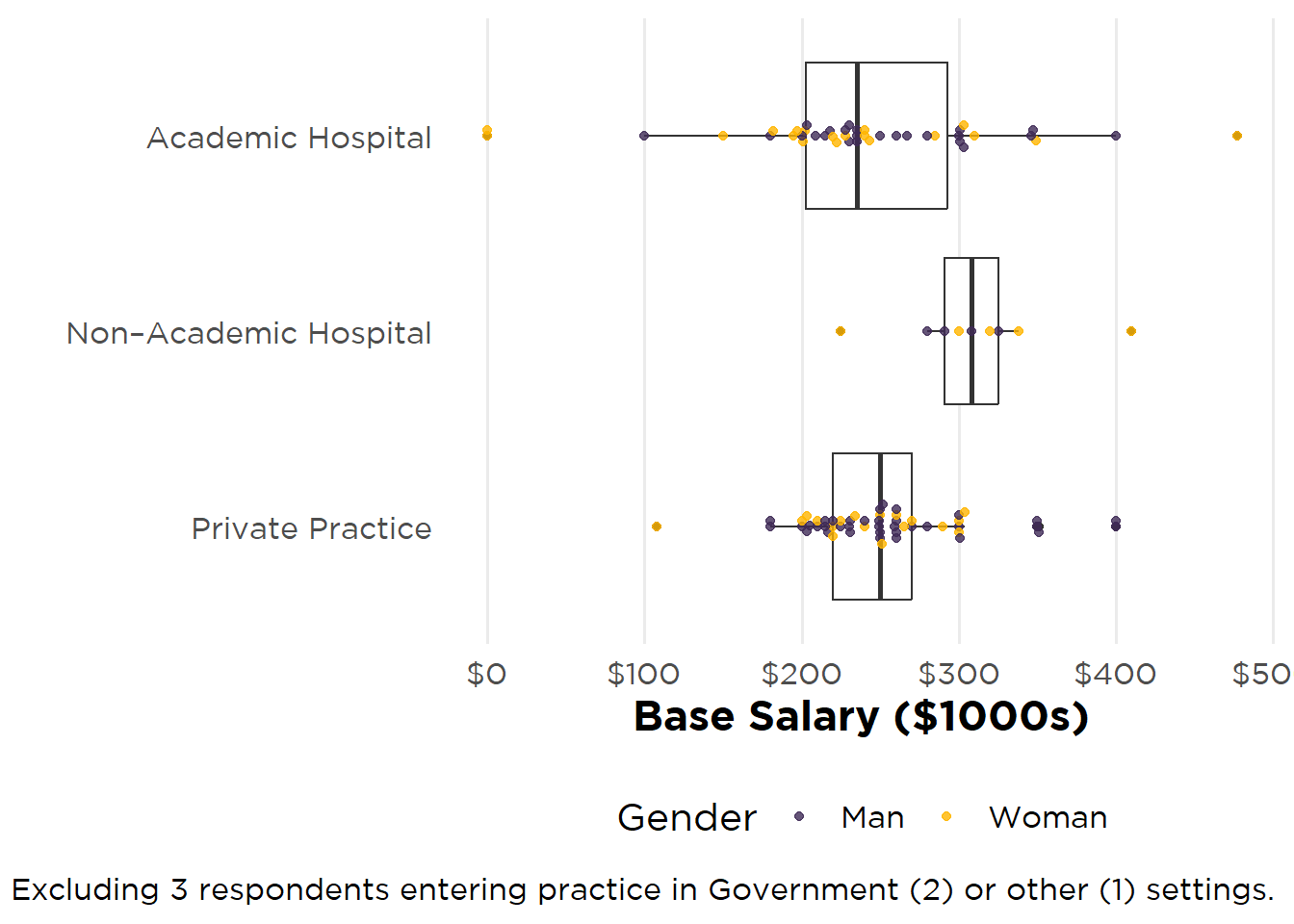
Figure 17: Base Salary—Employer and Educational Status
Fellows entering practice in the West Census Region had the highest median base starting salary ($260,000), with those starting in the South reporting the lowest median salary ($235,000) Figure 18. Although the West Region, as of Q2 2025 has the highest Employment Cost Index (ECI), there was no geographic concordance between base starting salary and ECI in the remaining Census Regions.
Figure 18: Base Starting Salary by Census Region
| Region | Median (IQR) | N | |
|---|---|---|---|
| West | $260,000 ($72,500) | 23 | |
| Midwest | $250,000 ($48,750) | 22 | |
| Northeast | $240,500 ($86,000) | 31 | |
| South | $235,000 ($57,000) | 38 |
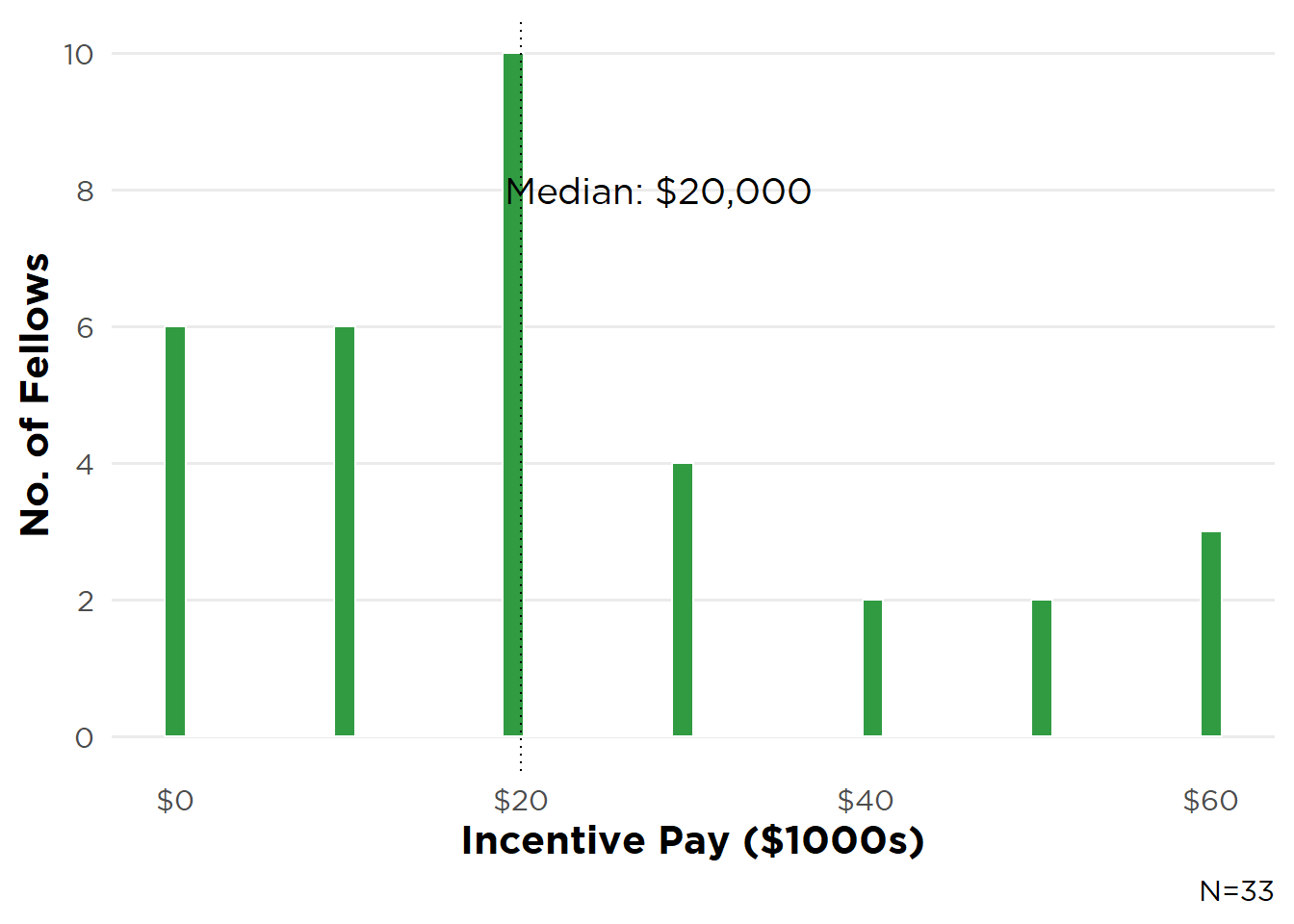
Malpractice insurance, a signing bonus, income guarantees, and MOC and CME support were the top four incentives fellows reported receiving again this year (Table 7). Nearly two-thirds (61%) indicated that incentives received were “Very”/“Extremely” important in choosing their position (Figure 19). Overall median bonus/incentive pay was $20,000 (71 fellows) with little variation based on gender (Figures 20A and 20B) and medical school location (Figures 21A and 21B).
Table 7: Incentives Received
| Incentive | N (%)* |
|---|---|
| Malpractice Insurance | 70 (64%) |
| Sign-on bonus | 58 (53%) |
| Income guarantees | 54 (49%) |
| MOC/CME | 51 (46%) |
| Relocation allowances | 48 (44%) |
| Career development opportunities | 47 (43%) |
| Flexible schedule | 28 (25%) |
| Quality-Metric bonus payments | 27 (25%) |
| H-1 visa sponsorship | 19 (17%) |
| J-1 visa waiver | 17 (15%) |
| On-call/moonlighting payments | 11 (10%) |
| On-call payments | 6 (5%) |
| Protected time for research/research “start-up” package | 5 (5%) |
| Loan repayment | 4 (4%) |
| Spouse/partner job transition assistance | 3 (3%) |
| Other | 3 (3%) |
| Real estate venture | 2 (2%) |
| Educational loan repayment | 2 (2%) |
| *N=110 | |
Figure 19: Importance of Incentives
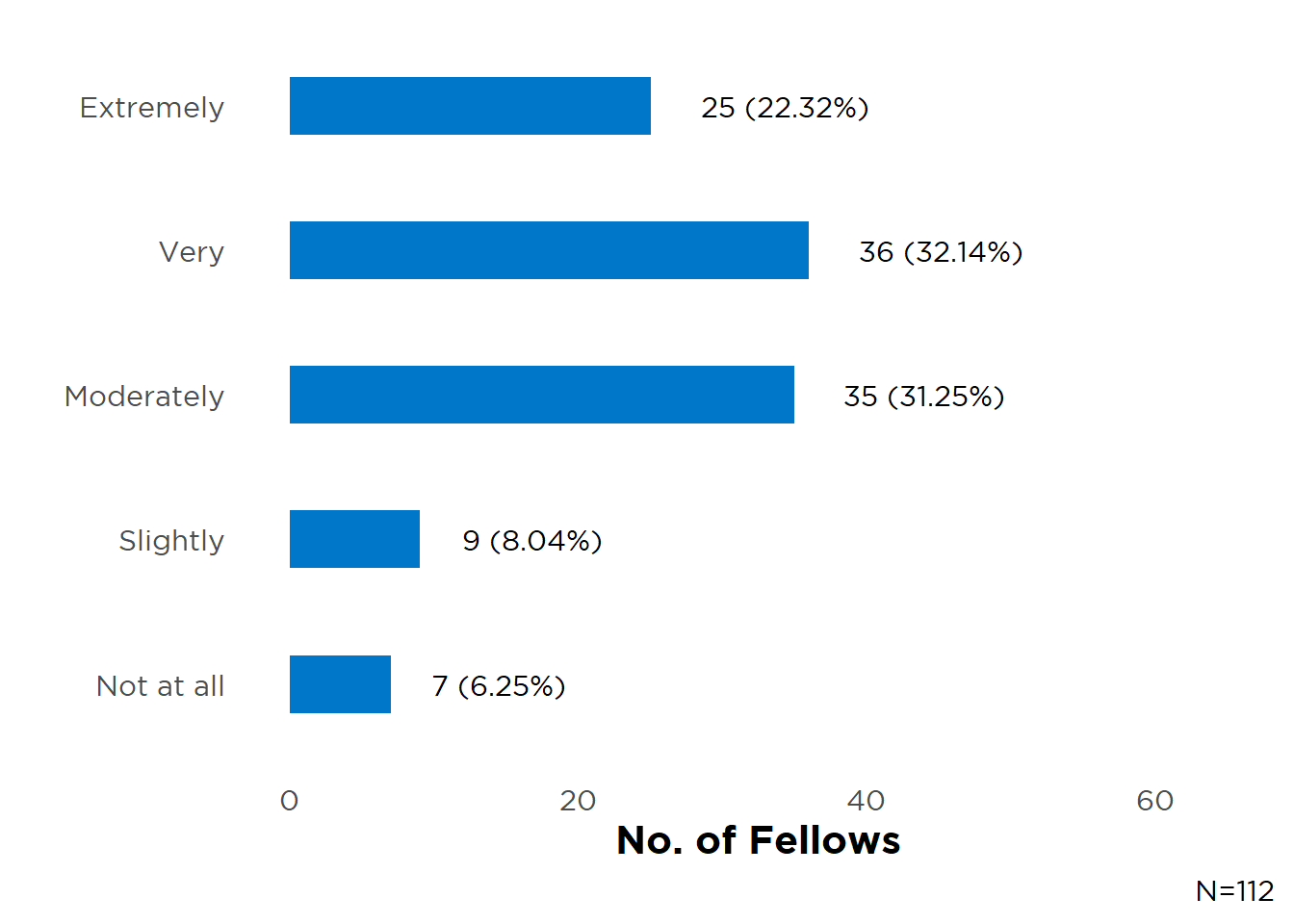
Figure 20A: Incentive Pay—Women
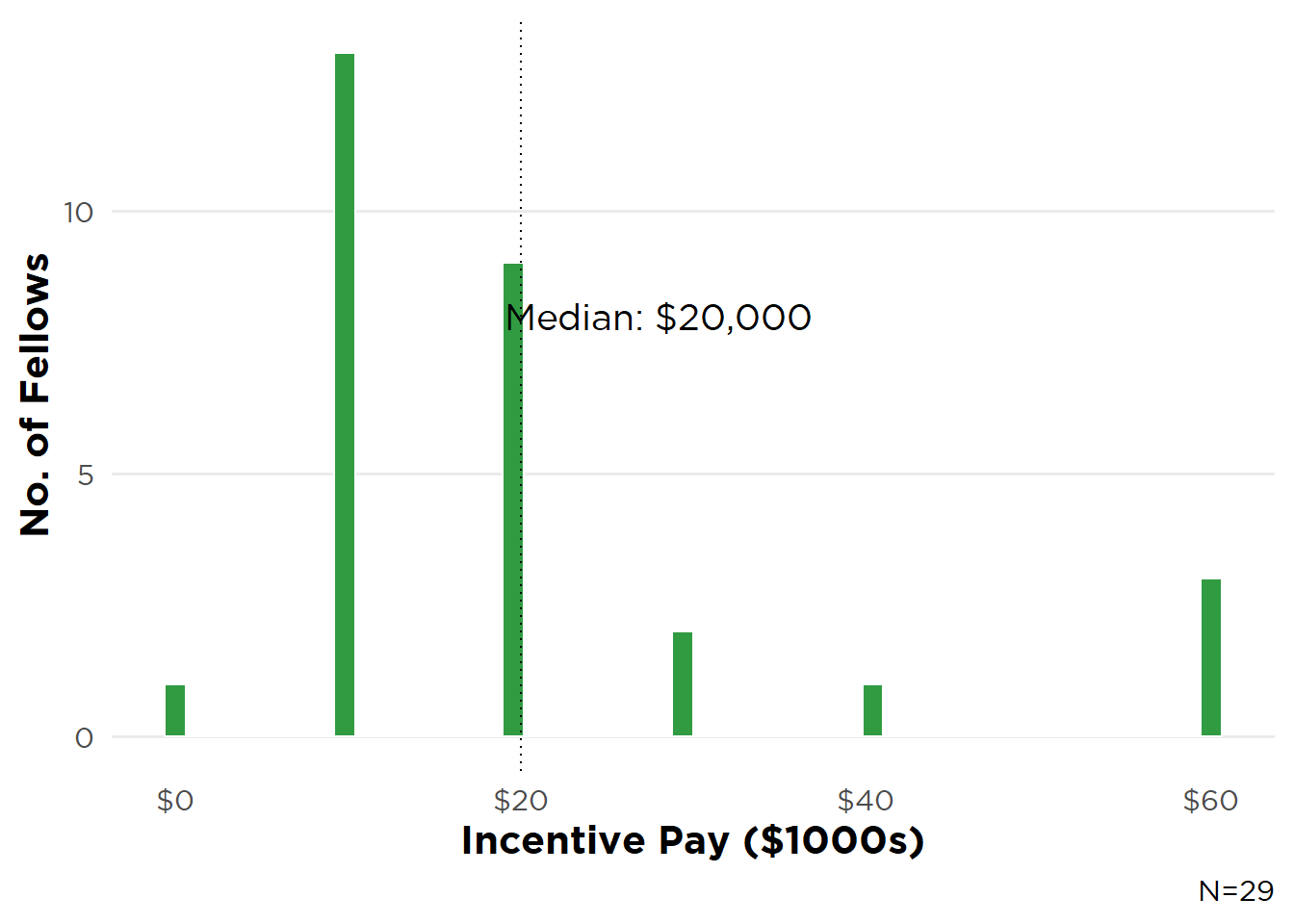
Figure 20B: Incentive Pay—Men
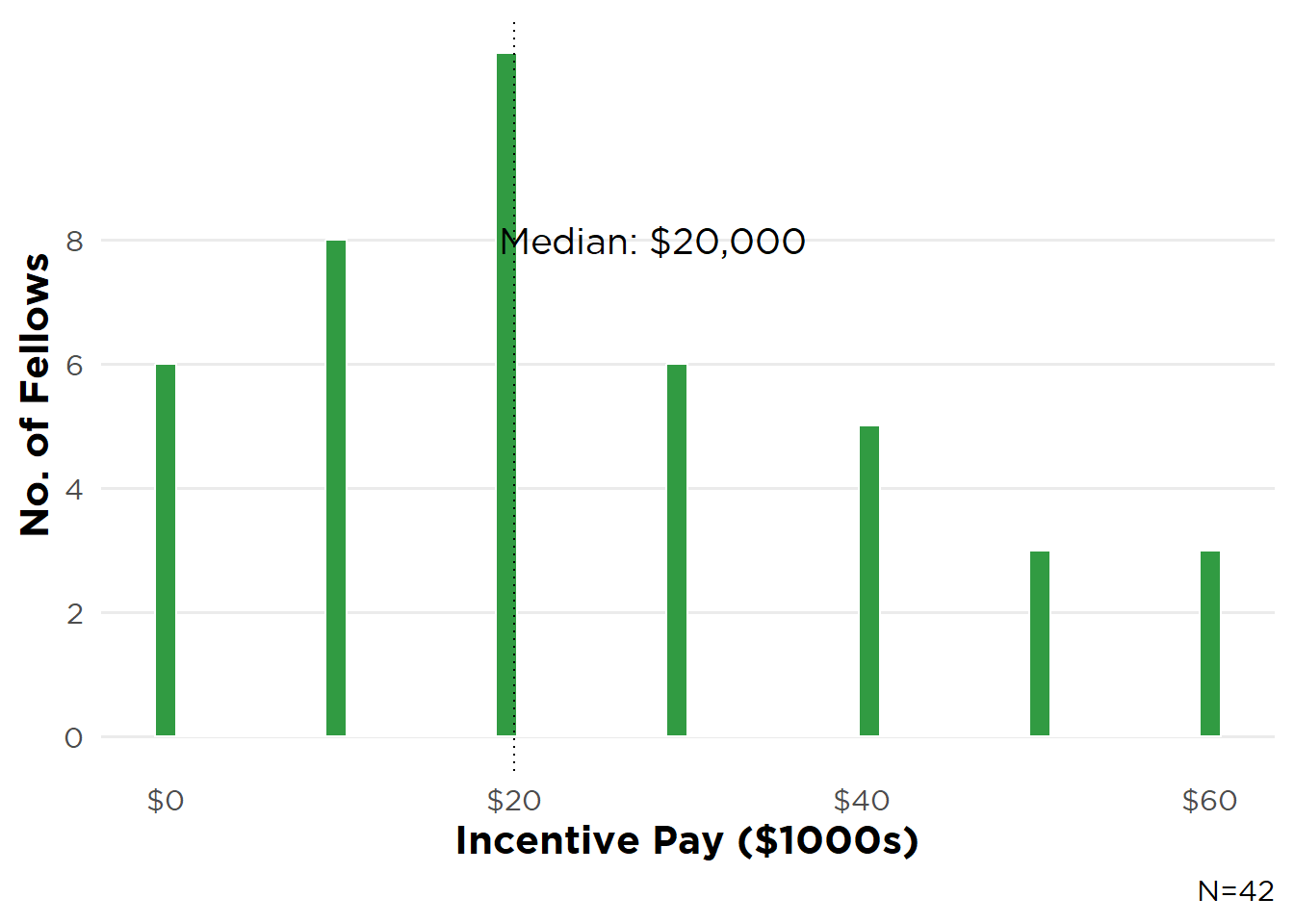
Figure 21A: Incentive Pay—IMGs
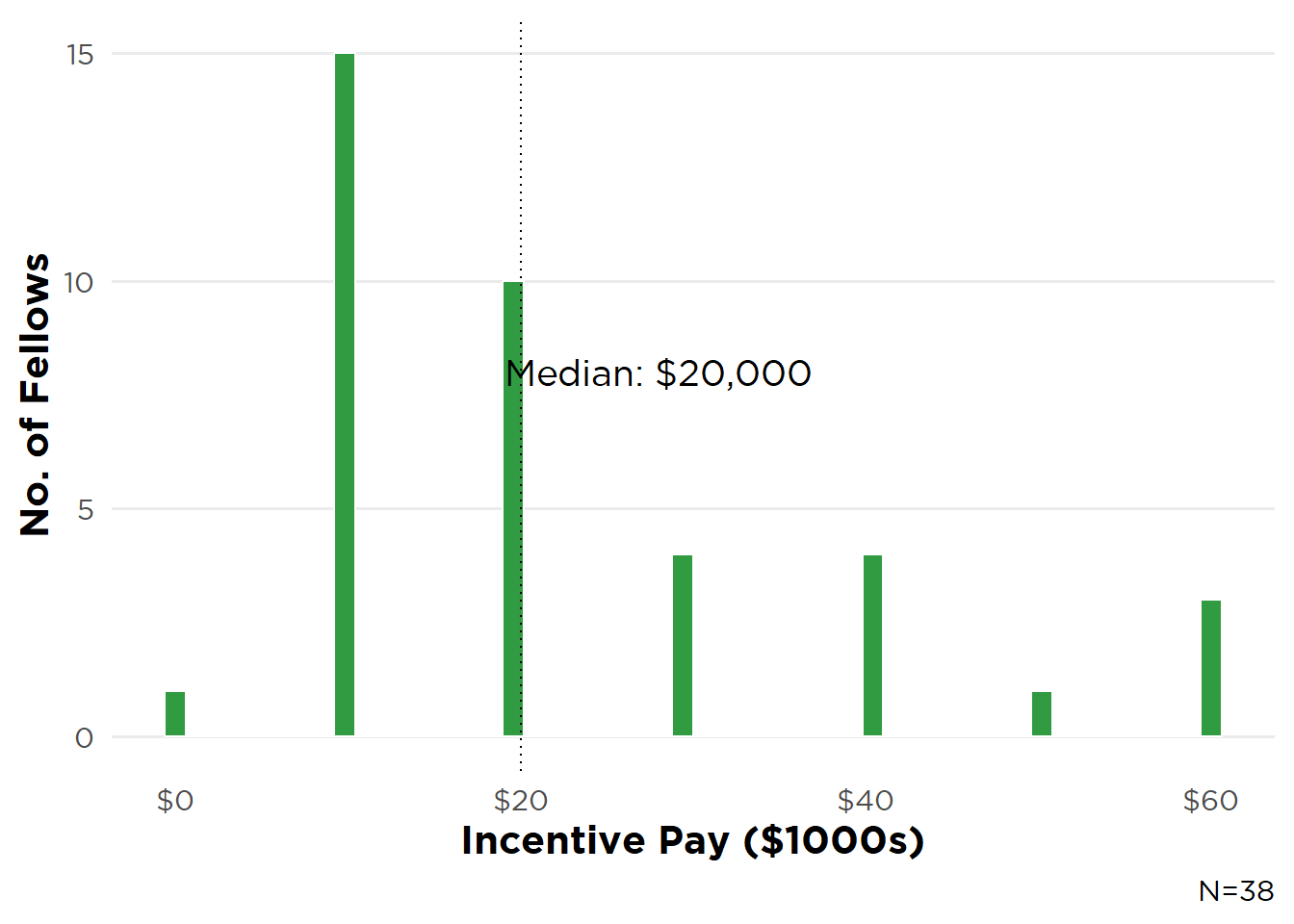
Figure 21B: Incentive Pay—USMGs
V. Pediatric Nephrology Fellows
V.1 Pediatric and Adult/Pediatric Fellow Demographics
This year 48 of 106 current pediatric fellows (45%) and 2 adult/pediatric fellows participated in the survey. Most pediatric fellow participants were USMGs (72%), women (70%), U.S. Citizens (87%), and non-Hispanic Whites (48%; see Table 1). Compared with the most recent ACMGE data on pediatric fellows, there were fewer Hispanic/Latina/Latino and more Asian and Black/African American respondents (Table 2). USMG pediatric respondents were mainly graduates of allopathic medical schools (91%, 32 fellows).
V.2 Educational Debt
Both pediatric and adult/pediatric participants reported carrying a higher debt burden than adult respondents. Median debt was $220,000 for pediatric and $393,000 for adult/pediatric fellows versus $165,000 for adult fellows. Similar to the adult cohort, a majority of pediatric fellows chose nephrology during their PGY-2 and PGY-3 years of residency (58% vs. 44% for adults).
V.3 Future Plans
Three-quarters of respondents (36 fellows) were continuing their current fellowship, with 10 respondents entering academic practice (21%), and 2 (4%) still undecided at the time of the survey.
All but 2 pediatric respondents planned to remain in the U.S. for their first position, with a lower percentage anticipating remaining in the same state (31%) and city/region (23%) as their current fellowship than adult participants (Figure 22).
Figure 22: Planned Post-Fellowship Job Location
V.4 Job Market Perceptions
Pediatric fellow respondents have a pessimistic view of the local job market with only 29% of USMGs and 31% of IMGs indicating and appropriate number of opportunities within 50 miles of their fellowship institution (Figure 23). This could partially explain the lower percentage of pediatric fellows anticipating practicing in the same state and city/region (Figure 22). Nationally, respondents were more optimistic with 46% of IMGs and 40% of USMGs indicating an appropriate number of jobs and 15% and 20%, respectively, perceiving too many open positions (Figure 24).
Figure 23: Local Pediatric Job Market Perspectives
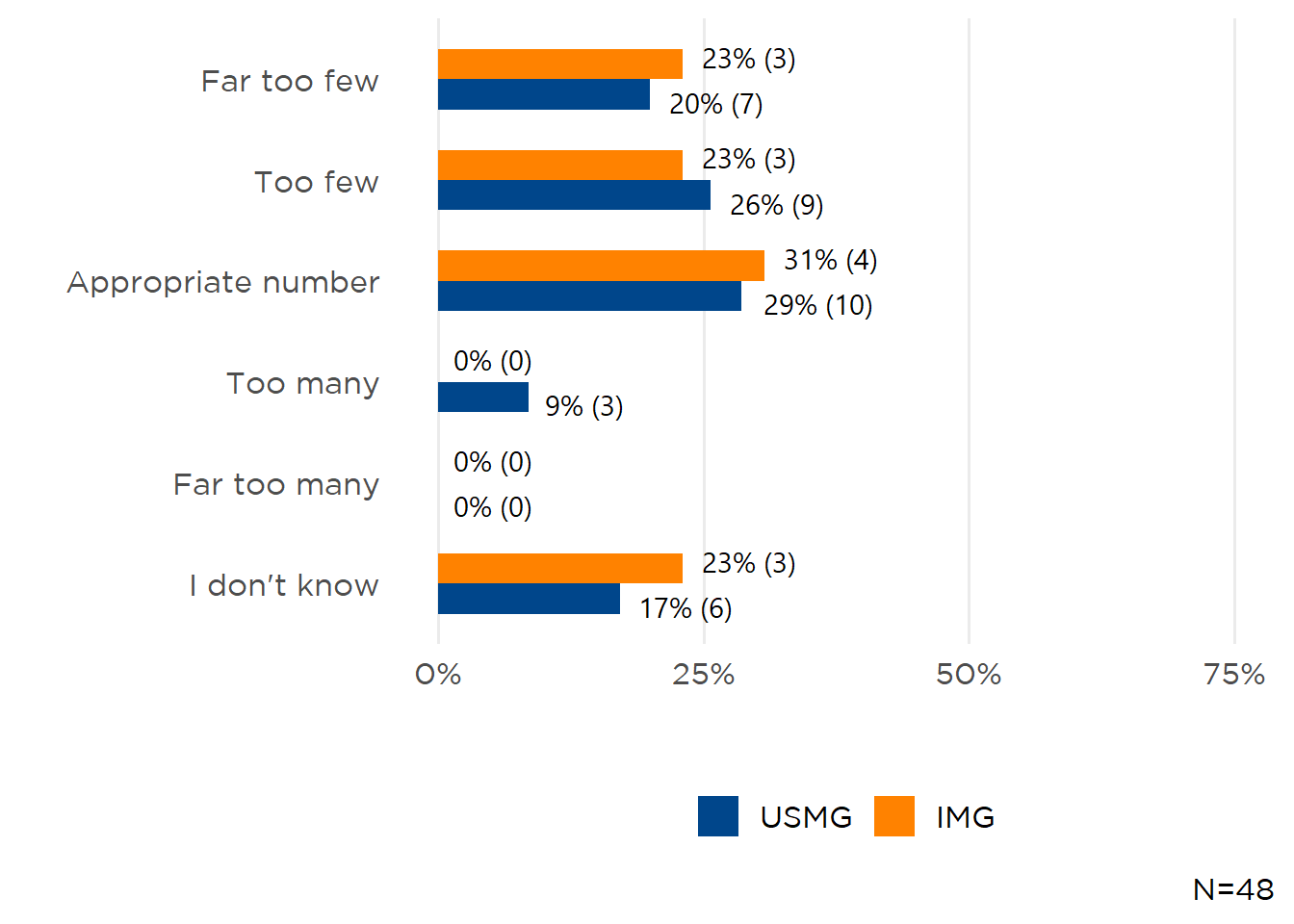
Figure 24: National Pediatric Job Market Perspectives
V.5 Entering Practice
Twelve participants had started their job search, with 10 pursuing clinical positions, 5 research positions, 3 fellows looking for a job in medical education, and 2 searching for positions combining nephrology and another specialty. Pediatric respondents applied for a median 2 positions and received a median 2 job offers. At survey time, 9 had accepted positions, 2 had received an offer but was still searching, and 1 had not received any employment offers. Unlike adult fellows, only 2 pediatric respondents had difficulty finding a position they considered satisfactory, primarily due to a lack of positions in a desired location or practice setting.
Of the 9 respondents who had accepted a position, 6 fellows were starting in clinical nephrology and 1 each in research, a combined nephrology/other specialty position, and medical education. Respondents entering pediatric nephrology practice were anticipating responsibilities for dialysis modalities (PD, CRRT, in-center HD), and outpatient and specialty clinics (Table 8). Many more pediatric respondents anticipated performing kidney biopsies (64%) than adult fellows (17%). Similarly, a greater proportion of pediatric fellows anticipated participating in clinical research (64% vs 18% of adult respondents), with only one fellow pursuing a translational research career focus and none entering basic science.
Table 8: Responsibilities in Practice
| Responsibility | N (%)* |
|---|---|
| General nephrology outpatient clinic | 11 (100%) |
| PD | 9 (82%) |
| CRRT | 9 (82%) |
| Outpatient—In-center HD | 8 (73%) |
| Kidney biopsy | 7 (64%) |
| Clinical research | 7 (64%) |
| Education | 6 (55%) |
| Transplant outpatient clinic | 4 (36%) |
| PLEX | 4 (36%) |
| Apheresis | 4 (36%) |
| Home HD | 1 (9%) |
| Nephrolithiasis specialty clinic | 1 (9%) |
| Glomerular disease specialty clinic | 1 (9%) |
| Translational research | 1 (9%) |
| *N=11 | |
Pediatric fellow respondents were starting positions in 7 states (Figure 25), and entering practice in a large urban area (10 fellows).
Figure 25: Location of First Post-Fellowship Positions
Base median starting salary was $195,500, which was a 2.8% increase from the median value of $190,000 reported in 2024 (Figure 26). Eight fellows (62%) also received incentive income ranging from $1,000 to $30,000 (median $10,000). Other incentives reported included support for malpractice insurance (90%) and career development opportunities (80%) (Table 9). More than two-thirds (70%) of pediatric fellow respondents indicated incentives were “Very Important”/“Extremely Important” in choosing their first position. Eight pediatric fellow respondents were starting in full-time positions, with 1 indicated they were 0.8 FTE.
Figure 26: Base Salary—Pediatric Fellows
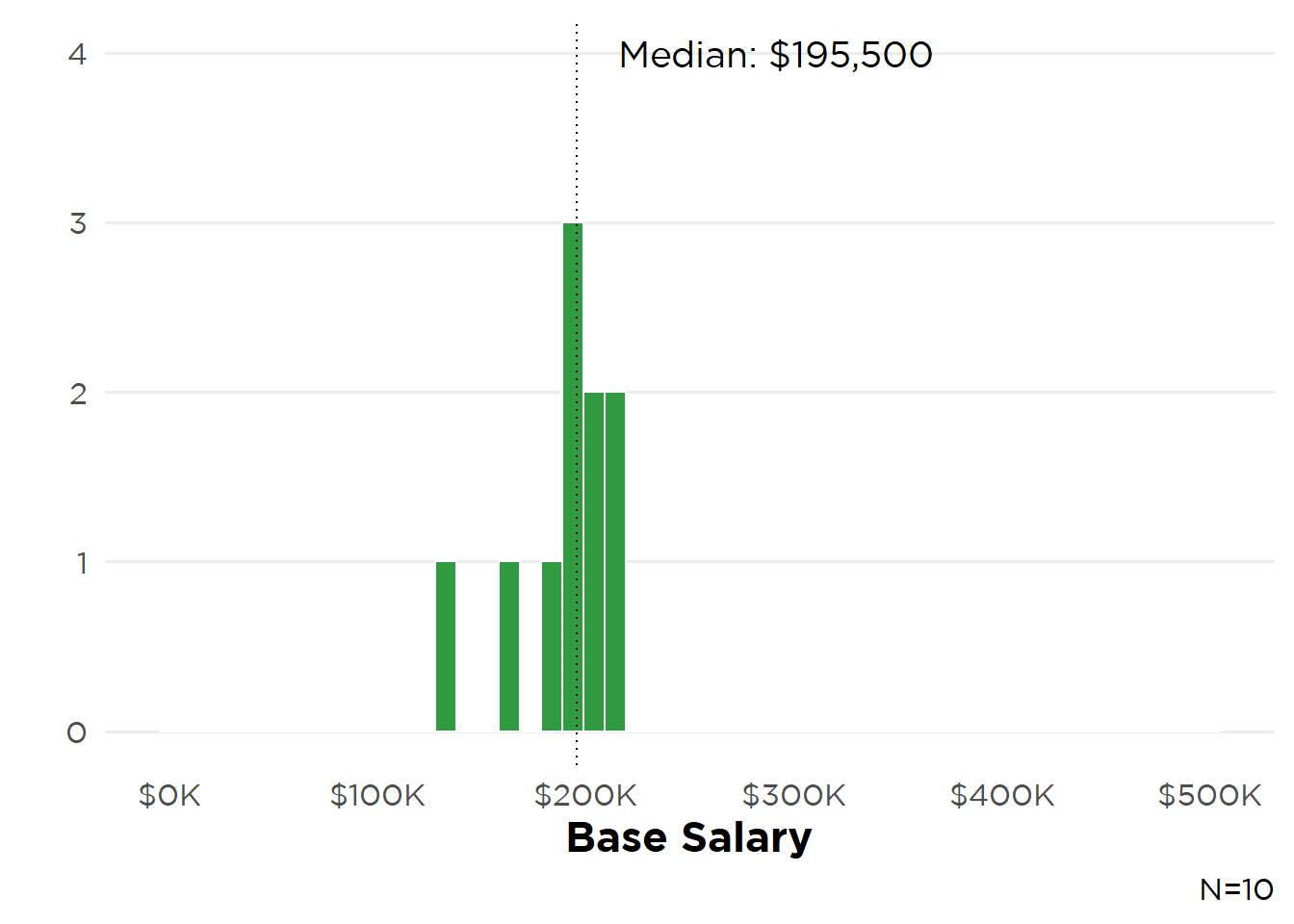
Table 9: Incentives Received
| Incentive | N (%)* |
|---|---|
| Malpractice insurance | 9 (90%) |
| Career development opportunities | 8 (80%) |
| Sign-on bonus | 7 (70%) |
| MOC/CME | 6 (60%) |
| Relocation allowances | 4 (40%) |
| Income guarantees | 3 (30%) |
| Protected time for research/research “start-up” package | 3 (30%) |
| Quality-Metric bonus payments | 3 (30%) |
| Other | 2 (20%) |
| J-1 visa waiver | 1 (10%) |
| *N=10 | |
VI. Transplant Nephrology Fellows
VI.1 Transplant Fellow Demographics
In its second year, the ASN Transplant Nephrology Fellow Survey received 15 responses, representing 25% of all current transplant fellows training in the U.S. The survey was developed to better understand transplant trainees and the job market for transplant nephrologists.
A slight majority of participating transplant fellows were IMGs (73%), women (53%), and training on J-1 visas (40%). Five respondents identified as Hispanic/Latina/Latino (33%), with half White, one-fifth South Asian, and 13% identifying as Black/African American.
VI.2 Choosing Transplant Nephrology
Most (73%) decided to subspecialize in transplant during fellowship, 2 during their 2nd or 3rd years of residency, and 1 before medical school. A majority (80%) were attracted to the science and allure of transplant nephrology, with two-thirds motivated by positive experiences during their transplant rotation (Table 10).
Table 10: Motivations to Pursue Transplant Nephrology
| Factor | N (%) |
|---|---|
| Science and allure of transplant nephrology | 12 (80%) |
| Positive experience with rotation or research in transplant | 10 (67%) |
| Inspired by mentor | 9 (60%) |
| Fulfillment in caring for post-transplant patients | 9 (60%) |
| Being part of a multidisciplinary team | 6 (40%) |
| Desire to work at an academic center post-fellowship | 4 (27%) |
| Expectation for a better lifestyle post-fellowship | 4 (27%) |
| Family reasons | 3 (20%) |
| Prestige | 2 (13%) |
| Job security | 1 (7%) |
| *N=15 | |
Sixty-seven-percent of participating fellows were very satisfied with their choice to pursue transplant, and 93% would recommend the subspecialty.
VI.3 Job Search Experiences and First Positions
Fourteen participants were searching for employment, focusing on solely transplant nephrology (6 fellows) or transplant nephrology combined with general nephrology (4 fellows). Nine participants had accepted an employment offer and 5 had received an offer but were still searching for a position. Five fellows experienced difficulty finding a position they considered satisfactory because of visa requirements (n=5), lack of positions in a desired location (n=4) or practice setting (n=2), or inadequate salary (n=2).
Of the 14 participants entering their first post-fellowship position, 53% were focused solely on transplant nephrology, with 20% entering combined transplant/general nephrology practice, 13% starting a general clinical nephrology position, and 7% in another type of position. Eleven respondents were starting in an academic hospital/health system, 2 in a non-academic/independent transplant center, and 1 in private practice. Of the 12 participants reporting base starting salary, the overall median was $256,000 (IQR $39,000) (Figure 27). Yet base salary varied by practice type: respondents starting in dedicated transplant positions reported a median $252,000 (IQR $52,500), those in joint transplant/general nephrology a median $230,000 (IQR $30,000), and those entering general nephrology a median $312,000 (IQR $37,500). Thirteen will oversee post-transplant clinics and 12 outpatient transplant clinics (Table 11).
Table 11: Transplant Nephrology Fellows: First Post-Fellowship Employment Responsibilities
| Responsibility | N (%)* |
|---|---|
| Post-transplant clinic | 13 (93%) |
| Outpatient clinic—transplant | 12 (86%) |
| Recipient evaluation | 10 (71%) |
| Fellow, resident or medical student education | 10 (71%) |
| Living donor evaluation | 9 (64%) |
| Inpatient transplant service for kidney and/or pancreas transplant recipients | 9 (64%) |
| Inpatient general nephrology service | 6 (43%) |
| Waitlist management | 5 (36%) |
| Inpatient service for other organ transplant recipients with kidney issues | 5 (36%) |
| Kidney biopsy | 4 (29%) |
| Satellite clinics—One state licensure | 4 (29%) |
| Outpatient clinic—CKD | 4 (29%) |
| Quality Improvement Program | 3 (21%) |
| Clinical research | 3 (21%) |
| Outpatient clinic—other specialty (e.g., GN, stones, hypertension) | 3 (21%) |
| Outpatient in-center hemodialysis | 3 (21%) |
| PD | 3 (21%) |
| PLEX/Apheresis | 3 (21%) |
| Living donor transplant program | 2 (14%) |
| Patient education | 2 (14%) |
| Home HD | 2 (14%) |
| Satellite Clinics—multi-state licensure | 1 (7%) |
| Organ offer call | 1 (7%) |
| Dialysis catheter placement | 1 (7%) |
| POCUS | 1 (7%) |
| Medical directorship with a dialysis provider | 1 (7%) |
| Other (please specify) | 1 (7%) |
| Contribute to Hispanic Program | 1 (7%) |
| *N=14 | |
Figure 27: Base Salary—Transplant Nephrology Fellows
Methods
Why does ASN survey nephrology fellows in training?
Since 2014, ASN has conducted an annual fellow survey to understand:
- The composition of the incoming workforce, including race, ethnicity, and gender
- Motivating factors for choosing the specialty to tailor approaches to sustain interest in nephrology
- Potential gaps in nephrology education
- Demand for nephrologists in the U.S.
How was the survey constructed?
The survey instrument comprised:
- Longitudinal questions drawn from the original 2014 survey focusing on job search experiences, perceptions of the specialty, practice patterns, and demographics
- Questions developed by the ASN Data Subcommittee to assess nephrology fellows’ training experiences and perceptions of the specialty.
The final instrument was piloted by ASN Data Subcommittee members and distributed via Qualtrics.
Who were surveyed?
The 2025 ASN Nephrology Fellow Survey was disseminated to a survey frame of 996 adult, pediatric, and adult/pediatric nephrology fellows drawn from the ASN (891 adult fellows) and American Society for Pediatric Nephrology (105 fellows) member databases. The survey received a 39% response rate, with participation from 339 adult, 46 pediatric, and 2 adult/pediatric fellows in training.
A separate ASN Transplant Nephrology Fellow Survey was distributed to 22 transplant fellows provided by current transplant fellowship TPDs. Of these, 15 participated (68% response rate).
Although this survey captures physician trainee perspectives, nephrology workforce planning should also consider advanced practice providers (APPs), nurse practitioners and physician associates, who are increasingly central to care delivery in dialysis, CKD, and transplant settings. Future reports may benefit from framing fellow trends alongside APP integration to reflect team-based care.
When was the survey conducted?
Invitation emails were sent to adult fellows on April 29 and the survey closed on May 22, 2025. Participating fellows were eligible to win one of 10 complimentary one-year ASN memberships or one of two complimentary BRCU registrations.
How were responses analyzed?
The ASN Nephrology Fellow Survey was reviewed and approved by the Johns Hopkins University School of Medicine Institutional Research Board (Study # 00205206). Data obtained from 2025 responses were analyzed using R (R Core Team (2025). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/.).
Citation
@online{a._pivert2025,
author = {A. Pivert, Kurtis and A. Balogun, Rasheed and Chowdhury,
Raad and Edwards, Angelina and Ann Lim, Mary and Mullane, Ryan and
A. Neyra, Javier and Raslan, Rasha and Saum, Keith and Smith, Leah
and M. Sozio, Stephen and Triozzi, Jefferson and K. Weidemann, Darcy
and M. Boyle, Suzanne},
title = {2025 {ASN} {Nephrology} {Fellow} {Survey:} {First} {Look}},
date = {2025-09-29},
url = {https://data.asn-online.org/posts/2025_fellow_survey/},
doi = {10.70093/f73153320},
langid = {en}
}
