Early Career Nephrologists: Results of a 2017 Survey
Practice Setting is a Major Factor Influencing Educational Pathways and Career Satisfaction
Leo Quigley, MPH
Edward Salsberg, MPA, FAAN
George Washington University Health Workforce Institute and School of Nursing
Ashté Collins, MD
George Washington University School of Medicine
Executive Summary
Since 2014 the George Washington University Health Workforce Institute (GW-HWI) in collaboration with the American Society of Nephrology (ASN) has surveyed nephrology fellows, tracking their transition to practice and their experience in the job market. In 2017, GW-HWI surveyed recent fellowship graduates to explore the practices, satisfaction and view of the specialty of early career nephrologists.
GW-HWI surveyed nephrologists who had completed their nephrology training between 2011 and 2016. There were 270 valid responses (an 11% response rate). While this response rate is low, a comparison with ACGME data on recent nephrology fellows indicates that the characteristics of respondents are generally consistent with the characteristics of recent graduates. The responses provide a good picture of the early career nephrologist.
After reviewing the results by gender, location/type of education (US medical graduates [USMGs] vs international medical graduates [IMGs]), length of time since graduation and practice setting, it appears that practice setting—those in academic practice compared to those in a group practice—is a major factor influencing educational pathways, current practice characteristics and satisfaction. The following are key findings related to the differences between nephrologists in academic practice and those in group practice.
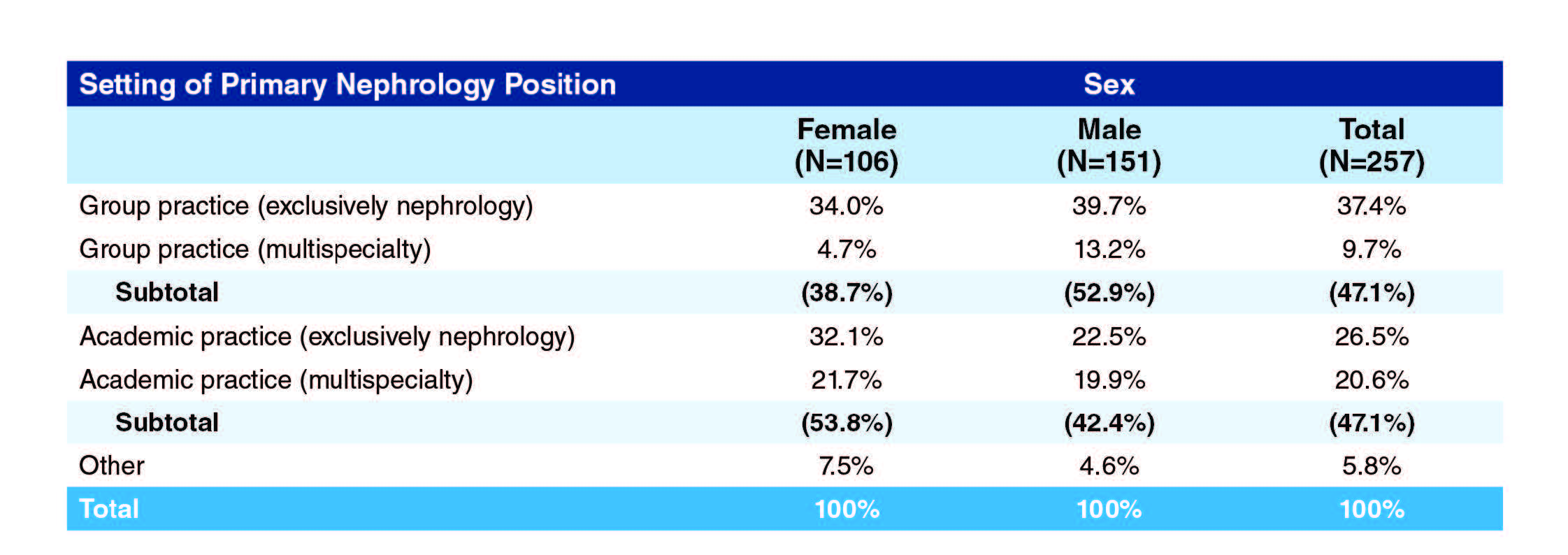
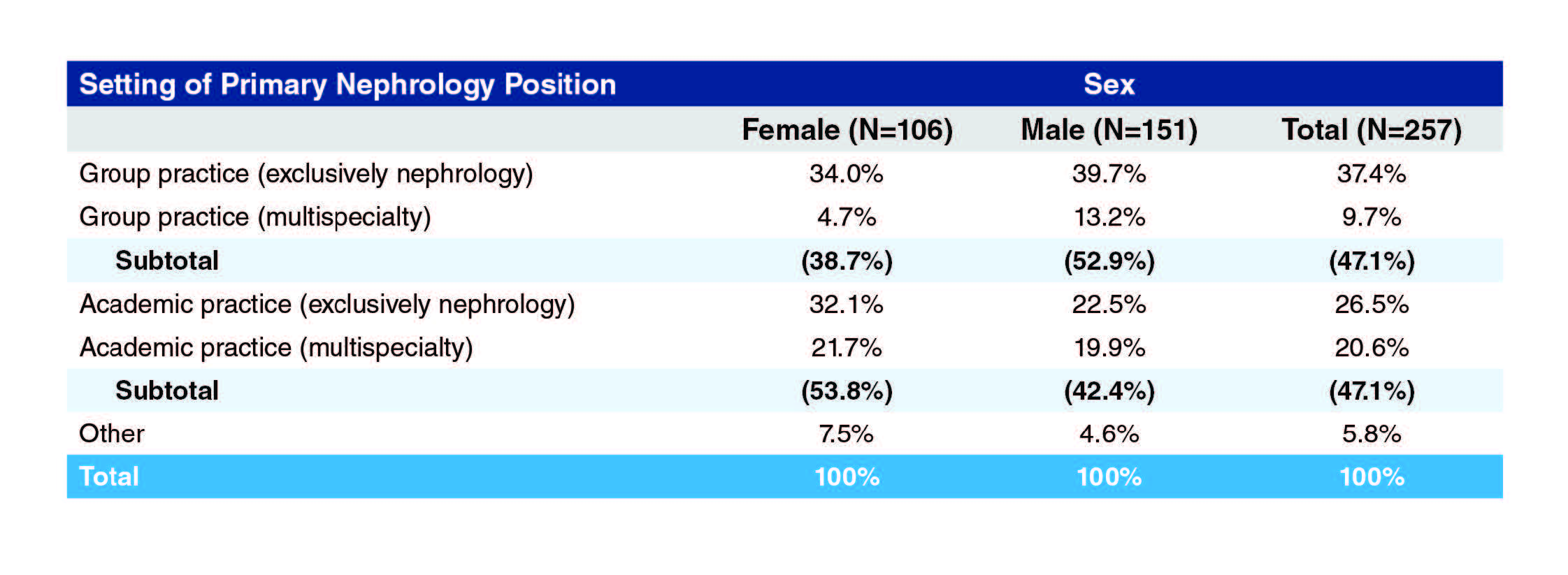
- An equal number of respondents were working in group practices and academic settings. Early practice female nephrologists are more likely to practice in academic settings than group practice settings (53.8% to 38.7%). Early practice male nephrologists, on the other hand, are less likely to practice in academic settings and more likely to practice in group settings (42.4% to 52.9%).
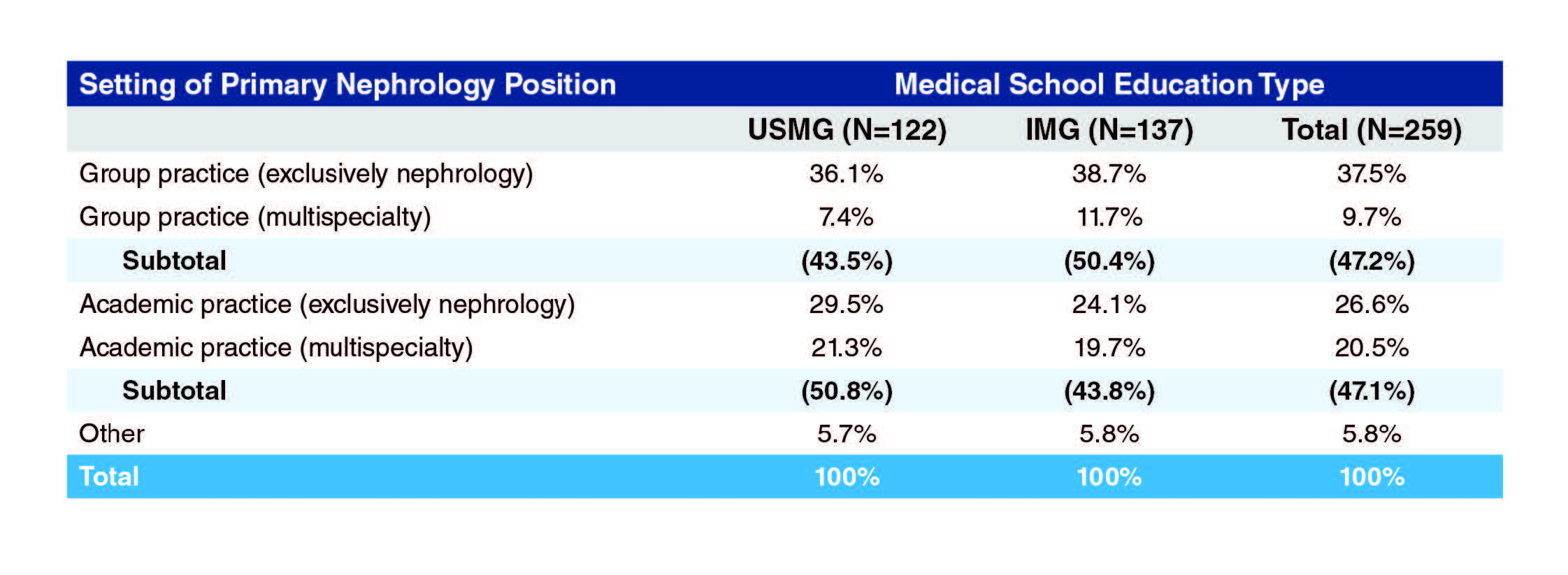
Similarly, USMGs among the early practice nephrologists are more likely to practice in academic settings than group practice (50.8% to 43.5%) while IMG early practice nephrologists are less likely to practice in academic settings and more likely to practice in groups (43.8% to 50.4%).
Academic practitioners are far more likely to have had 3 or more years of nephrology fellowship training than group practice nephrologists (48.4% to 14%). Academic physicians are more likely to have had additional training in clinical research (37.4% vs. 16.3%); basic science research (19.8% vs. 14%); and transplant nephrology (31.9% vs. 20.9%). Group practice nephrologists were more likely to have had training in interventional nephrology (20.9% to 4.4%) and palliative care (9.3% to 4.4%).
Both academic and group practice nephrologists were generally satisfied with their education and training with only 3.3% of each group expressing any dissatisfaction.
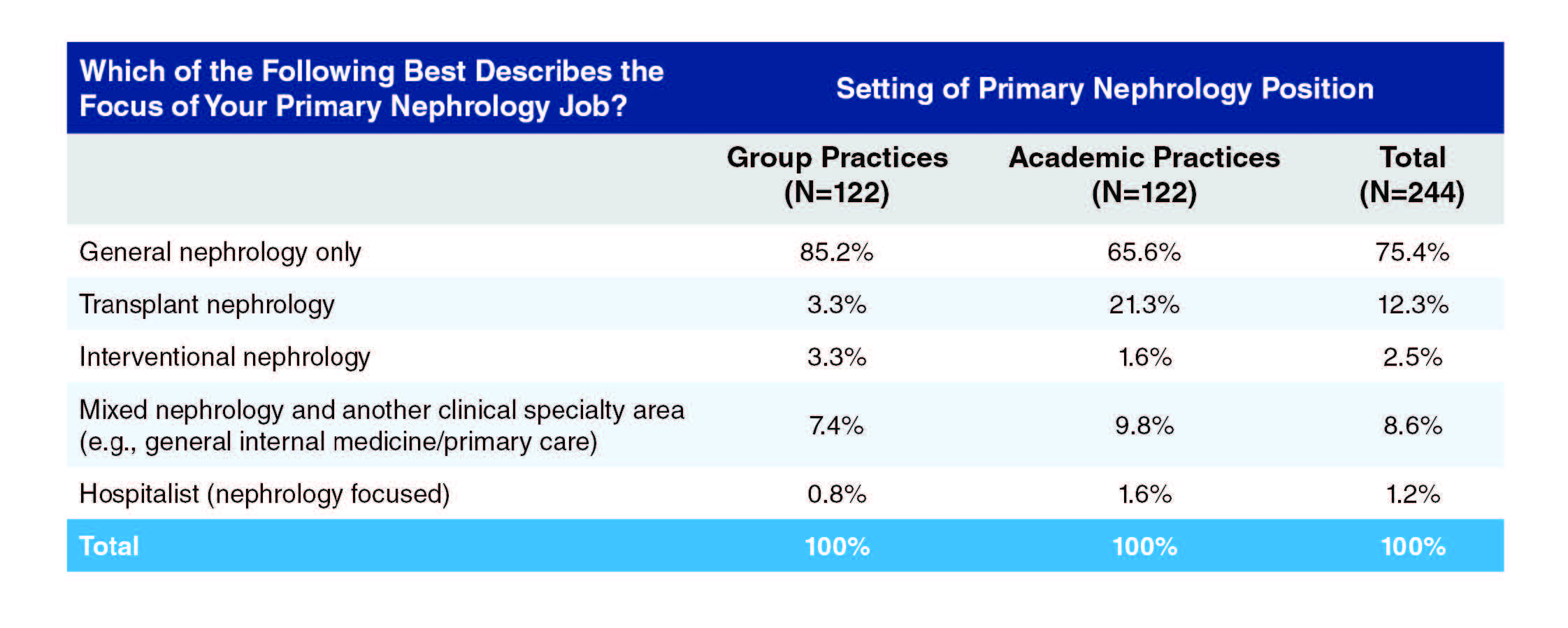
Not surprising, academic nephrologists were far more likely to focus on transplant than group practice nephrologists (21.3% to 3.3%). The majority of nephrologists practice general nephrology only: 85.2% of the group practice nephrologists and 65.6% of the academic nephrologists.
By far the most common job responsibilities were care of hospitalized patients (96.1% of respondents), care of patients in the clinic (93.8%) and care of patients in an outpatient dialysis unit (78.7%). Those in academic practices were more likely than those in group practices to have responsibility for kidney biopsies (48.4% vs. 9.1%), dialysis catheter placement (34.4% vs. 19.8%) and clinical research (57.4% vs. 8.3%), while those in group practices were more likely than those in academic practices to have responsibility for care of patients in an outpatient dialysis unit (90.1% vs. 69.7%) or in a nursing home or rehabilitation unit (34.8% vs. 22.5%) or to hold a medical directorship with a dialysis provider (33.9% vs. 15.6%).
*Percentages are of those responding to any part of this question
As would be expected, the vast majority of group practice nephrologists have a path to partnership (77%), while this is rare for those in academic practice (5.7%).
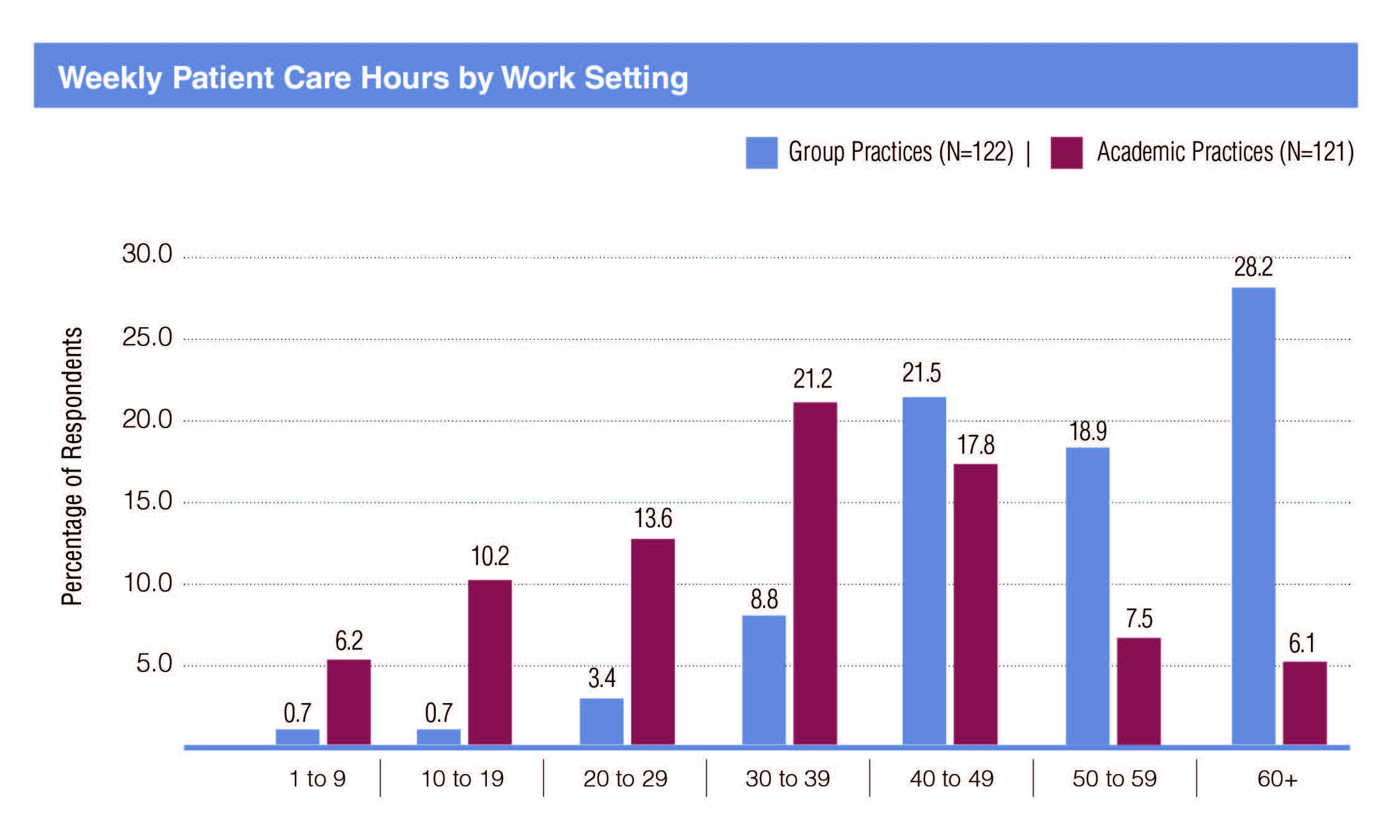
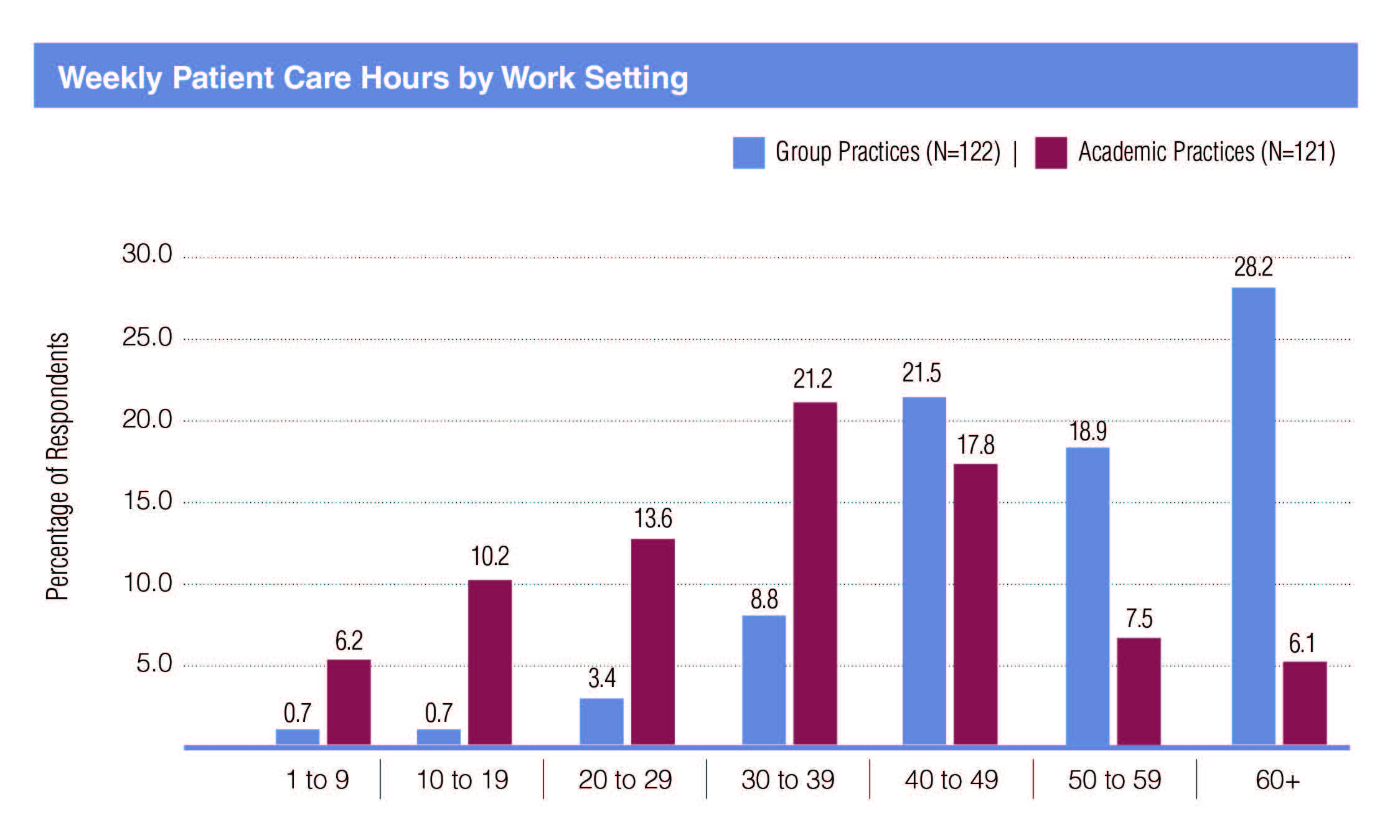
Group practice nephrologists work far more patient care hours per week than academic nephrologists: 57.4% of group nephrologists provided 50 or more hours of patient care per week compared to 16.5% of academic nephrologists. Academic nephrologists provided more hours per week on research than group practice nephrologists.
In general, nephrologists working in group practices received more incentives to join their current practice compared to academic nephrologists including: sign-on bonuses (28% to 5.1%); income guarantees (33.1% to 16.9%); relocation allowance (34.7% to 20.3%); support for MOC preparation (53.4% to 40.7%); and J-1 visa waivers (6.6% to 3.4%). On the other hand, academic physicians were more likely to receive support for career development opportunities (37.3% to 16.9%); H-1 Visa sponsorships (18.6% to 13.6%); and on-call payments (5.9% to 2.5%).
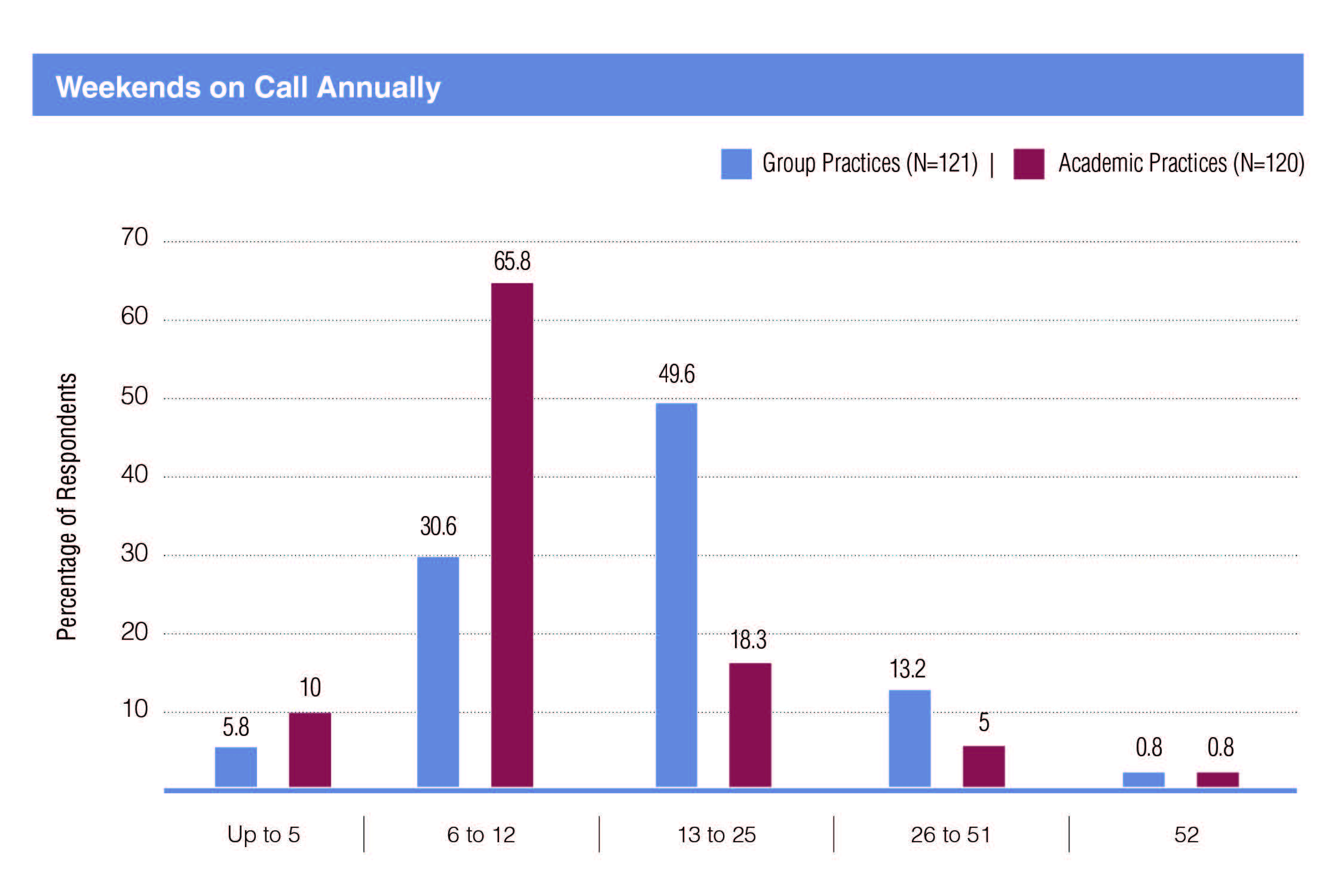
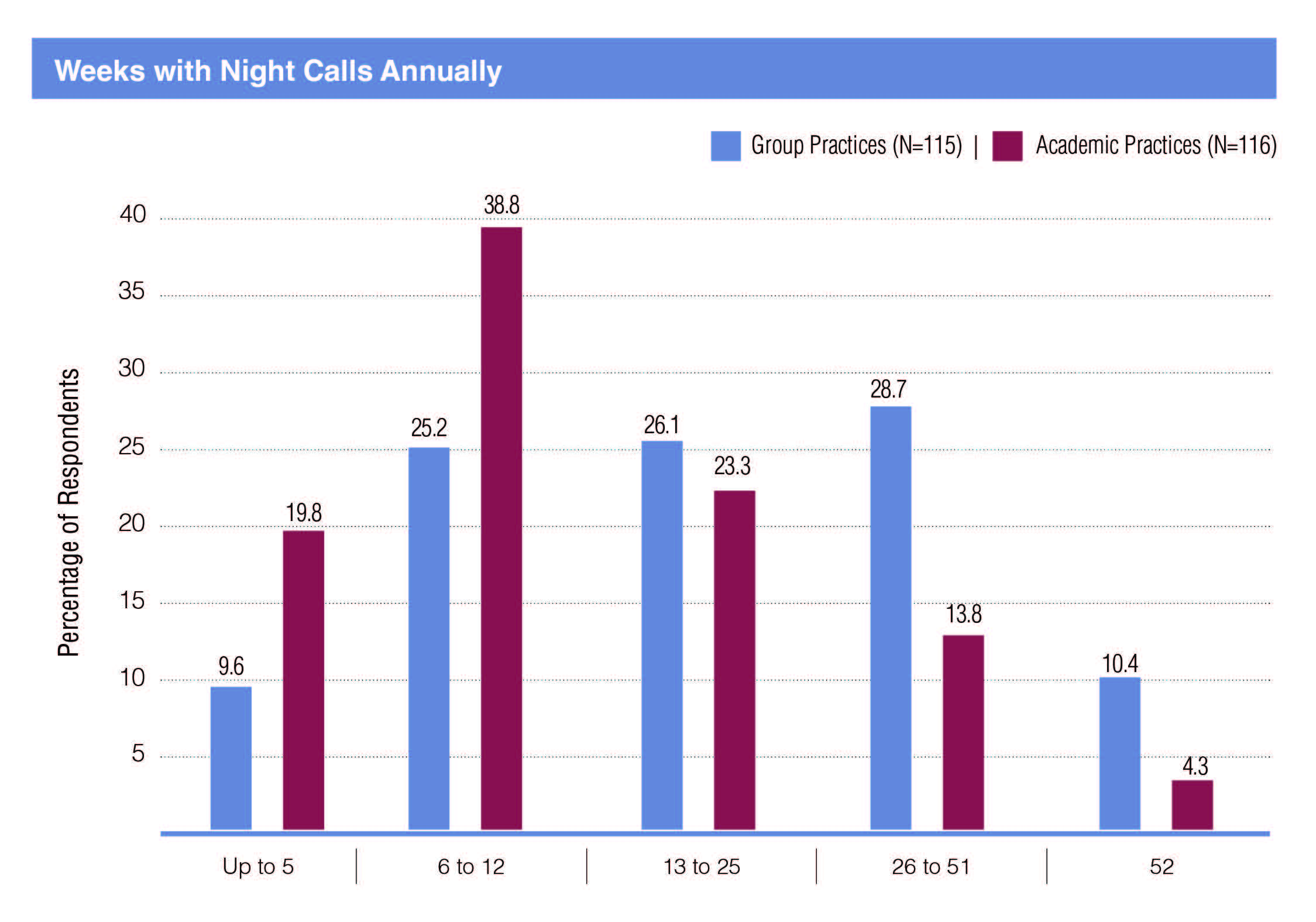
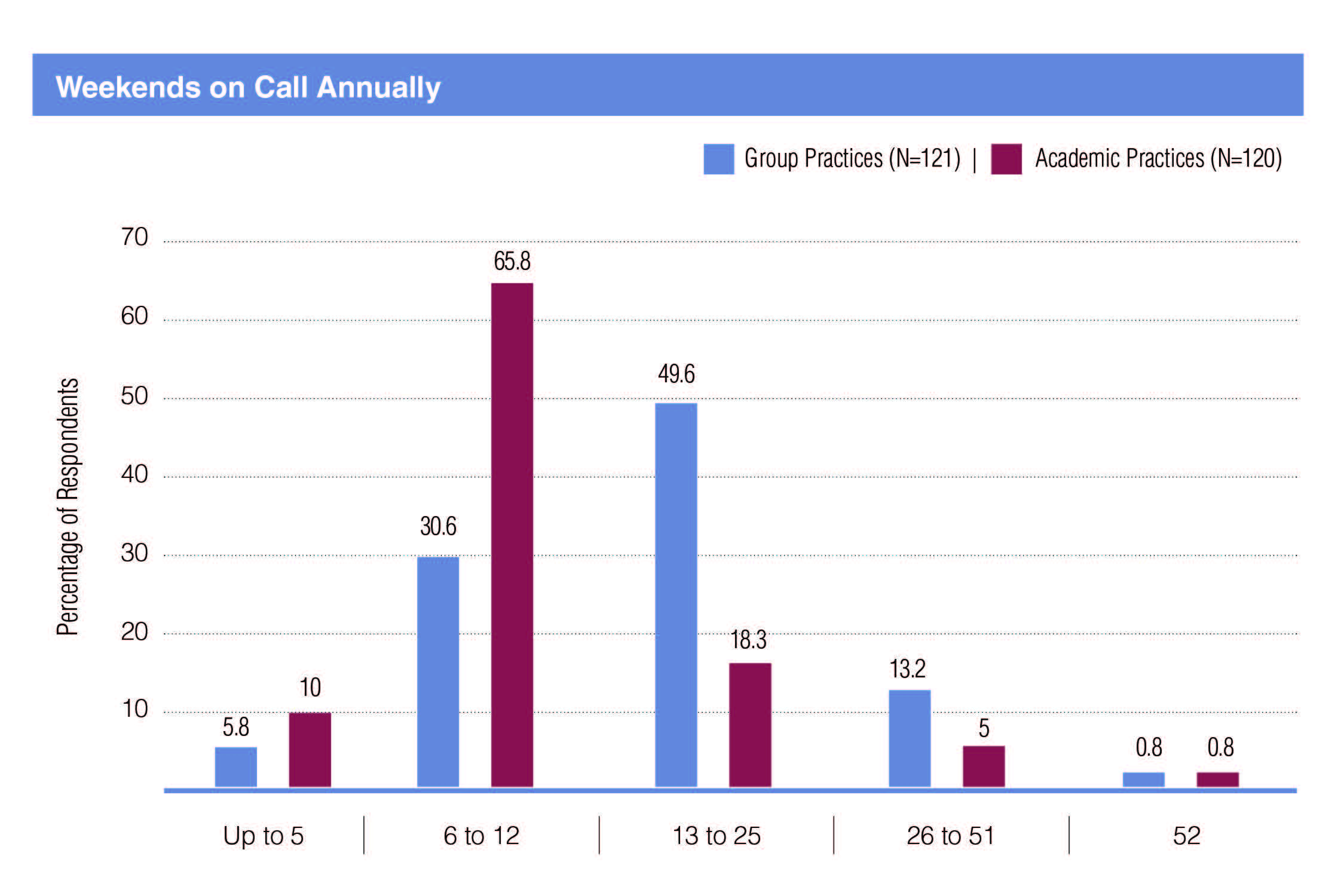
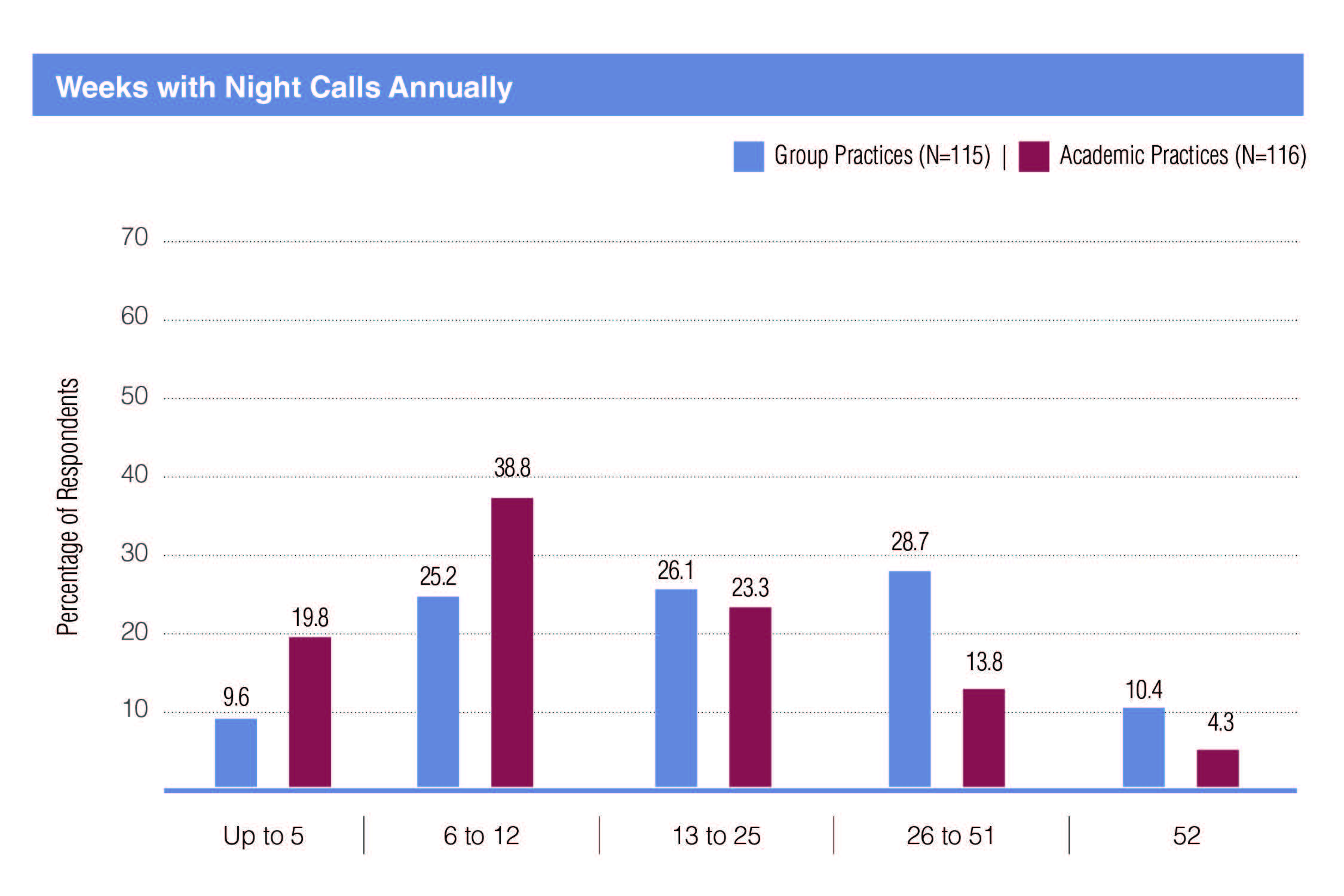
Group practice nephrologists have far more evening and weekend call responsibilities: 60.6% of group practice nephrologists had weekend call 13 times or more in a year while only 24.1% of academic nephrologists had 13 or more; and 39.1% of group practice nephrologists had night call 26 or more weeks compared to 18.1% of academic nephrologists.
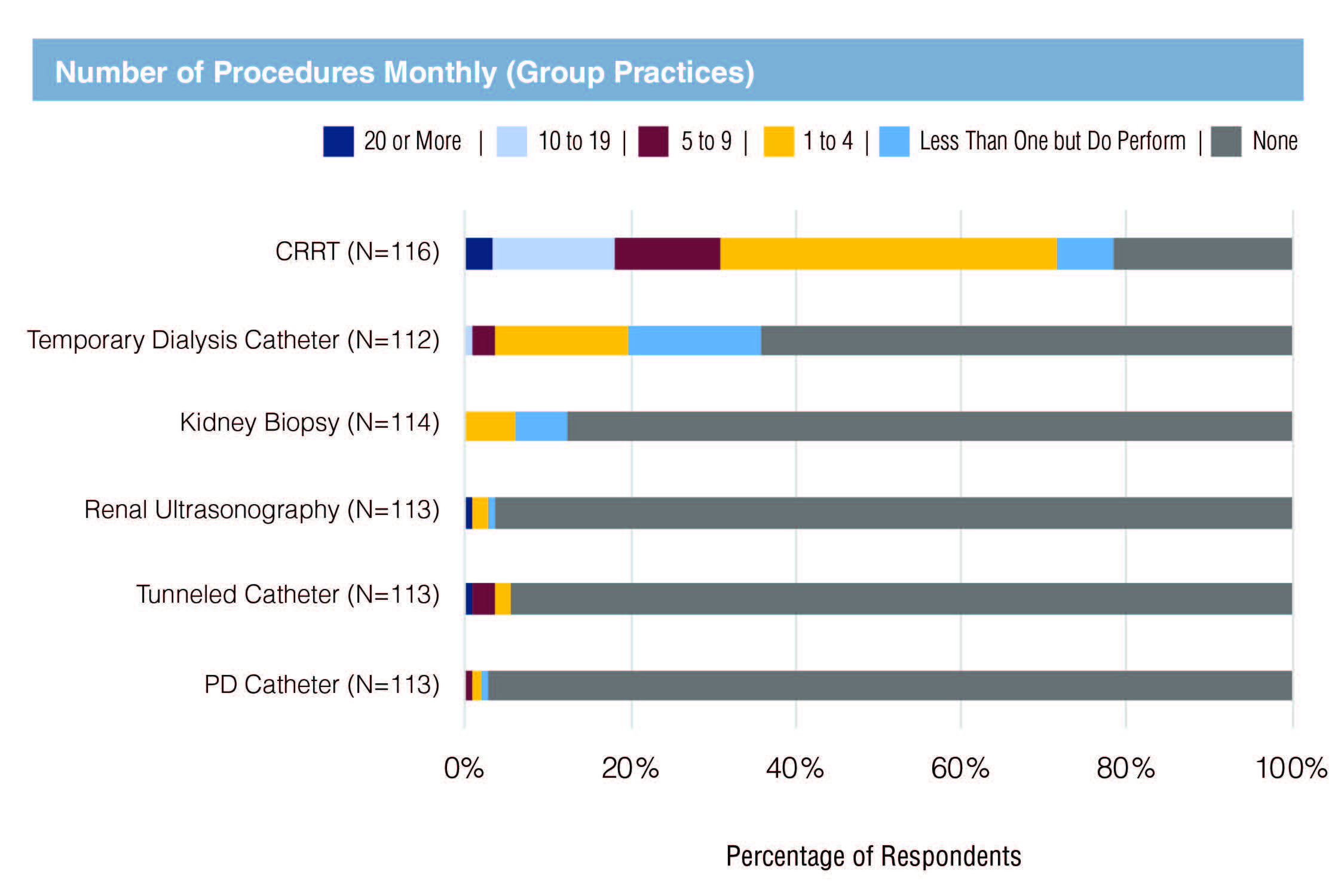
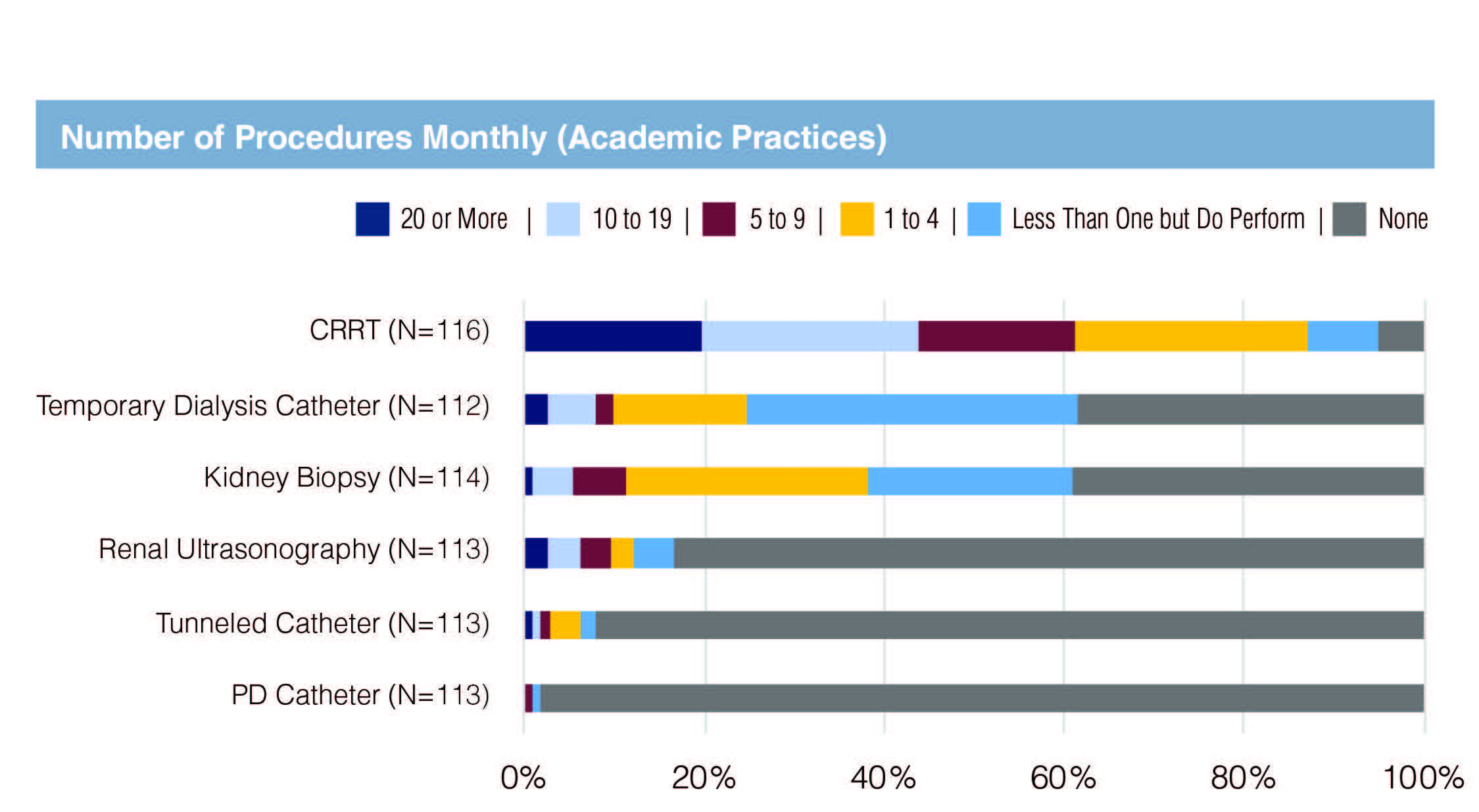
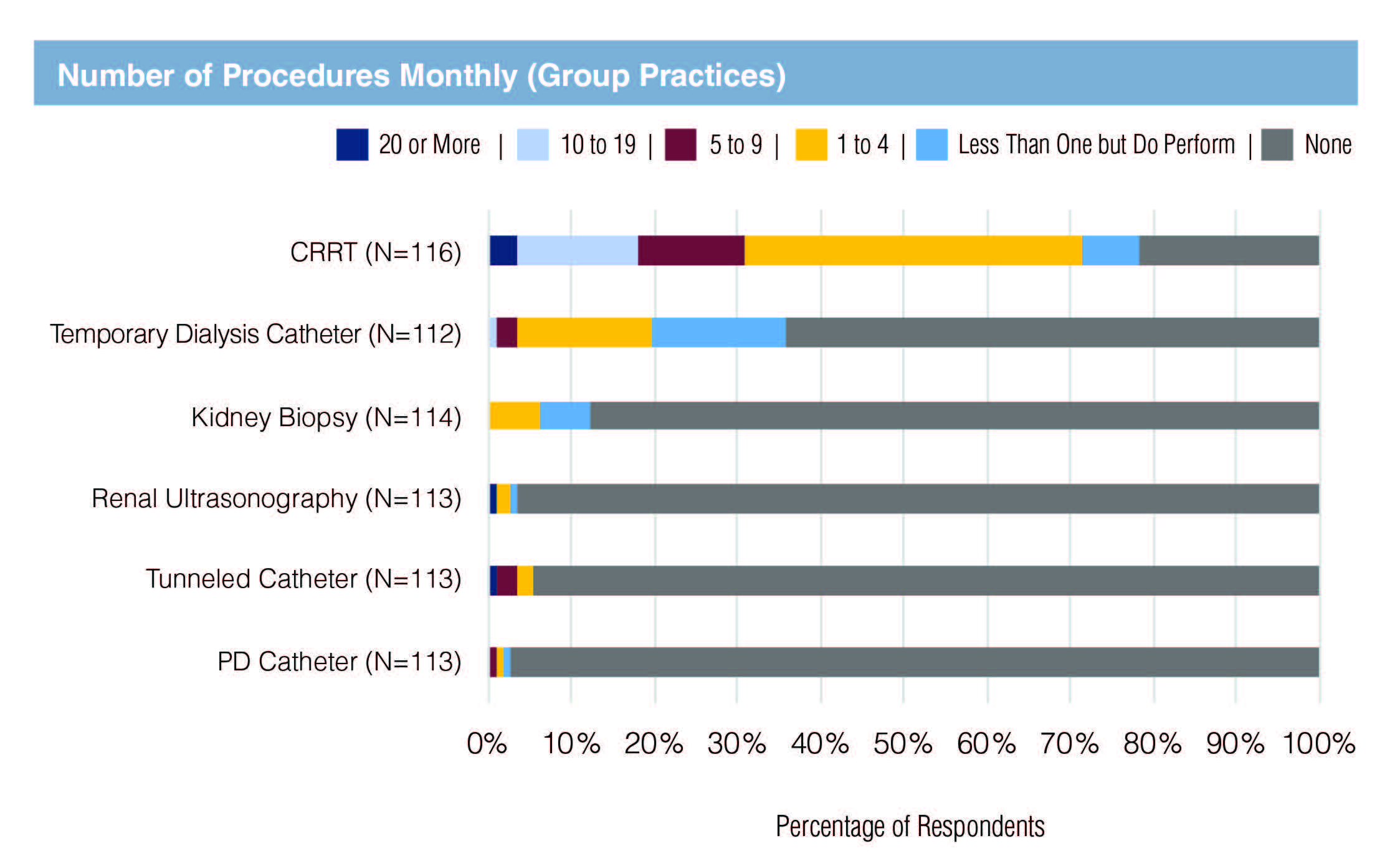
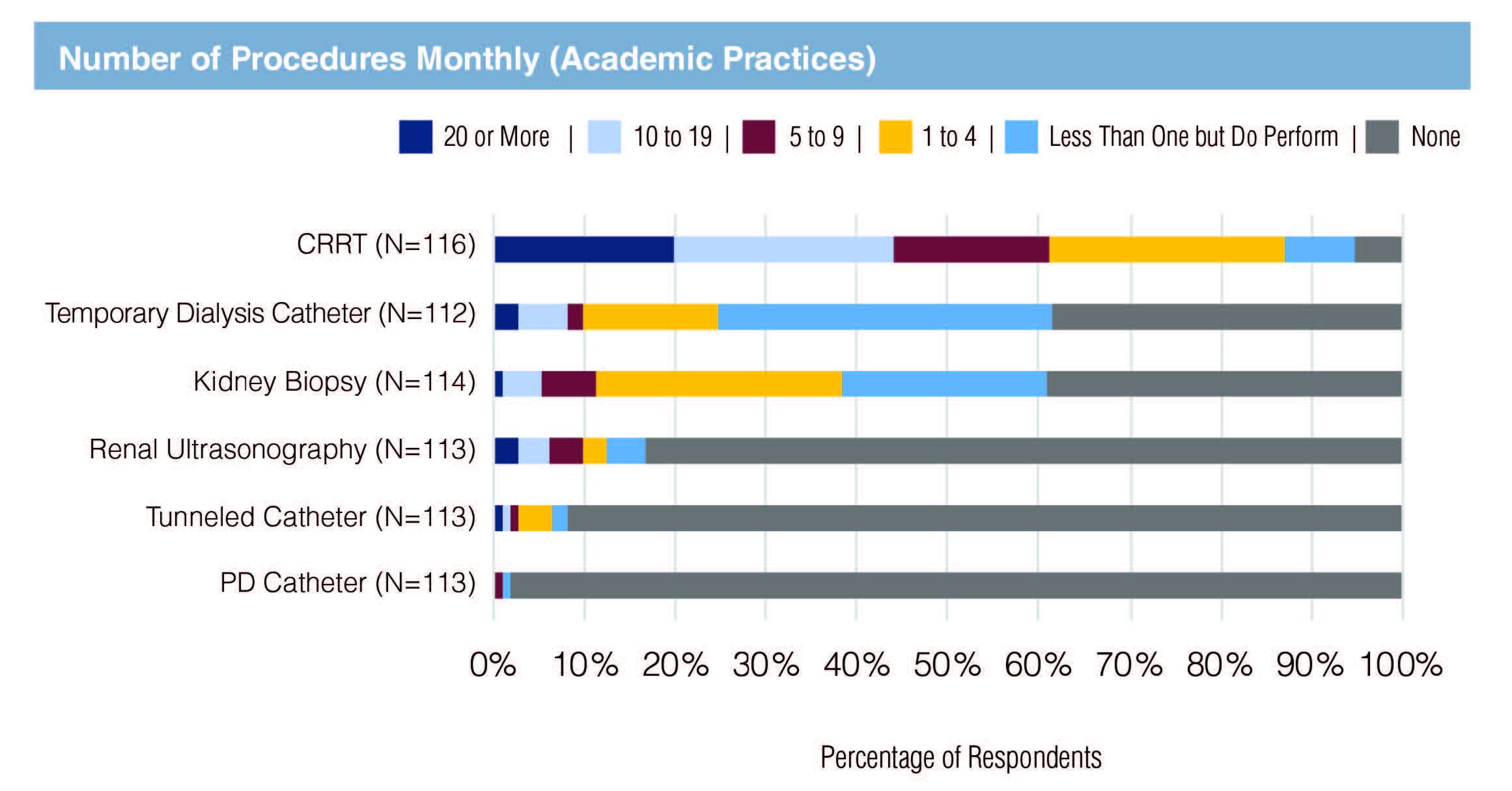
- While nephrologists generally provide a set of core services regardless of setting, there are some notable differences in regard to specific procedures. For example, 61.1% of academic nephrologists provided CRRT to 5 or more patients per month, yet, only 31% of group practice nephrologists provided that level of procedures. Only 12.3% of group physicians performed any kidney biopsies in a typical month compared to 60.9% of the academic nephrologists. Only 35.7% of group nephrologists performed any temporary dialysis catheter placement in a month compared to 61.4% of the academic nephrologists; and academic nephrologists were more than 4 times as likely to perform a renal ultrasound in a month as group nephrologists (16.7% vs. 3.5%).
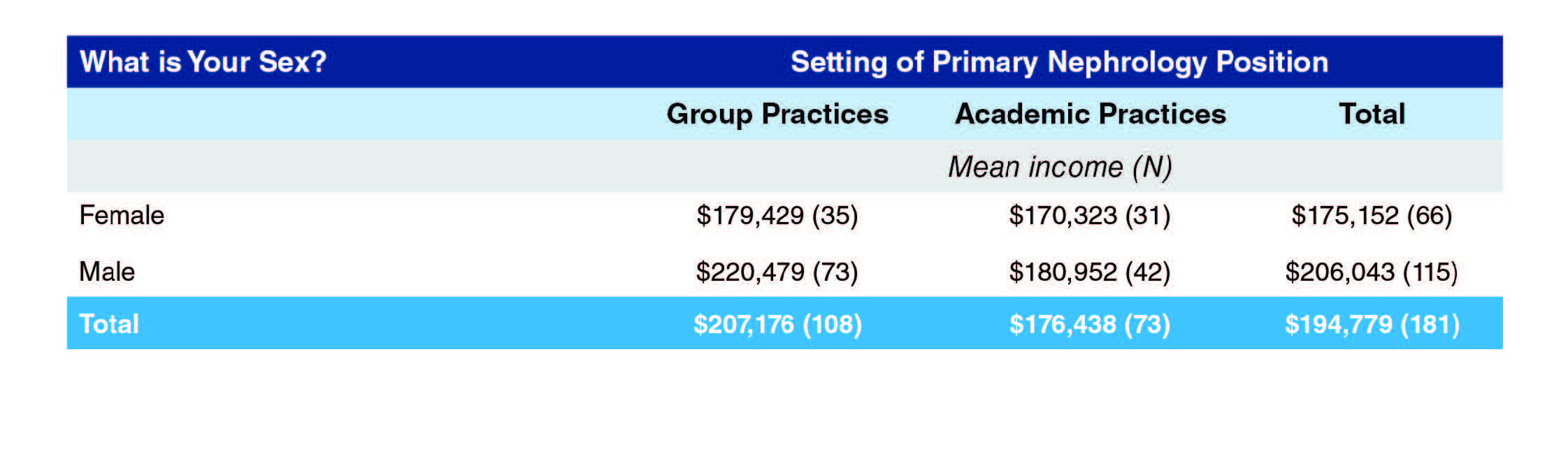
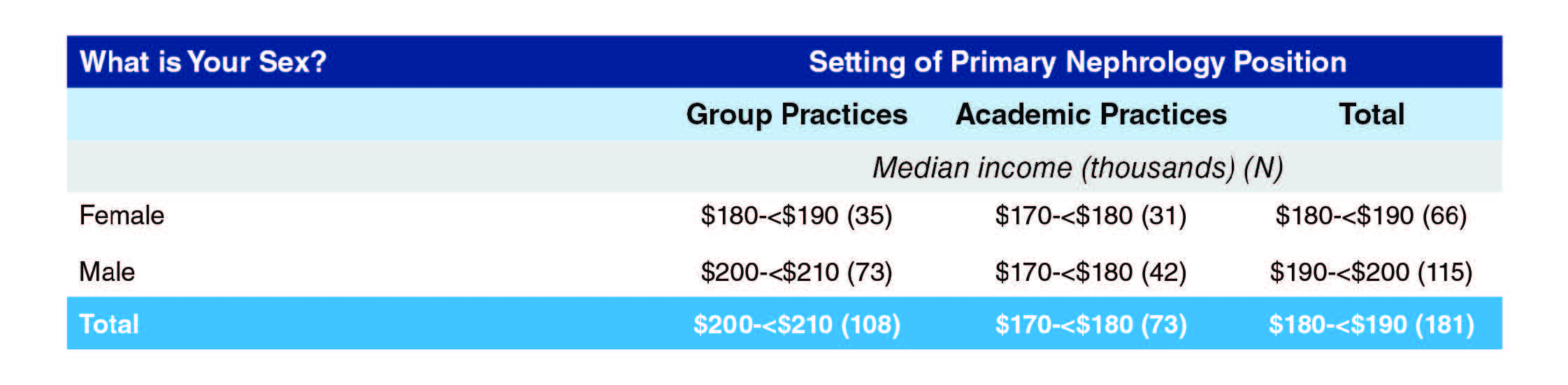
There was a significant difference in income by setting, with group practice nephrologists earning an annual mean income $30,000 higher than academic physicians (mean incomes $207,176 vs. $176,438). The difference was greatest for males, with male group practice nephrologists making nearly $40,000 more per year than male academic nephrologists ($220,479 vs. $180,952). The difference for females was a little more than $9,000.
When viewed by gender, males were making nearly $31,000 more than females (mean incomes $206,043 vs. $176,152). The difference was far greater in group practice ($41,050; $220,479 for males vs. $179,429 for females) than in academic positions ($10,629; $180,952 vs. $170,323).
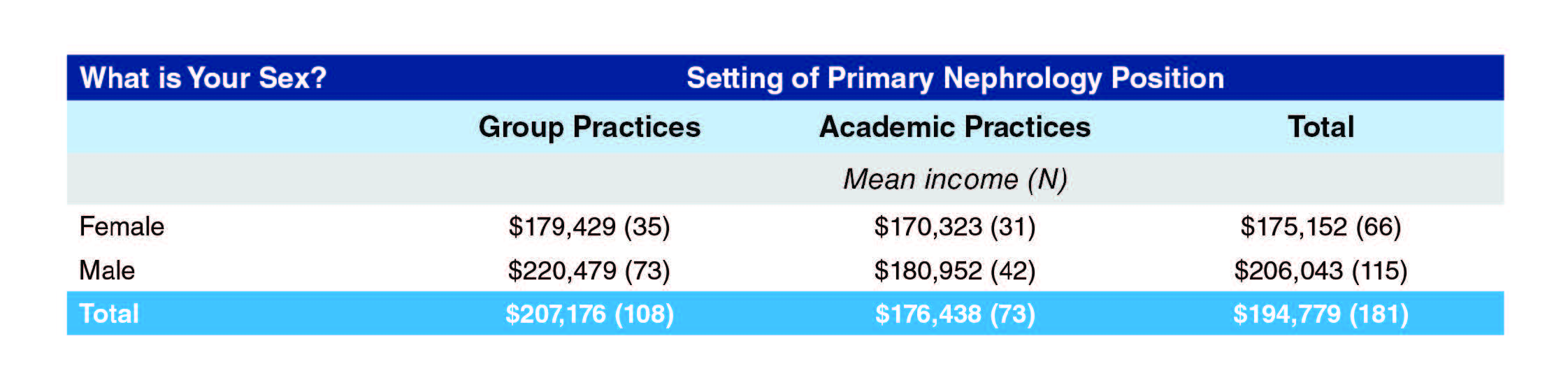
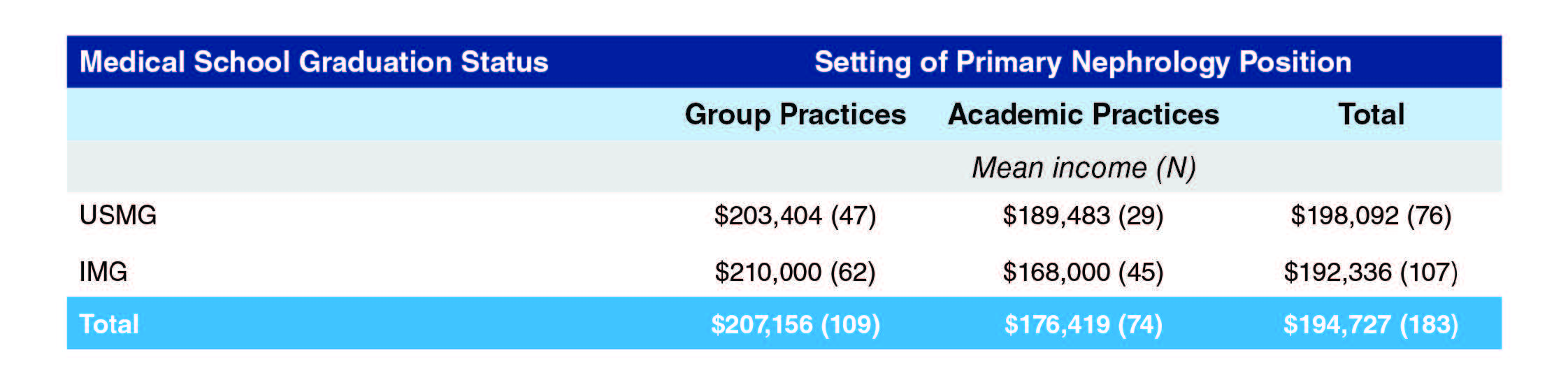
IMGs in group practices reported earning $6,500 more than USMGs in group practices ($210,000 vs $203,404). However, USMGs in academic settings make nearly $20,000 more than IMGs in that setting ($189,483 vs $168,000)
Despite the great variation between the incomes of nephrologists in group practice and academic institutions, their satisfaction with their income is similar. Overall, a quarter of nephrologists were dissatisfied with their income.
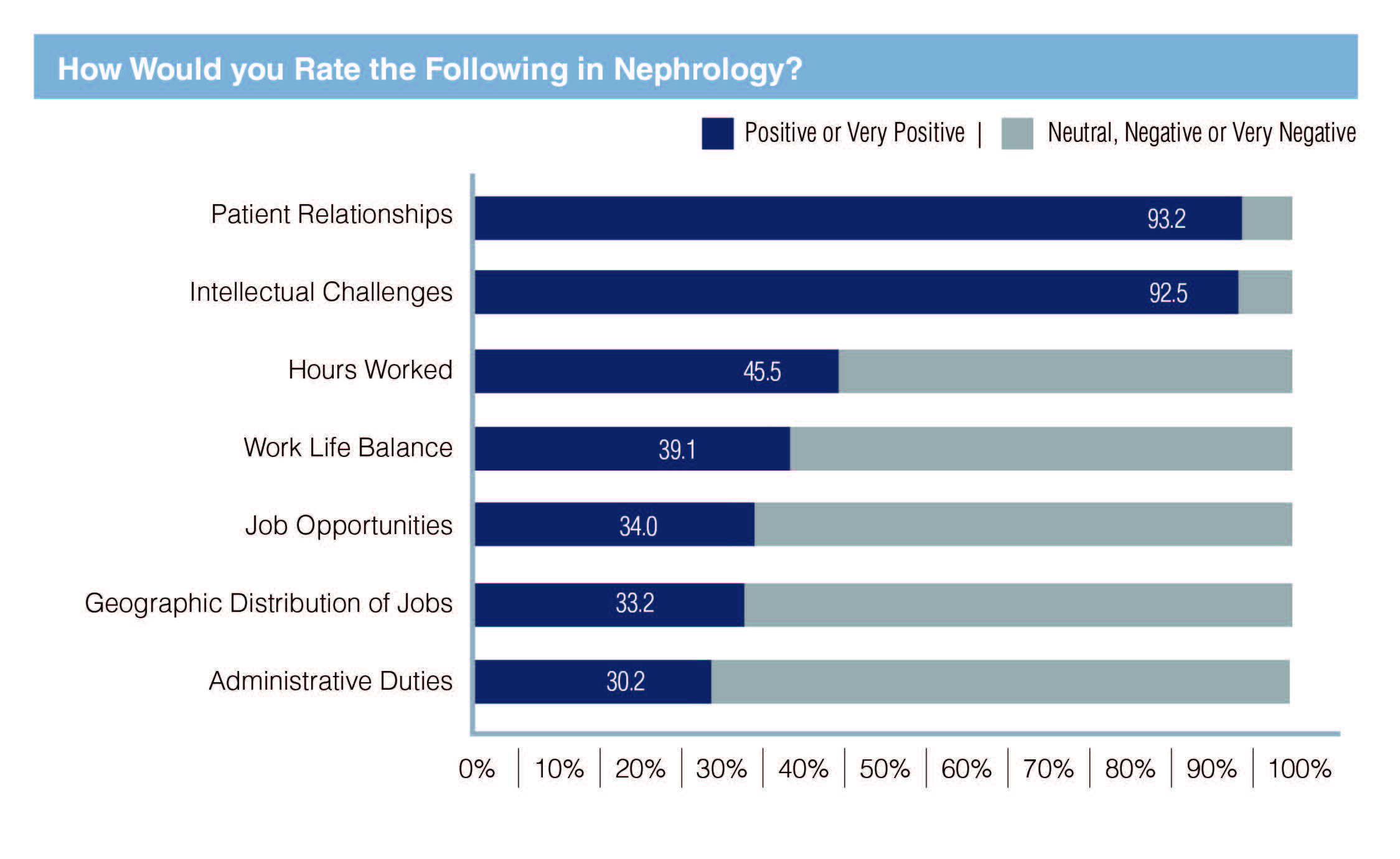
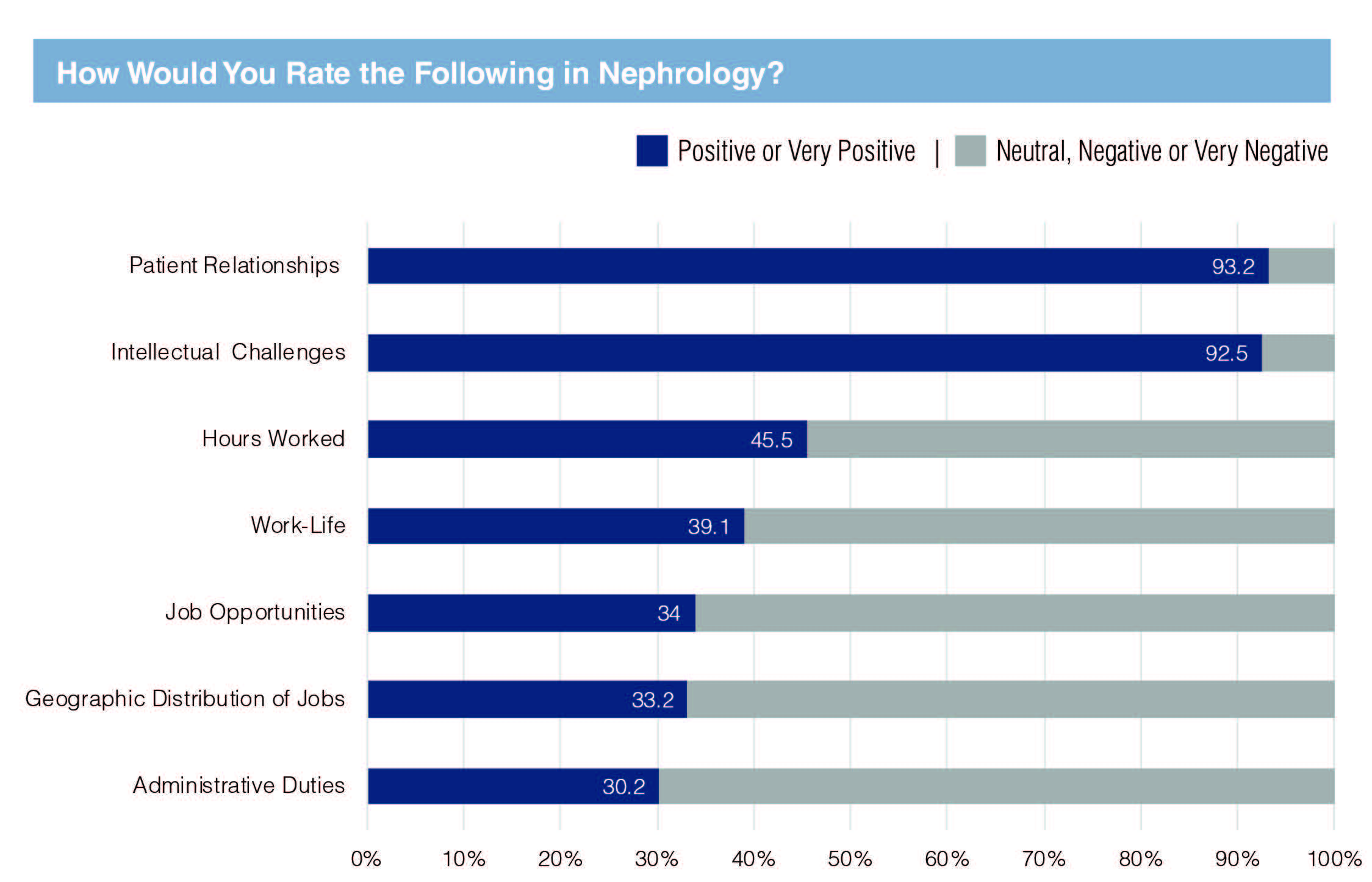
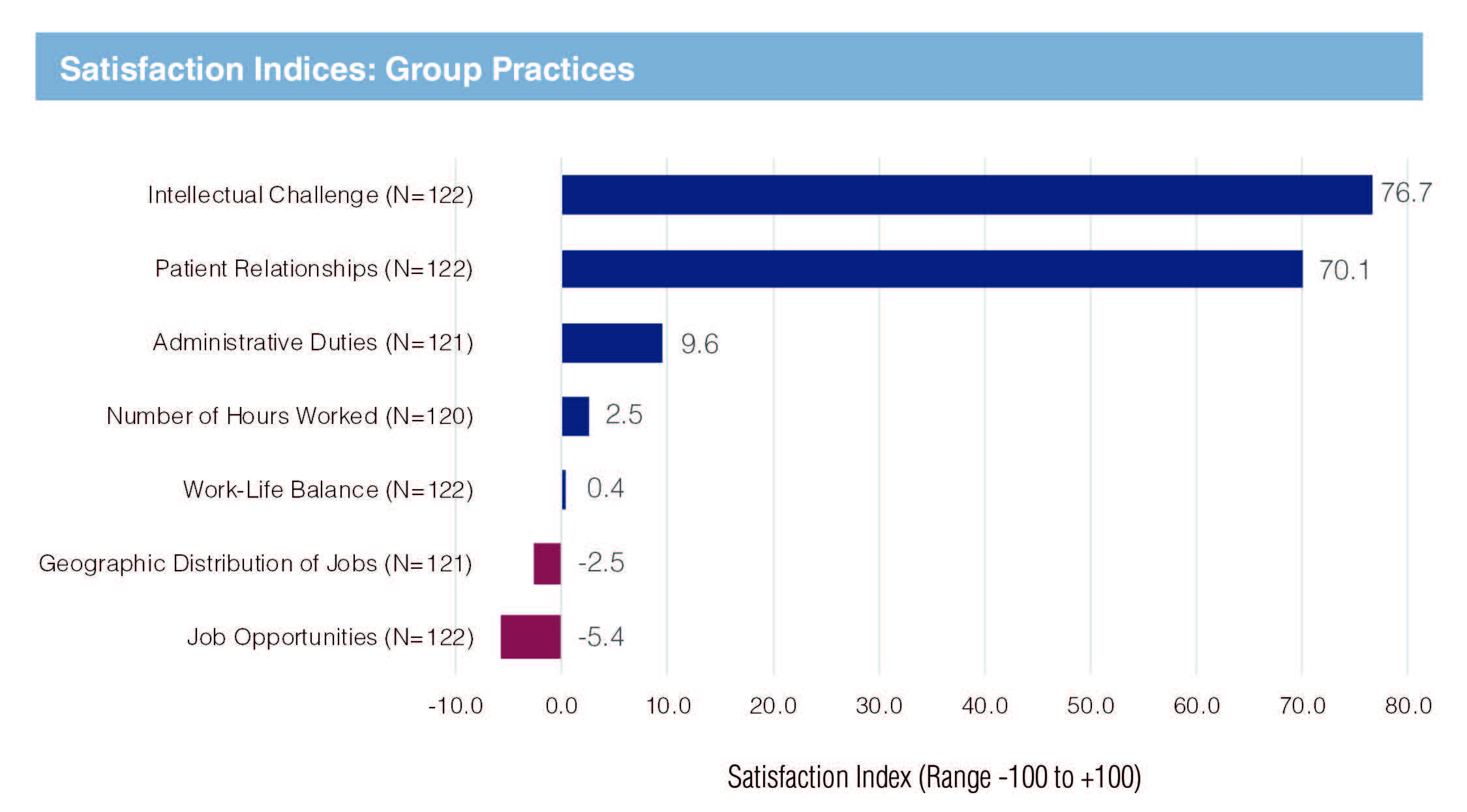
Both group practice and academic nephrologists were satisfied or very satisfied with the intellectual challenges (92.6% and 93.3% respectively) and with their relationships with patients (91% and 94.5% respectively). These were clearly some of the key reasons for selecting the specialty and undoubtedly contributed to the general satisfaction with their current position.
Overall, 11.6% were dissatisfied with the current position, with similar percentages for group and academic nephrologists.
On the other hand, work hours and ability to balance work-life needs are challenges in nephrology especially in group practice: 35% of group practice nephrologists had a negative opinion of hours worked compared to 23.5% of academic nephrologists; and 33.6% of group practice nephrologists were dissatisfied with their work-life balance compared to 26.1% of the academic nephrologists.
Many group practice nephrologists were also dissatisfied with job opportunities in nephrology (38.5%); this was also an issue for academic nephrologists but to a lesser extent (23.7% dissatisfied).
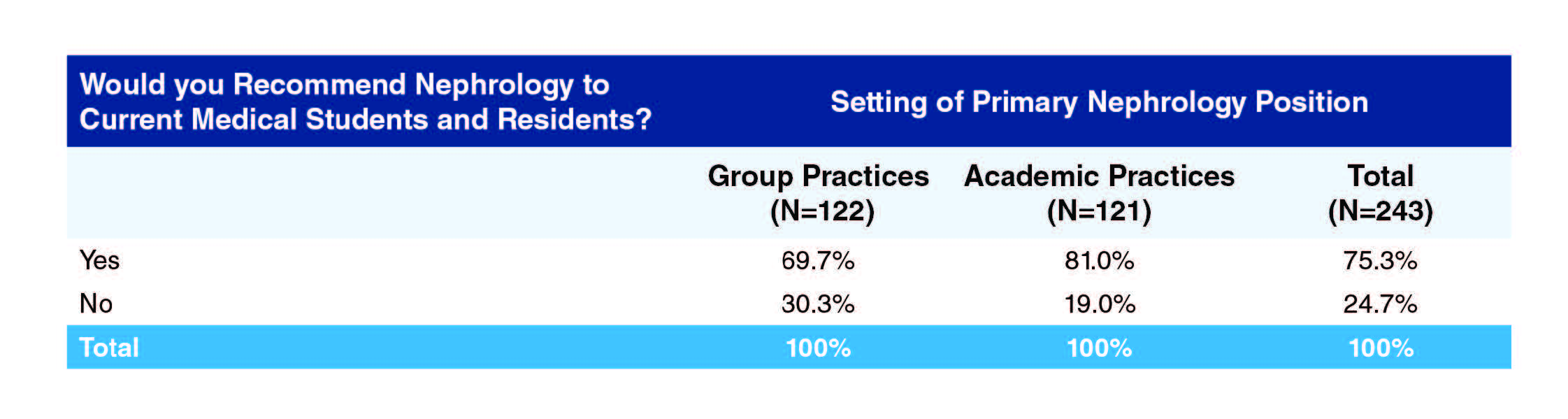
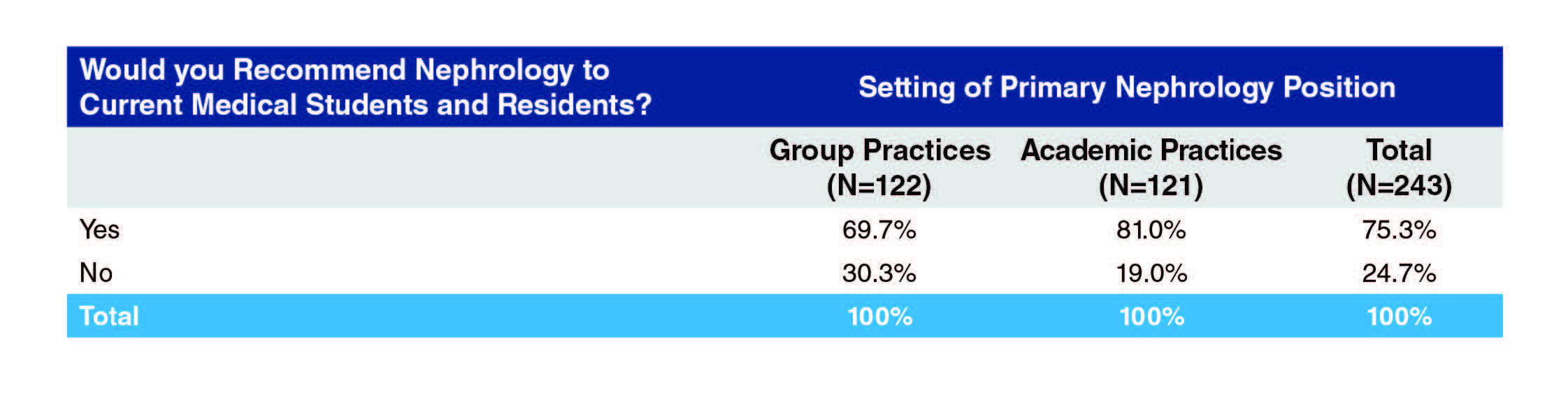
The difference in satisfaction between the group and academic nephrologists comes out in their willingness to recommend the specialty to medical students and residents: 81% of academic physicians would recommend the specialty compared to 69.7% of group practice nephrologists.
Methods
The target group for the survey was nephrology fellows who graduated during the period 2012–2015 and had therefore been in practice for at least one year. ASN provided GW-HWI with 2934 email addresses of nephrologists believed to have completed training in that period. GW-HWI utilized REDCap survey software for emailing a unique survey web link to each potential participant. The survey launched in late May 2017 and closed after five weeks with 320 valid responses for a response rate of 10.9%.
During data cleaning it was found that a number of respondents had completed their fellowship outside the target year range, including 2016 graduates. Given the relatively low response rate and noting that most 2016 graduates would likely have a full year’s practice experience behind them and therefore could provide useful data about post-training practice, it was decided to extend the year range for completing core nephrology training to 2009–2016 but to exclude those outside this range. Ten respondents who did not provide their year of completing training were also included, in the expectation that they were far more likely than not to fall within the year range of interest given the method by which individuals were selected for the survey.
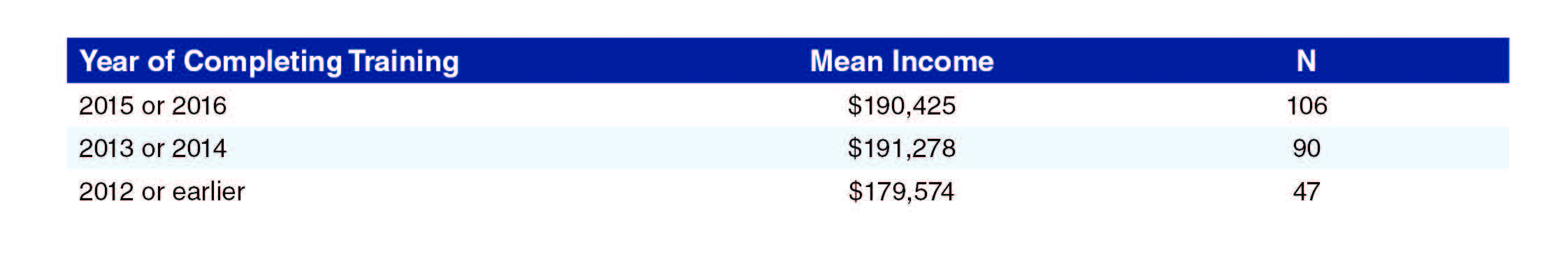
A decision was made to exclude pediatric nephrologists; taken together with data cleaning this left a total of 270 respondents for the analysis. . lists the responses by year of completing core training.
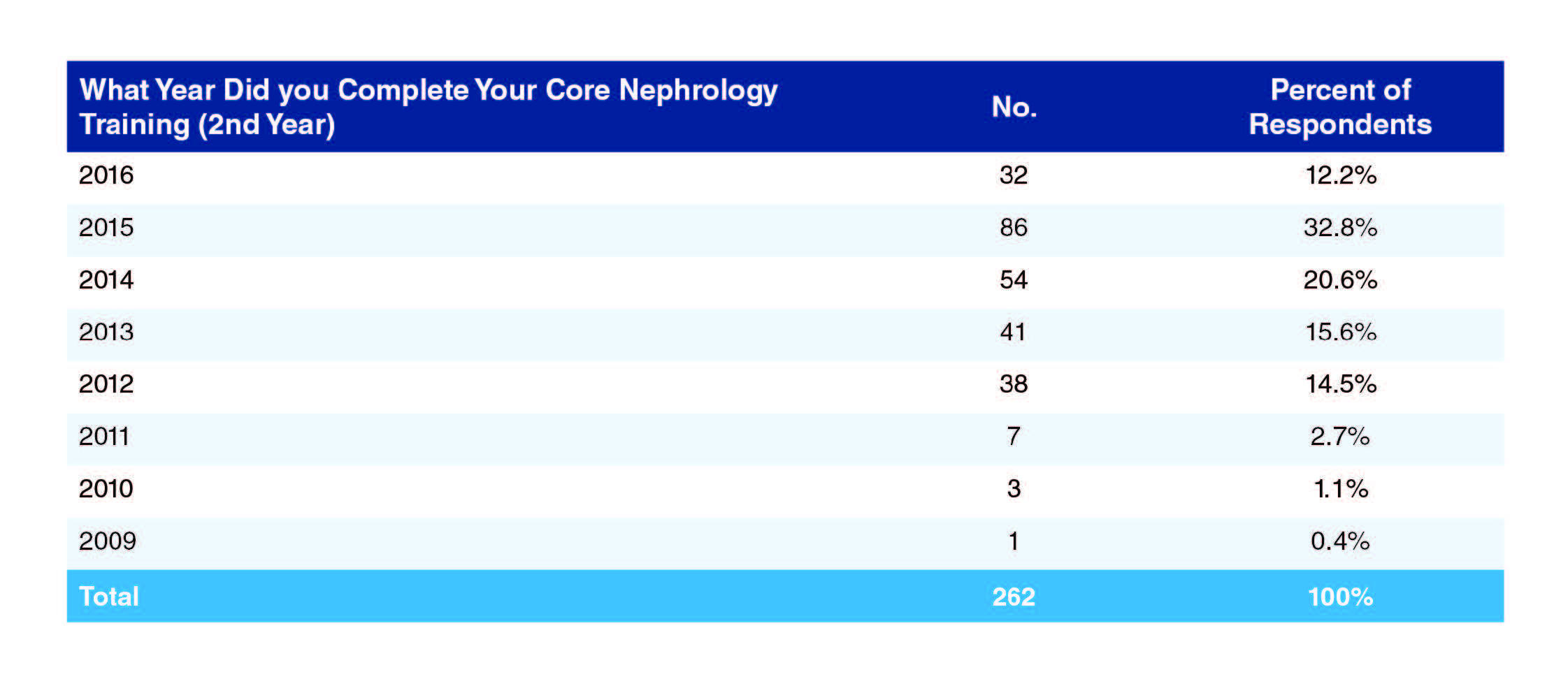
As the exhibit shows, respondents’ years of completing nephrology training ranged from 2009 to 2016, which is consistent with the target group being 2012–2015 new practitioners, some of whom were continuing with extra training following core nephrology training before beginning practice.
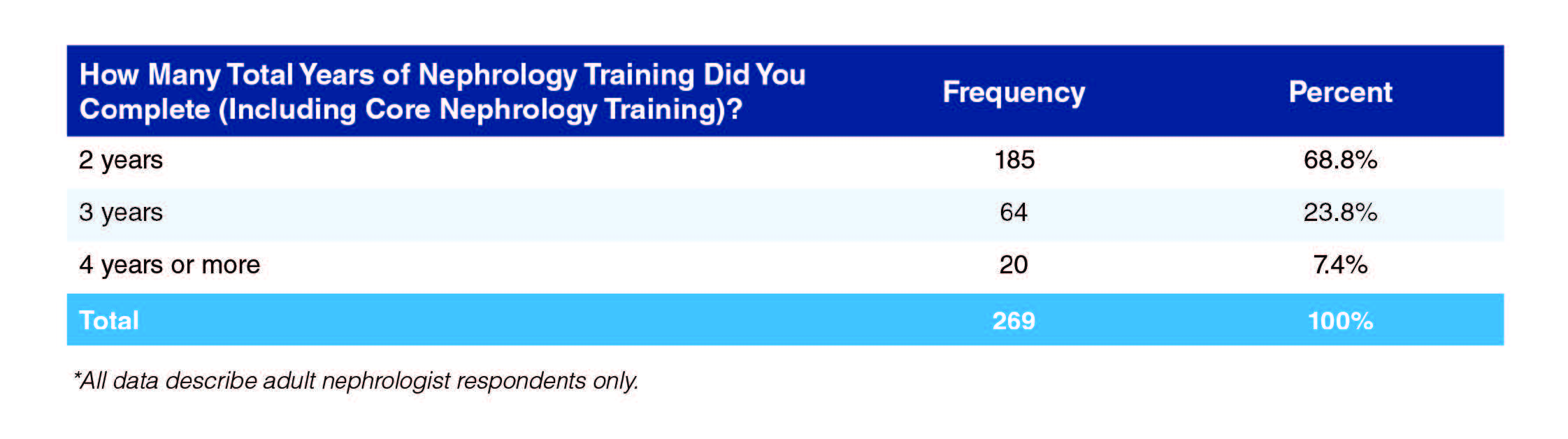
More than two-thirds of respondents (68.8%, Exhibit 2) completed their nephrology training in 2 years though a substantial minority spent 3 or more years in training.
Representativeness
Comparison with ACGME data from 2013–2014 and 2015–2016 suggests that respondents to the Early Practice Survey had a higher proportion of females (by around 5%) and a lower proportion of IMGs (by around 10–12%) than the likely population of nephrologists who completed training in recent years. Proportions of Black/African Americans and Hispanics/Latinos were, very roughly, in line with the expected population.
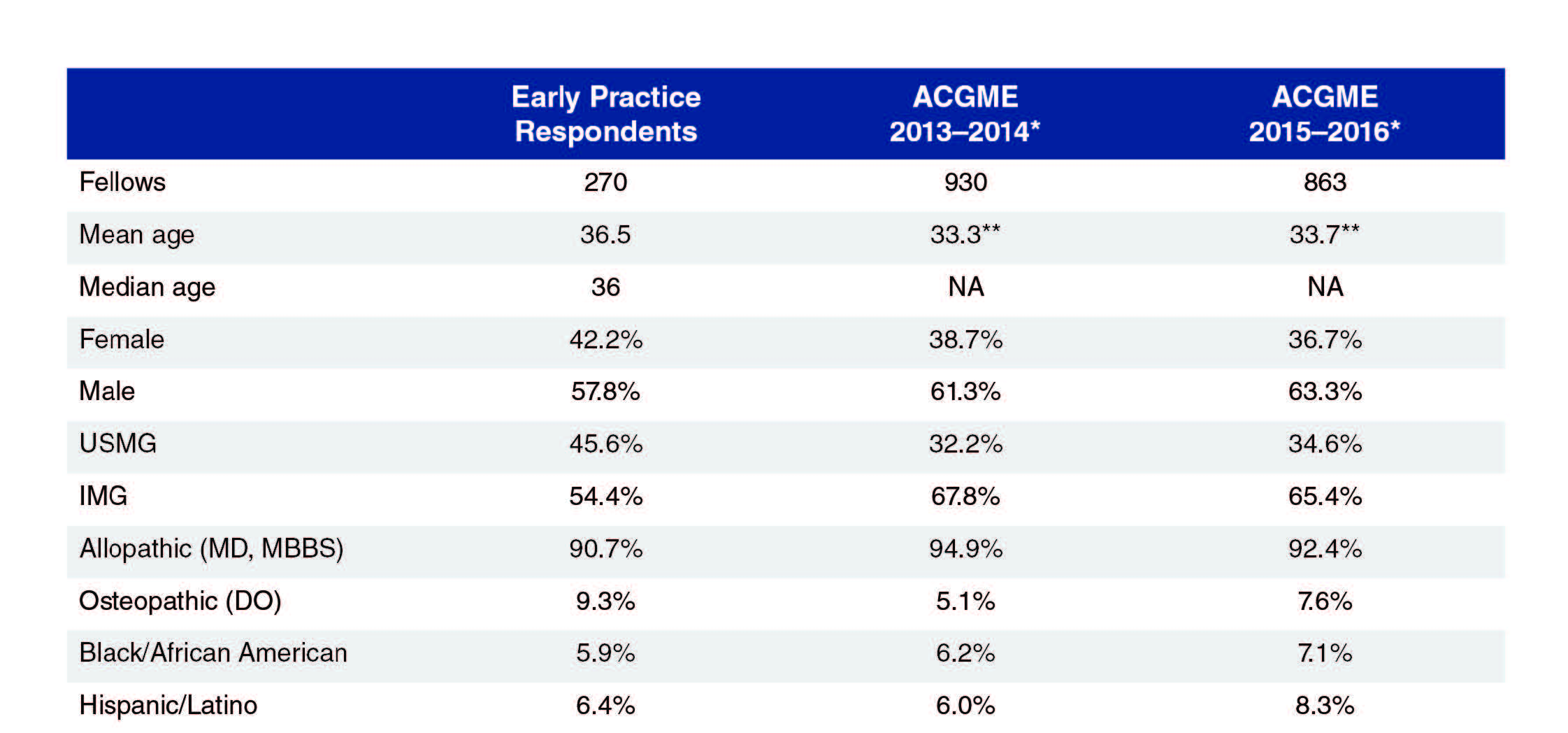
*Includes all active residents, except that overall fellow number is for 1st and 2nd year fellows only
**Mean age of first year nephrology fellows.
Source: ACGME Data Resource Books, 2014 and 2016
Educational and Demographic Background
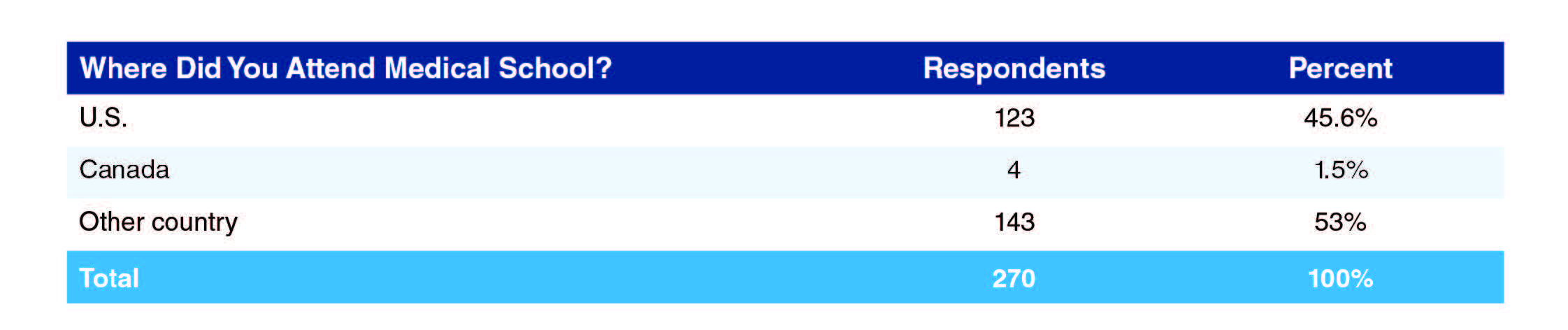
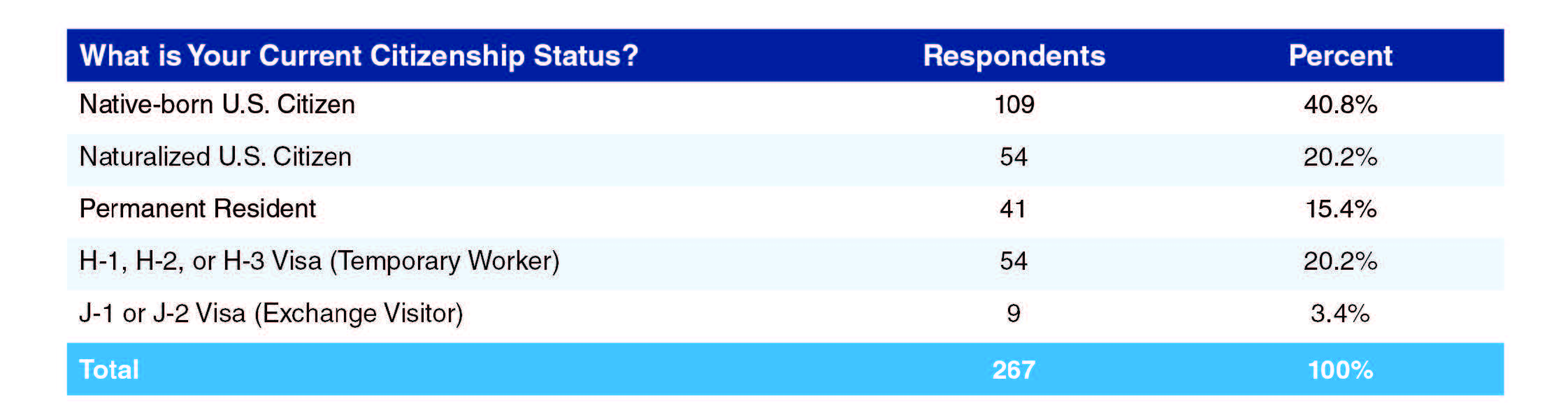
More than half of respondents were U.S. citizens, either native born (40.8%) or naturalized (20.2%). Around one-quarter were on temporary visas, either temporary worker (H, 20.2%) or exchange visitor (J, 3.4%) visas. It is unclear why any practicing nephrologists would be on exchange visitor visas, though it is possible these were former J visa holders working in HPSAs under one of the various J visa waiver schemes. (Technically, waiver holders transfer to H-1B visas, but it is possible some are unaware of this change in visa status. GW-HWI has agreed with ASN to conduct interviews during 2018 to explore this and similar questions about visa status awareness.)
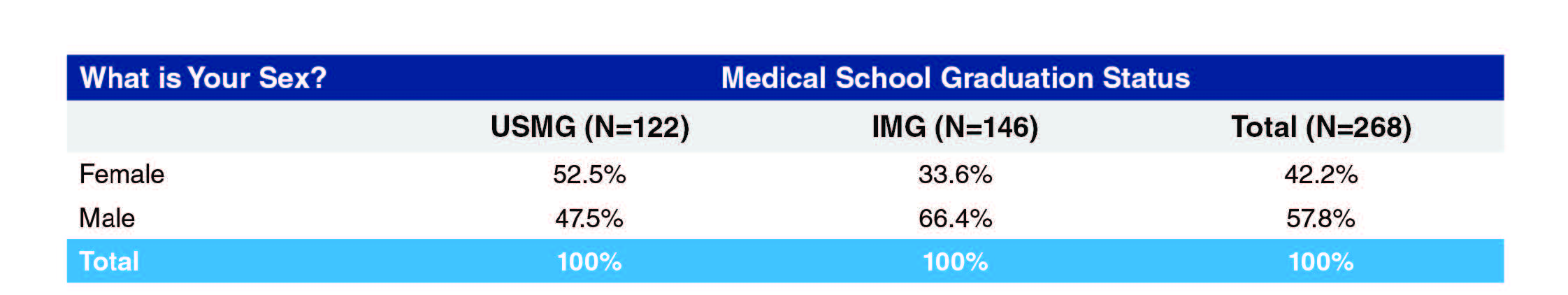
IMG respondents were more likely than USMGs to be male (66.4% vs. 47.5% male respectively, Exhibit 6).
Academic Practice vs. Private Practice
An analysis of the survey responses indicated that there were significant differences on numerous variables between nephrologists who had gone into academic practice compared to those who went into private practice. For that reason, this report includes numerous exhibits comparing nephrologists who are in group practice to those that are in academic practices.
As indicated in Exhibit 7, 47.1% of the respondents went into group practice and 47.1% into academic practice. Also, as indicated in the exhibit, females were more likely to go into academic practice than group practice (53% to 39%), while males were more likely to go into group practice (53% to 42%).
As indicated in Exhibit 8, USMGs were more likely to enter academic practices than group practices (51% to 43.5%), while IMGs were more likely to enter group practices (50% to 44%).
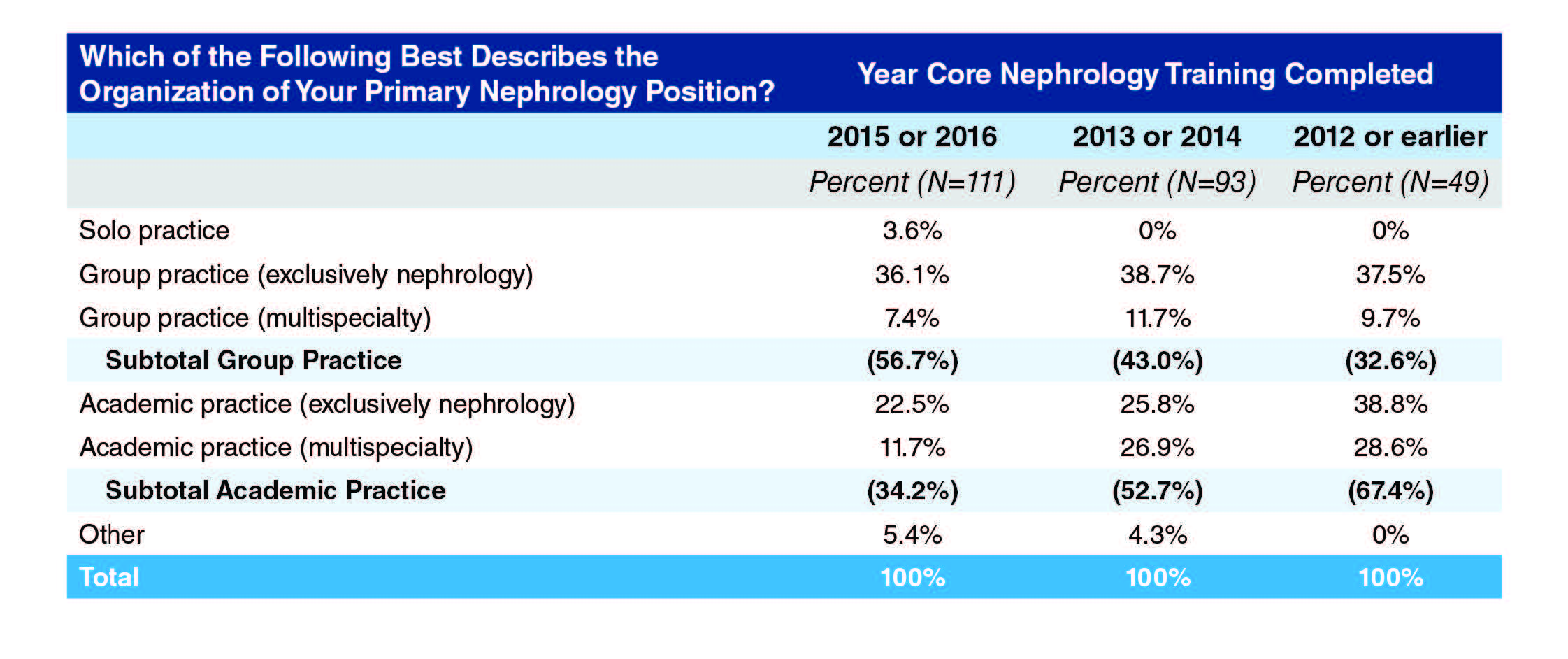
It appears that as a nephrologist advances through their early career they move away from group practice and towards academic practice (Exhibit 9), with the percentage in group practice at 56.7% among those who completed core training in the past two years but only 32.6% among those who completed training in 2012 or earlier; conversely, the percentage in academic practices is almost double among those who completed training in 2012 or earlier compared to those completing training in 2015 or 2016 (67.4% vs. 34.2%). It is also possible that the 2011–2012 cohort entered practice at a time when there happened to be opportunities in academic practice.
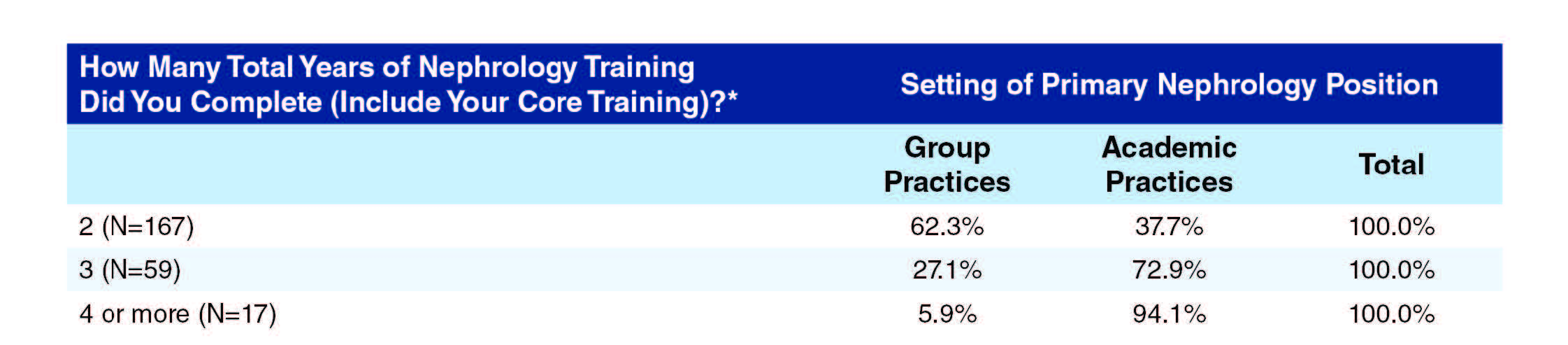
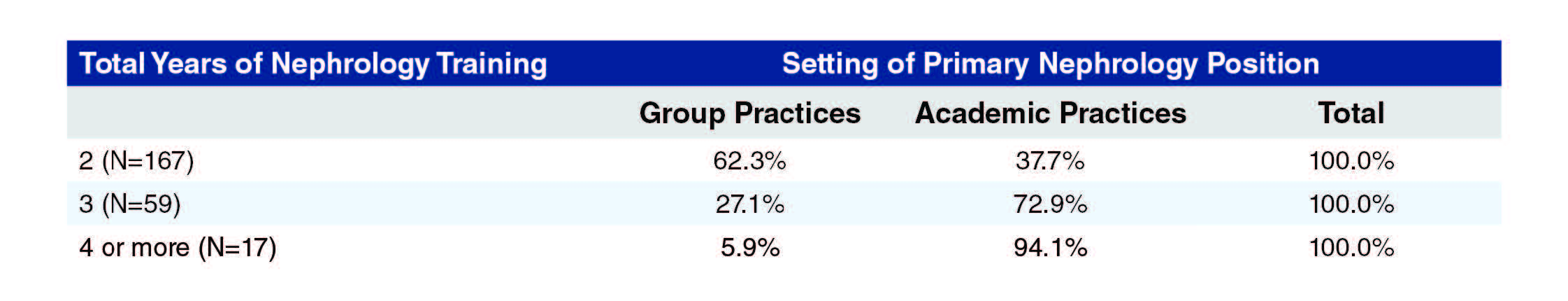
As might be expected, those working in academic practices typically spent more years in nephrology training than those working in group practices (Exhibit 10). Almost twice as many of those with only two years of training were working in group practices as in academic practices (62.3% vs. 37.7%), with the proportions being more than reversed for those with three years of training; only one of the 17 with four or more years of training was working in a group practice.
Practice and Focus Activities
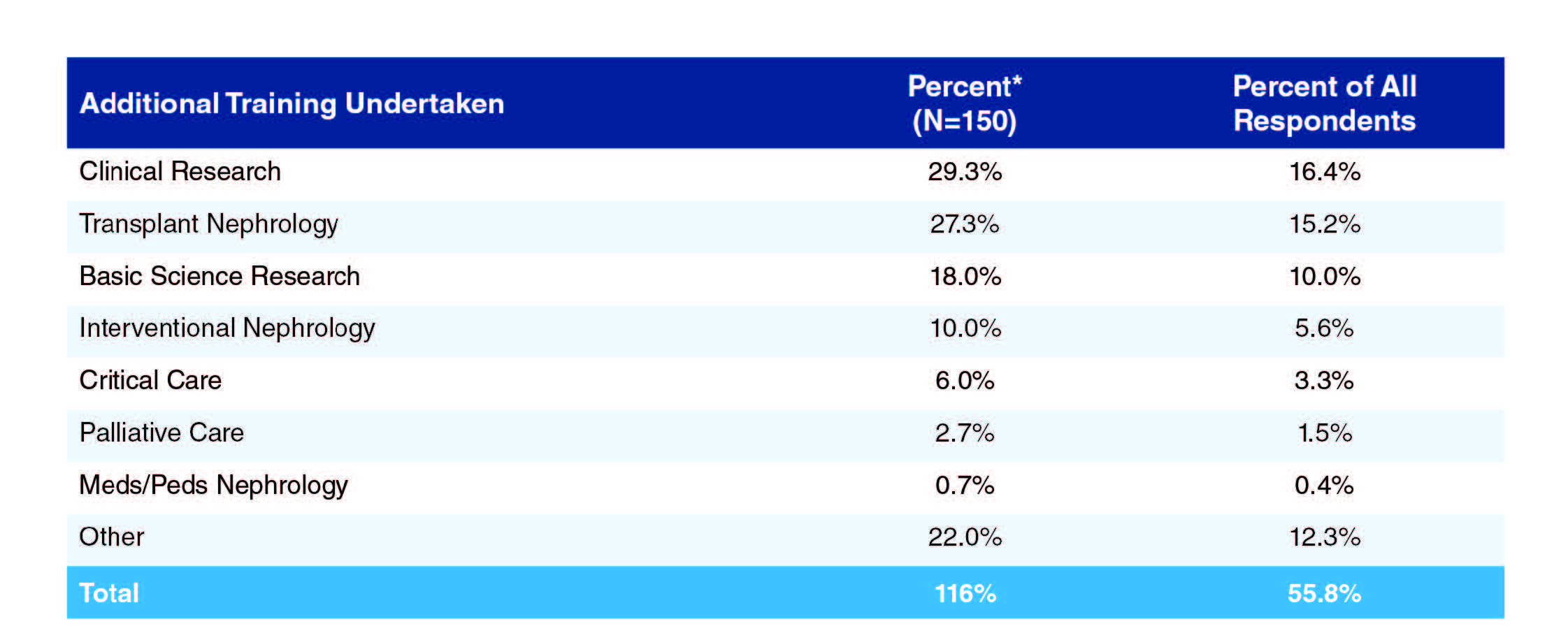
More than half (55.8%) of respondents indicated they had taken additional training following completion of core nephrology training (Exhibit 11). The most common additional trainings undertaken were clinical research (29.3% of respondents who answered any part of this question), transplant nephrology (27.3%), basic science research (18.0%), and interventional nephrology (10.0%). Among the 18 others, 2 (1.4%) cited clinical ethics training, two cited glomerular disease and two mentioned medical education.
*These percentages are of respondents who answered any part of this question and add up to more than 100% because respondents could indicate more than one answer (though few did).
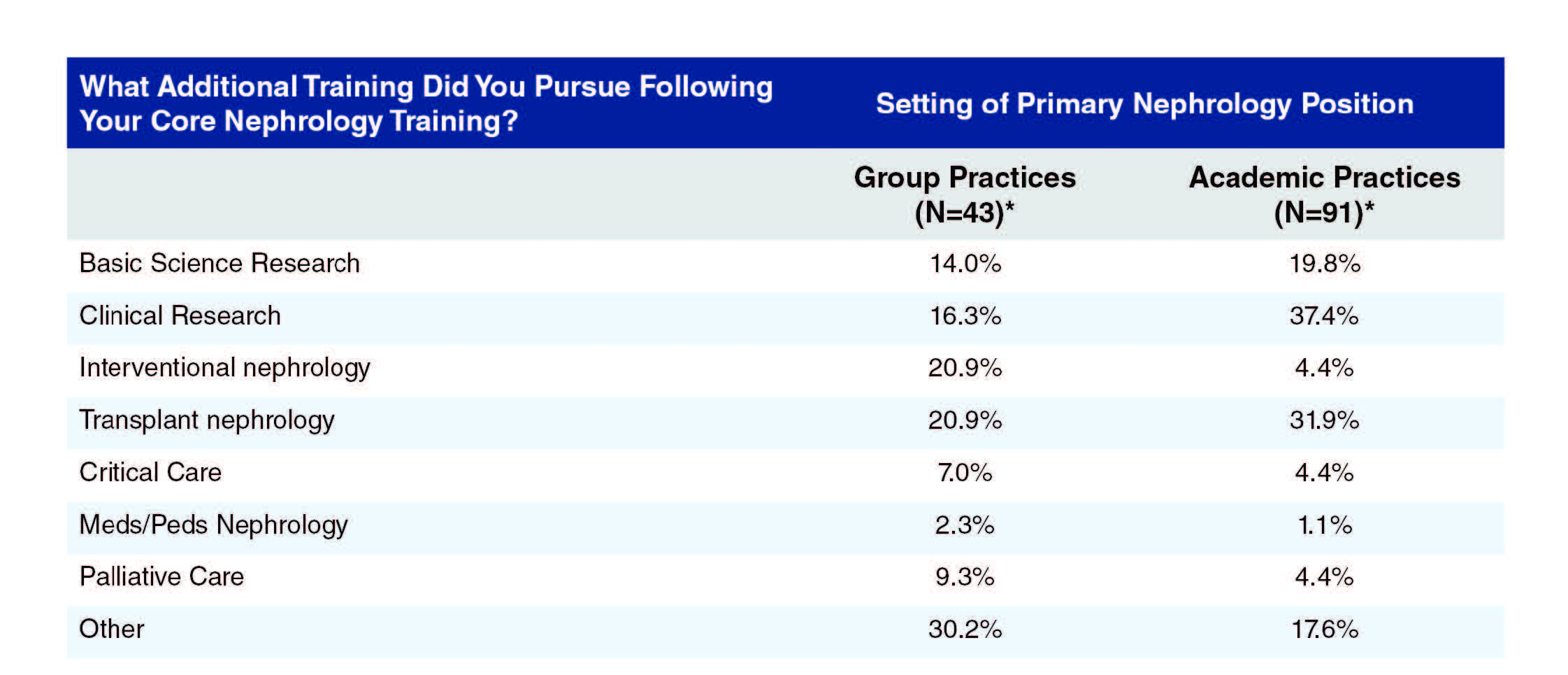
There were some substantial differences in training patterns depending on practice setting in either group practice or academic practice, as seen in Exhibit 12. For example, more than twice as many of the respondents from academic practices had had training in clinical research compared to those in group practices (37.4% vs. 16.3%), and one and a half times as many had had training in transplant nephrology (31.9% vs. 20.9%); conversely, far more of the respondents from group practices had undergone training in interventional nephrology (20.9% vs. 4.4% of those from academic practice).
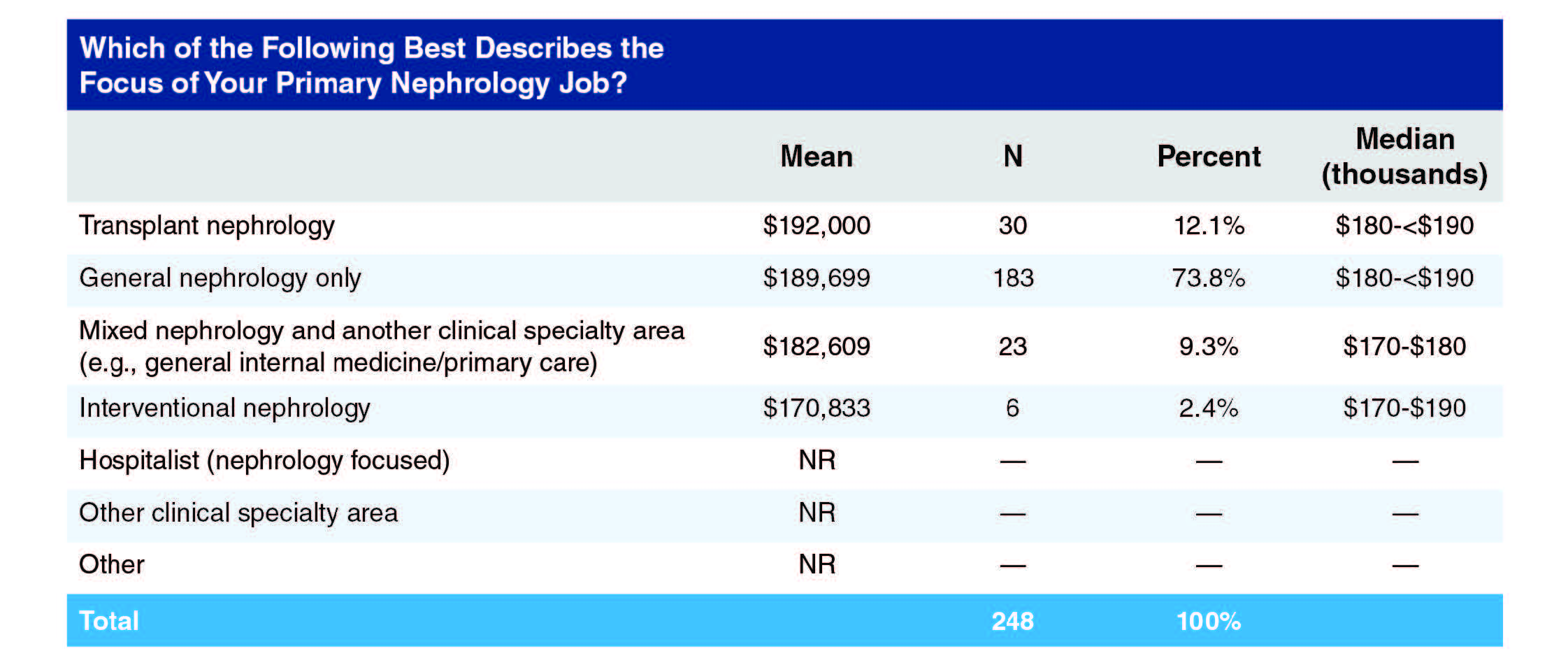
Almost three-quarters of respondents (72.2%) said their primary work focus was general nephrology (Exhibit 13). The only other notable responses were transplant nephrology (11.9%) and mixed nephrology plus another clinical specialty area (8.8%). USMGs were more likely than IMGs to focus on general nephrology (79.7% vs. 66.0%) but less likely than IMGs to work in transplant nephrology (8.1% vs. 15.0%). Only 9 (3.3%) were not primarily focused on nephrology.
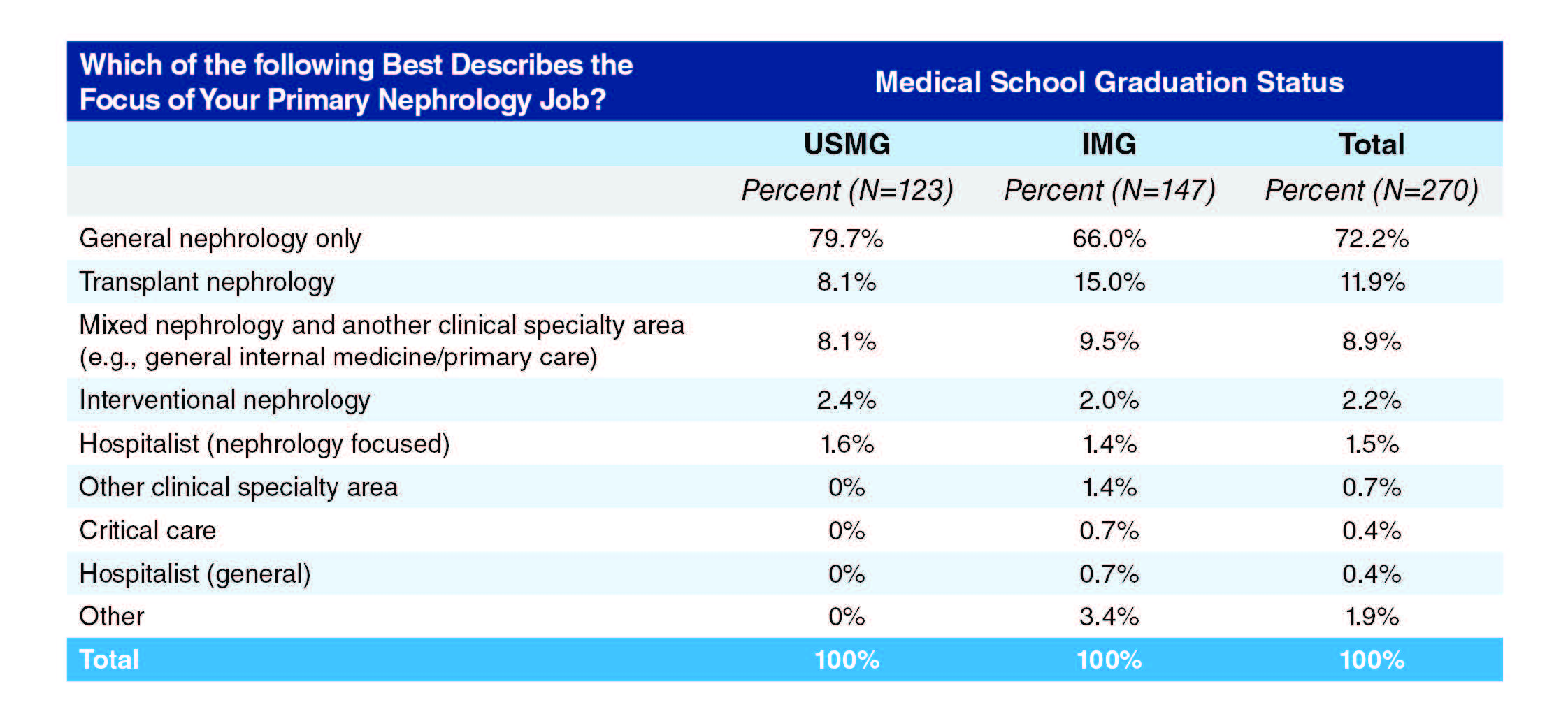
Exhibit 14 shows that those whose focus was general nephrology were more likely to be in group practice than academic practice settings (85.2% vs. 65.6%), while those whose focus was transplant nephrology were more likely to be in academic than group practice settings (21.3% vs. 3.3%).
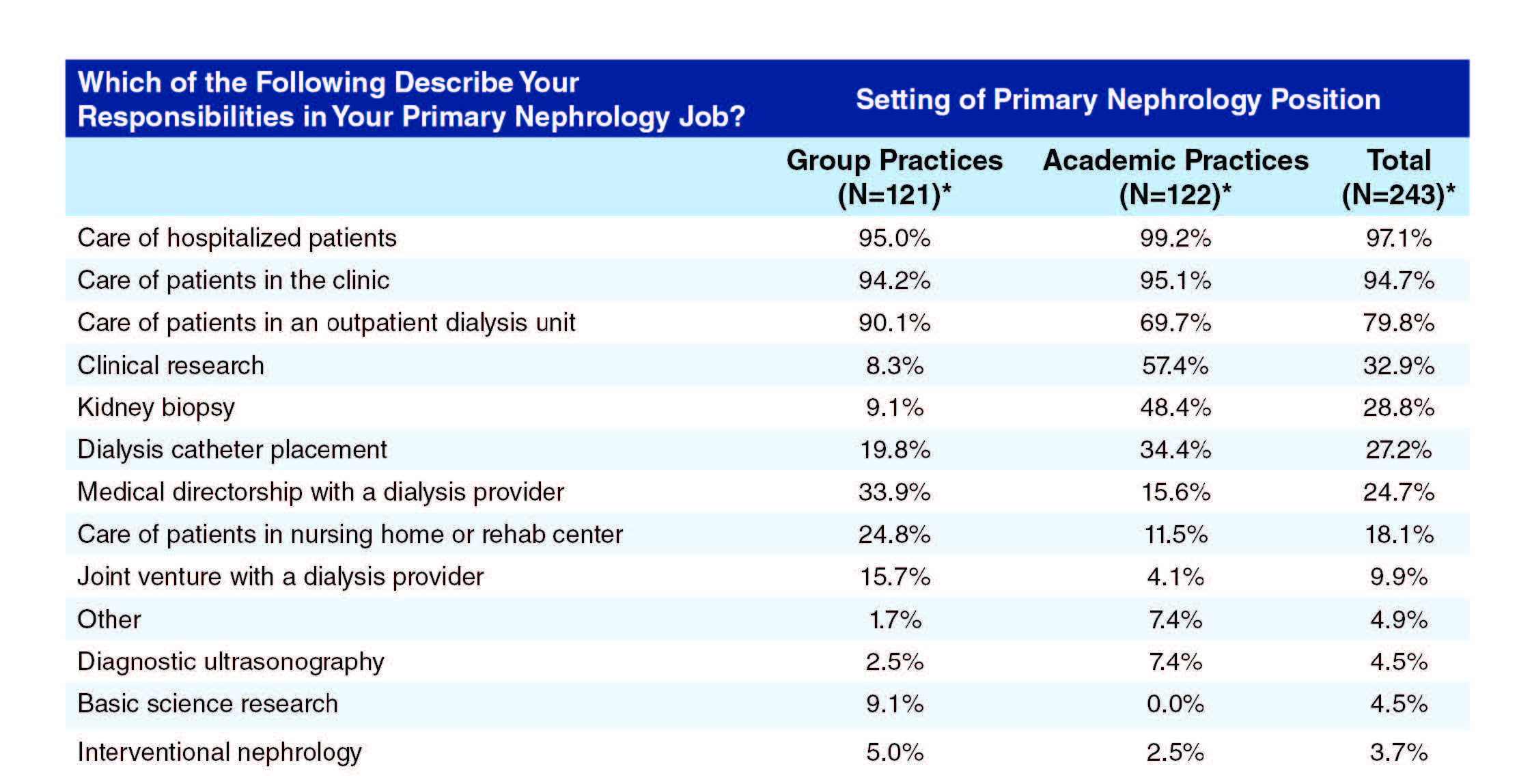
By far the most common job responsibilities were care of hospitalized patients (97.1% of respondents), care of patients in the clinic (94.7%) and care of patients in an outpatient dialysis unit (79.8%), as seen in Exhibit 15. Other responsibilities exercised by more than 10% of respondents were clinical research (32.9%), kidney biopsy (28.8%), dialysis catheter placement (27.2%), medical directorship with a dialysis provider (24.7%) and care of patients in a nursing home or rehabilitation center (18.1%).
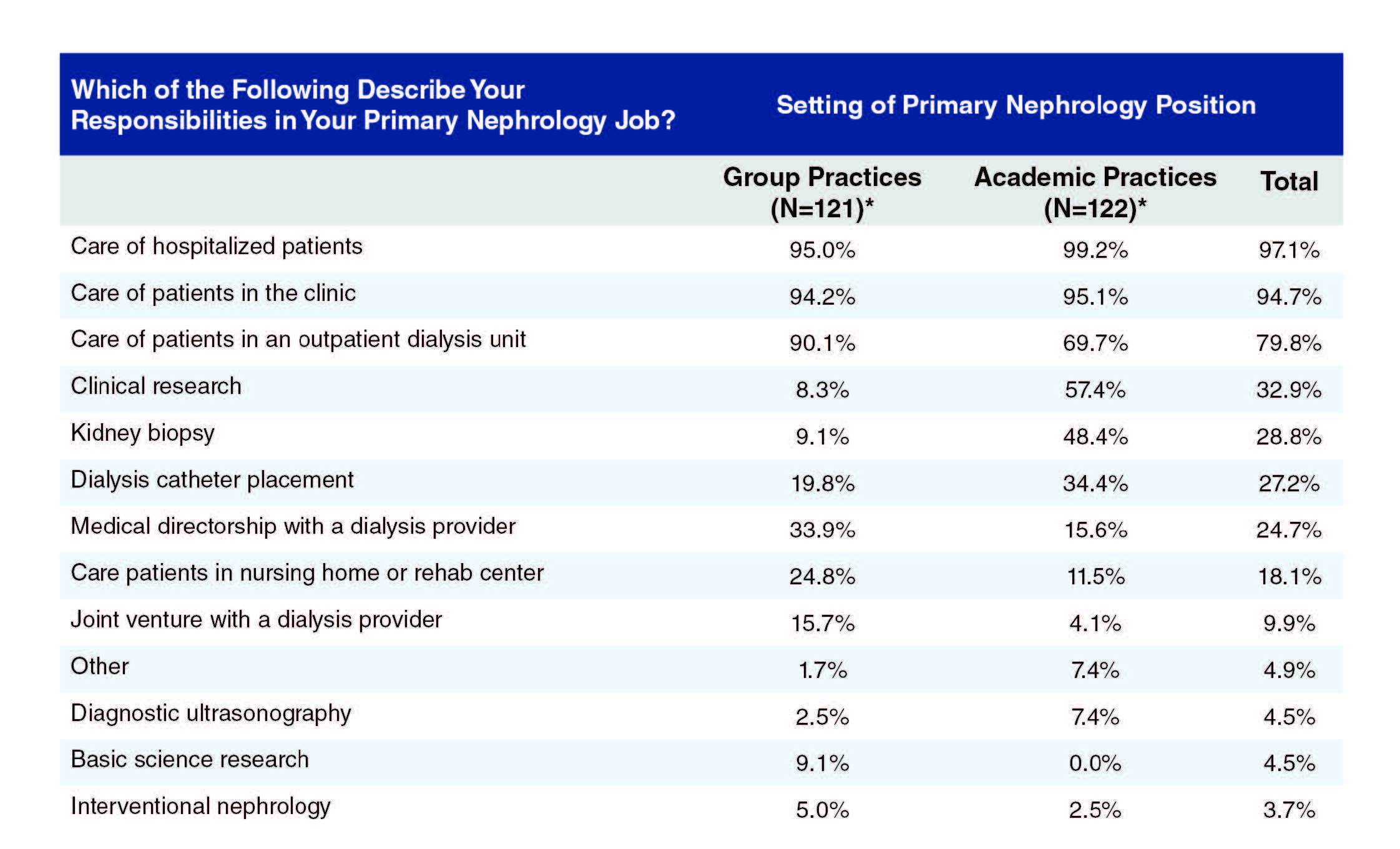
*Percentages are of those responding to any part of this question
Also from Exhibit 15, those in academic practices were more likely than those in group practices to have responsibility for kidney biopsies (48.4% vs. 9.1%), dialysis catheter placement (34.4% vs. 19.8%) and clinical research (57.4% vs. 8.3%), while those in group practices were more likely than those in academic practices to have responsibility for care of patients in an outpatient dialysis unit (90.1% vs. 69.7%) or in a nursing home or rehabilitation unit (24.8% vs. 11.5%) or to hold a medical directorship with a dialysis provider (33.9% vs. 15.6%).
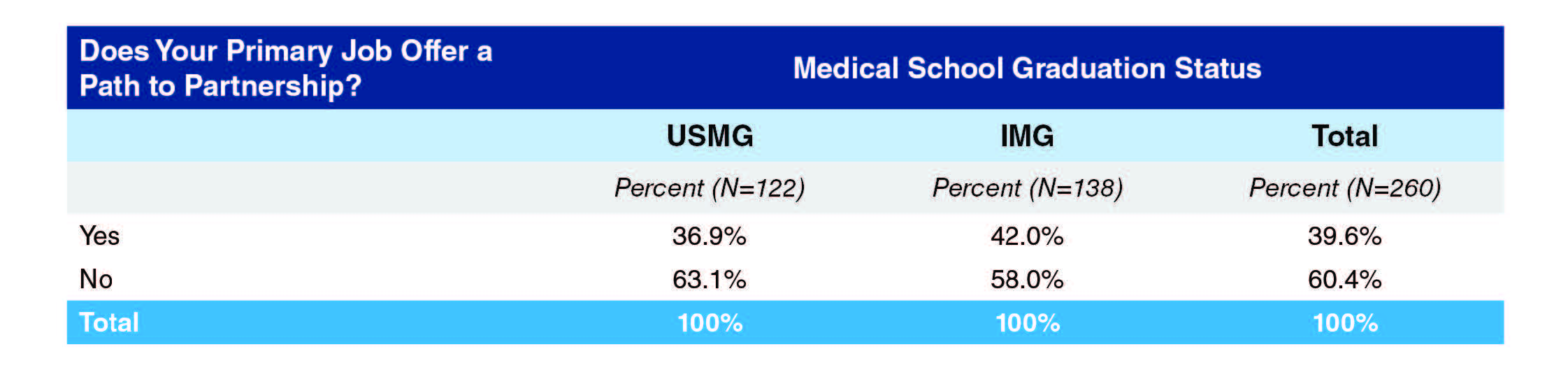
Not surprisingly, the vast majority of nephrologists in group practice (77%) said their primary job offered them a path to partnership; only 5.7% of those in other settings said they had a path to partnership (Exhibit 16).
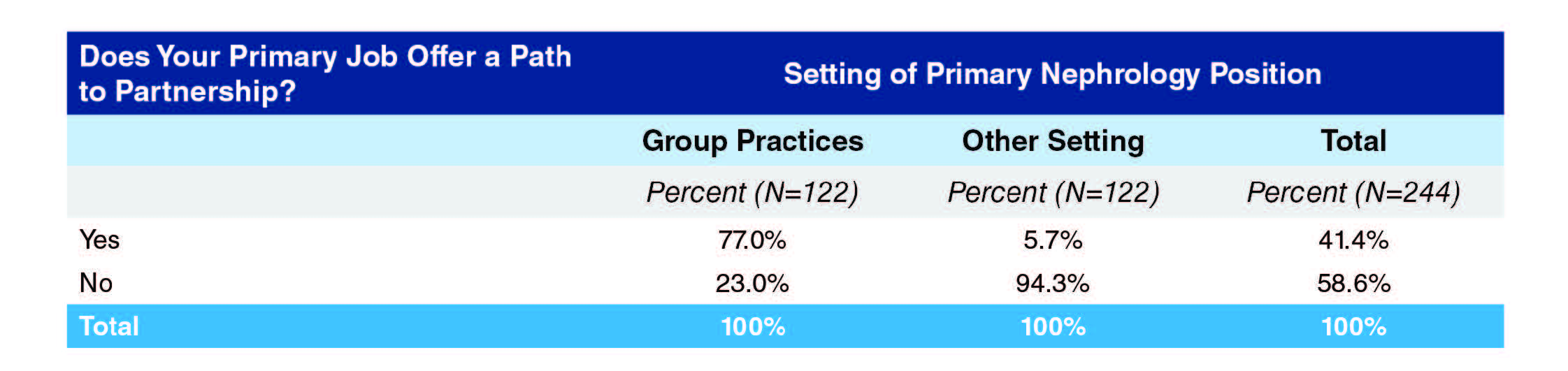
IMGs were more likely than USMGs to have a path to partnership (42.0% vs. 36.9%), likely because a higher proportion of IMGs than USMGs were in group practice.
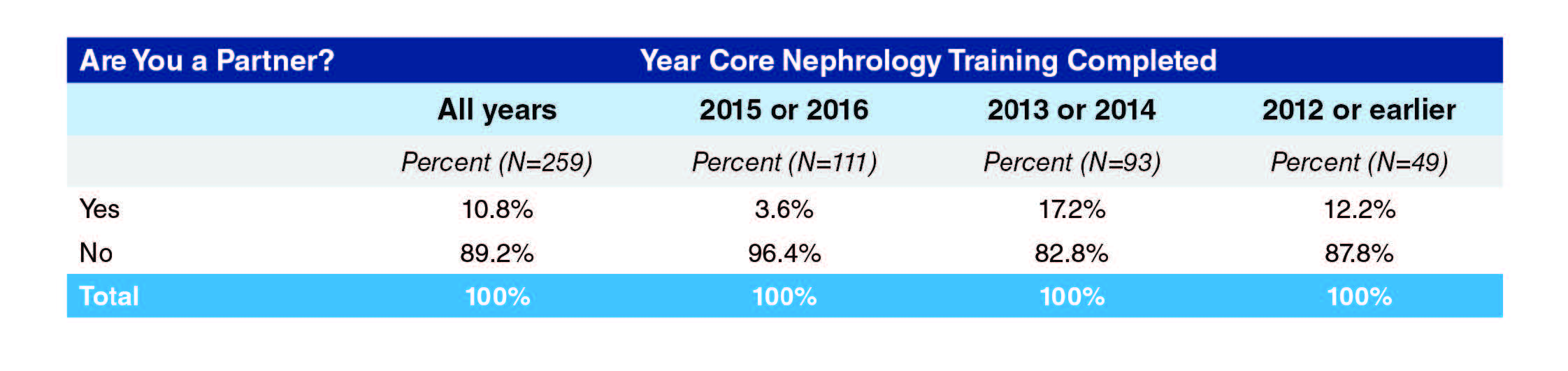
Overall, 10.8% answered that they were already a partner (Exhibit 18).
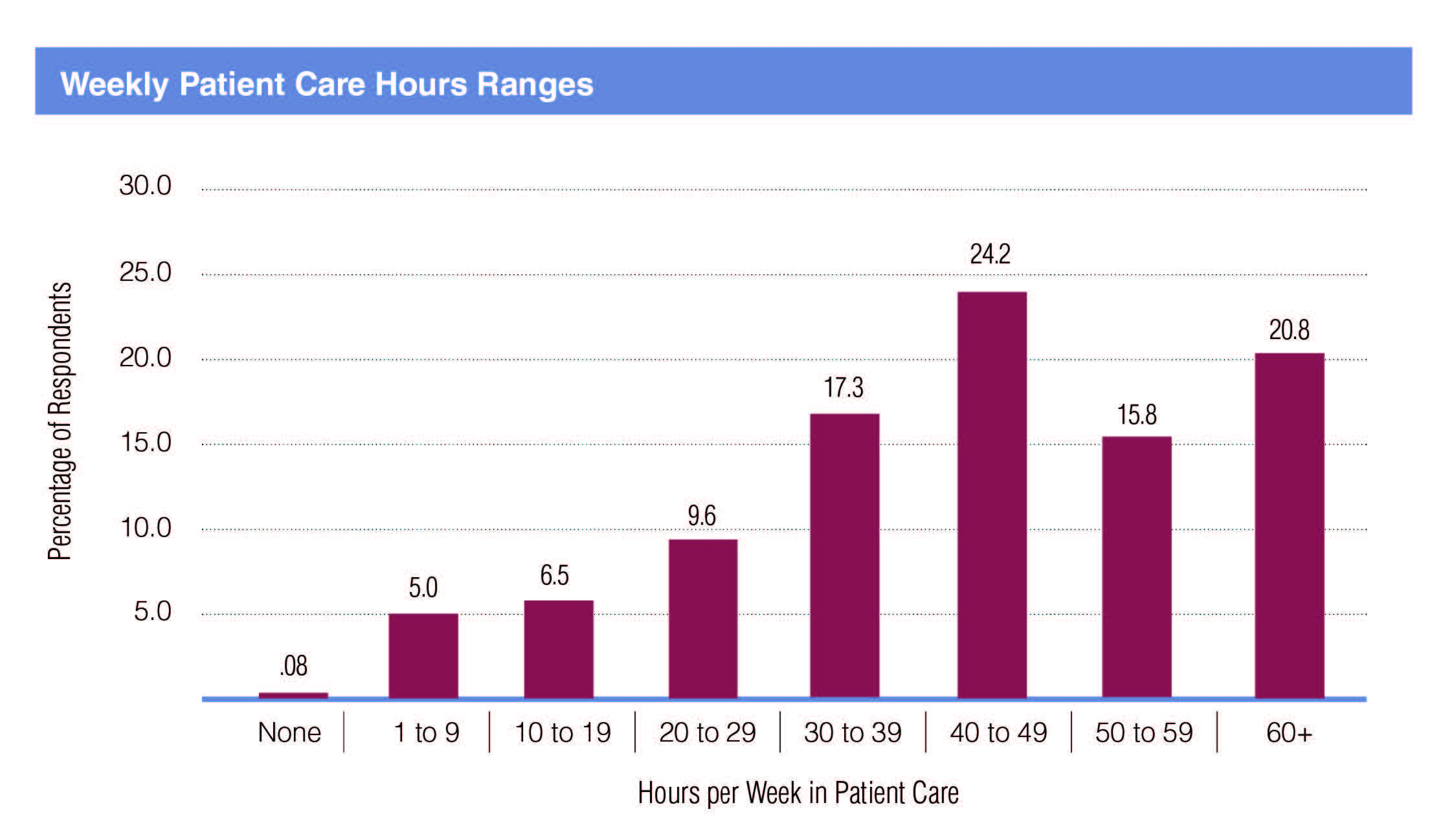
Over 60% of respondents reported spending at least 40 hours per week in patient care, with another 17.3% spending at least 30 hours weekly (Exhibit 19).
Respondents working in group practices were spending more time in patient care than those in academic practices, with 47.1% of them reporting 50+ hours a week of patient care compared to 13.6% of those in academic practices (Exhibit 20).
The most common incentives reported were support for maintenance of certification and continuing medical education (47.0%), relocation allowances (27.5%), career development opportunities (27.1%), income guarantees (25.0%), sign-on bonus (16.5%) and H-1 visa sponsorship (16.1%). Fewer than one in four (21.6%) reported no incentives. Of the 14 respondents who described ‘other’ types of incentive, 5 cited some kind of performance or productivity bonus and 2 more cited an annual bonus without saying how this was assessed.
Respondents from group practices were more likely than those from academic practices to report receiving support for maintenance of certification and continuing medical education (53.4% vs. 40.7%), relocation allowances (34.7% vs. 20.3%), income guarantees (33.1% vs. 16.9%) and a sign-on bonus (28.0% vs. 5.1%). Those in academic practices were more likely than those in group practices to report receiving career development opportunities (37.3% vs. 16.9%) and H-1 visa sponsorship (18.6% vs. 13.6%).
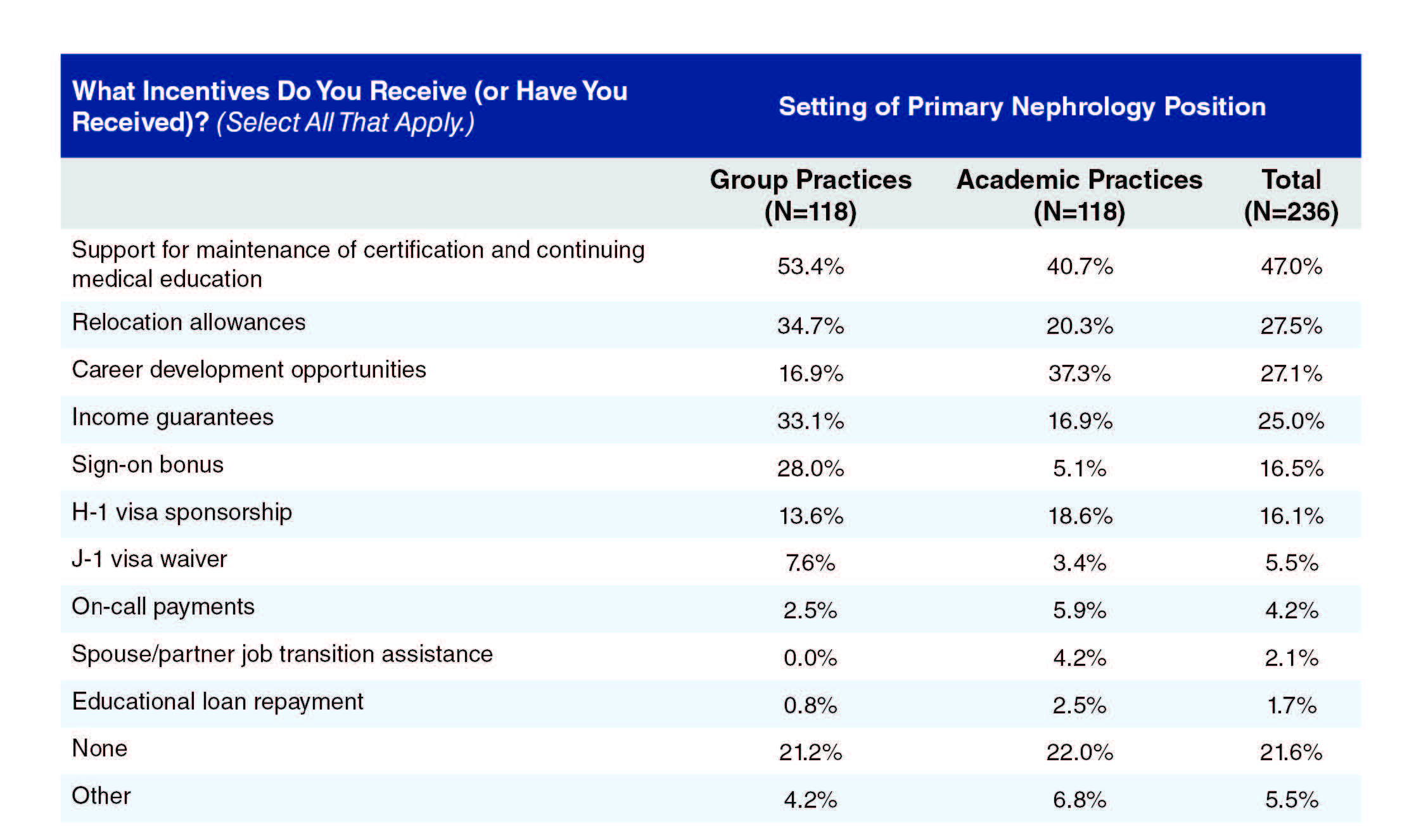
*Percentages are of those responding to any part of this question and can add up to more than 100% because respondents can indicate more than one answer
Evening and Weekend Responsibilities
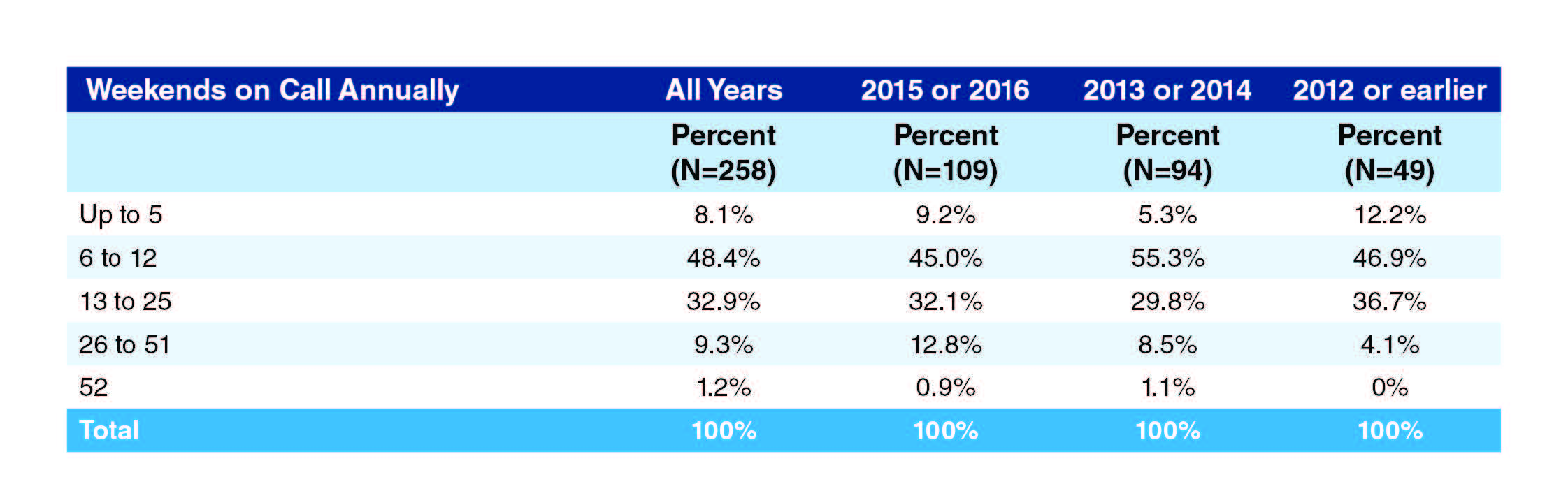
Only one in ten respondents (10.5%) were on call every other weekend or more, but 32.9% more were on call at least every fourth weekend. Most respondents (48.4%) were on call at least once every two months but less often than every fourth weekend. The proportion on call at least every other weekend decreased as the number of years out of training increased, with the proportion on call at least one weekend in two being 12.8% among those completing training in 2015 and 2016 compared to 4.1% among those completing training in 2012 or earlier. A corresponding change in those on call from 6 to 12 weekends annually suggests a general trend towards a lower on-call frequency as the nephrologist career progresses.
More respondents were on night call at least every other week than were on call every other weekend (29.7% vs. 10.5%) but, as with weekends on call, the largest group were on night call at least once every two months but less than every fourth weekend (31.7%).
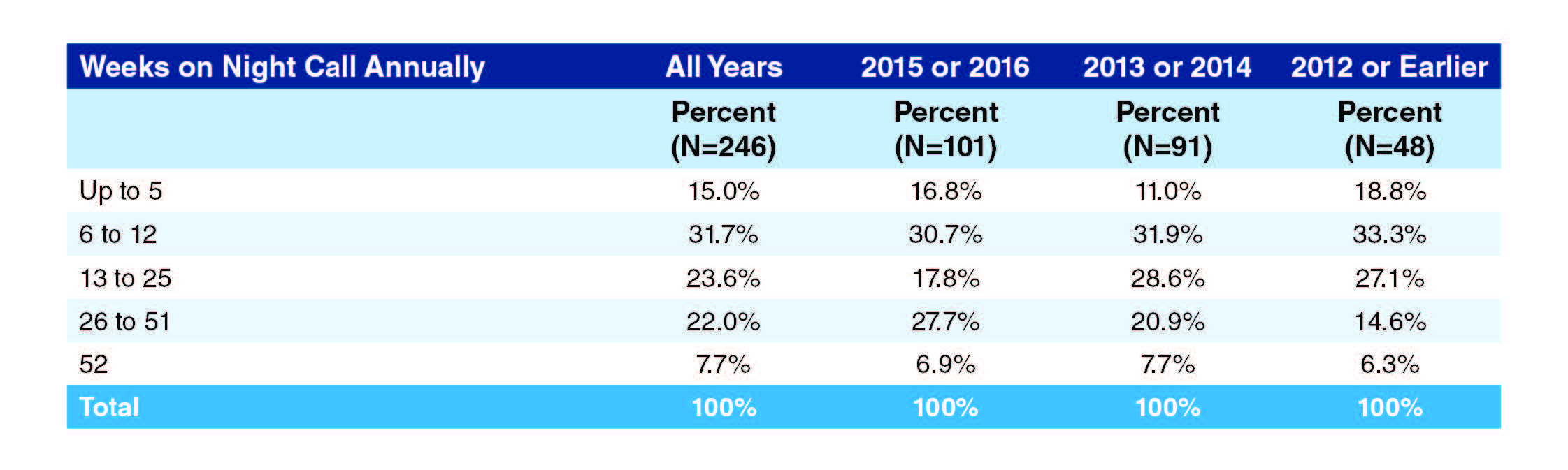
As with weekends on call, a general trend is evident towards a lower frequency of weeks with night calls as the nephrologist career progresses, with 27.7% of those completing training in 2015 and 2016 on night call at least every other week compared to 14.6% of those completing training in 2012 or earlier.
How far these trends toward reduced out-of-hours responsibilities as the nephrologist’s career progresses are explained by the switch from group practices to academic practices is unknown, but as Exhibits 24 and 25 show, those in academic practices are generally on call and on night-call less often than those in group practices: only 24.1% of respondents in academic practices reported being on call 13 or more weekends annually compared to 63.6% of those in group practices, while only 41.4% of respondents in academic practices reported 13 or more weekends on night call annually compared to 65.2% of those in group practices.
Procedural Responsibilities
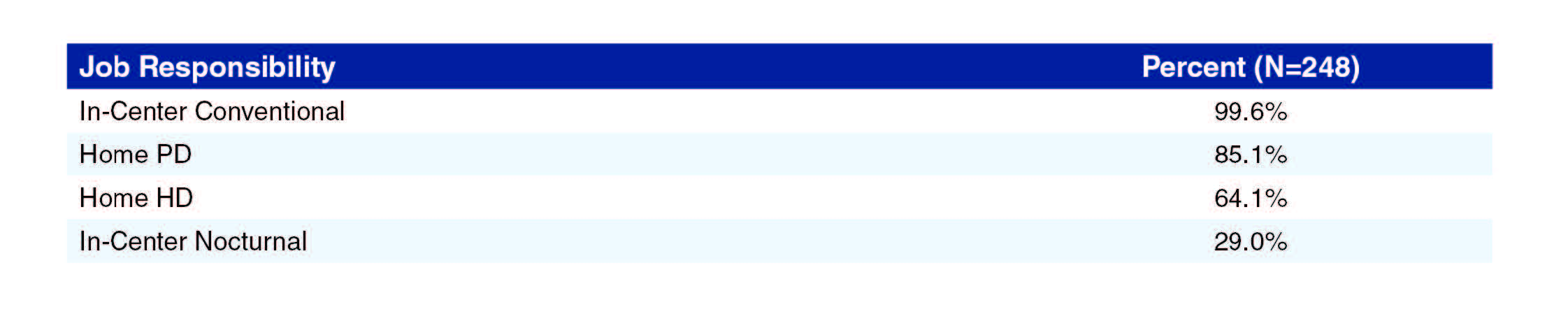
The most common dialysis modalities offered were in-center conventional (99.6% of respondents), home PD (85.1%) and home HD (64.1%), with in-center nocturnal much less common (29.0%).
CRRT was the most frequently performed procedure and only 15% of respondents did not perform CRRT; temporary dialysis catheter placement was performed by 48.3% of respondents and kidney biopsy by 46.3%. Renal ultrasonography, tunneled catheter placement and PD catheter placement were all performed relatively infrequently.
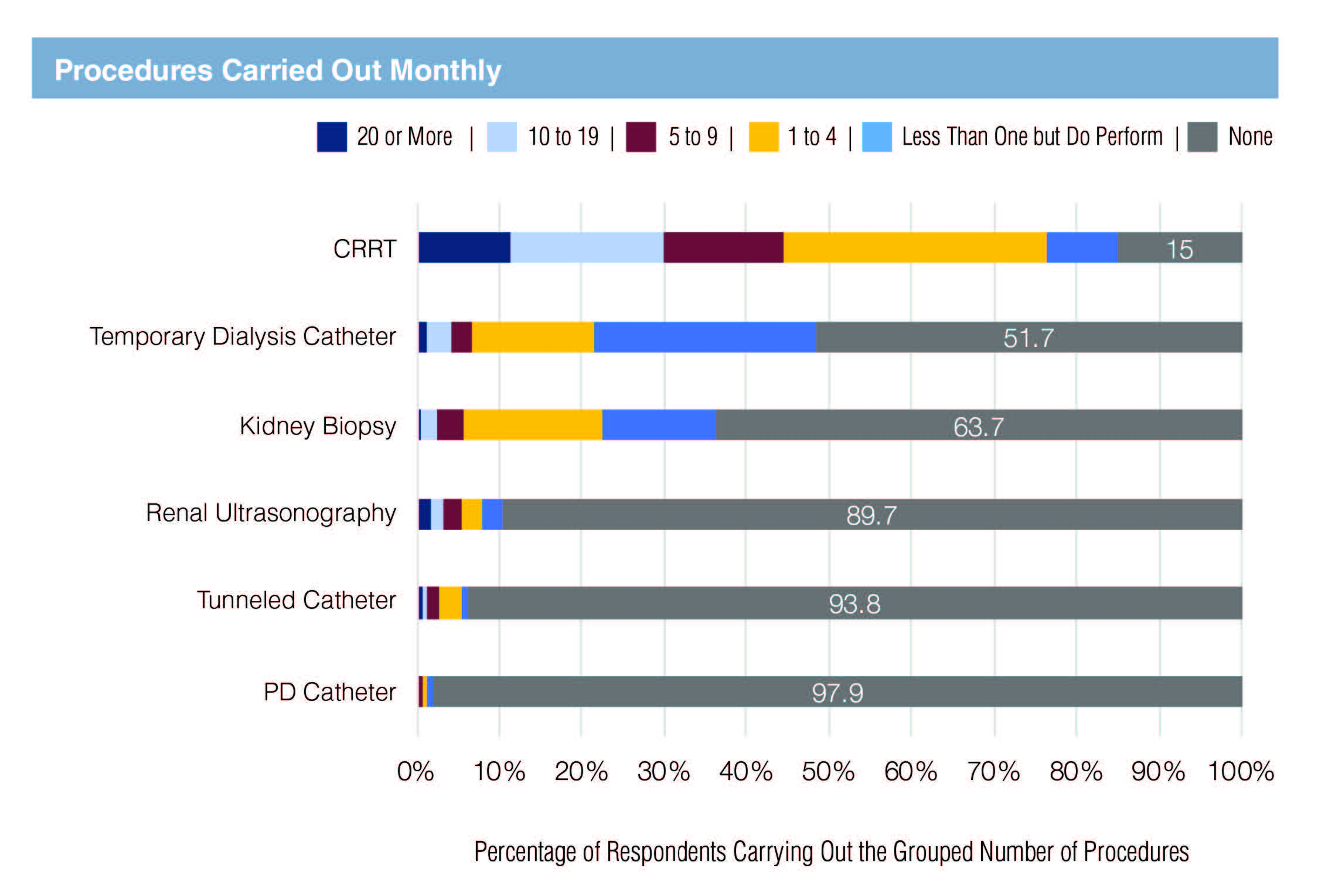
In general, those in academic practices were more likely than those in group practices to report performing procedures such as CRRT, temporary dialysis catheter placement and kidney biopsy (Exhibit 28).
Salaries
Mean income (based on midpoints of $10,000 ranges) indicates that males were earning around $30,000 more on average than females, while there was little overall difference between USMG and IMG average salaries (Exhibit 29). The median salary, which is less sensitive to outliers, told a similar story, with the overall median in the range $180,000-$189,999 and male and female median salaries around $20,000 apart.
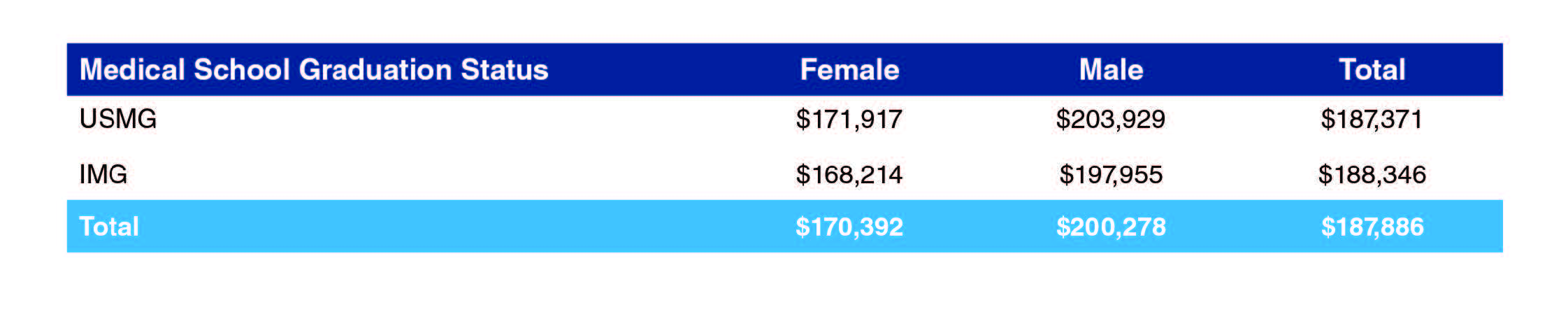
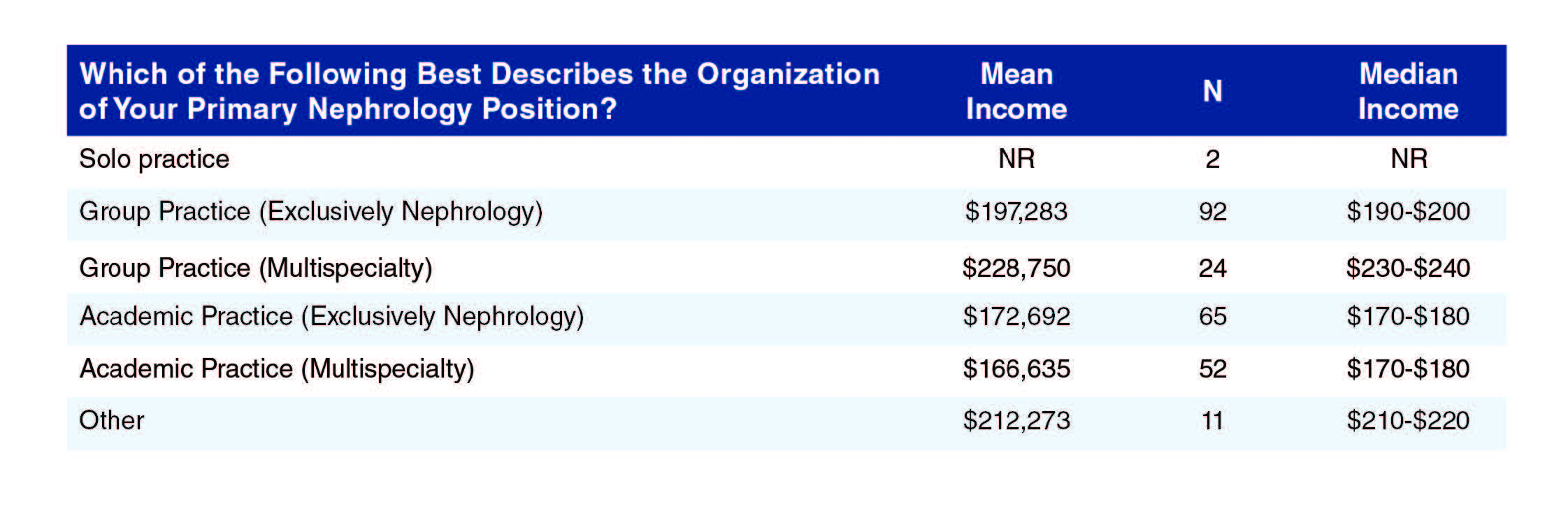
Exhibit 30 indicates that nephrologists in group practices were earning more than those in academic practices, as can be seen by differences of around $25,000 in exclusively nephrology group vs. academic practices and more than $60,000 in multispecialty group vs. academic practices. The highest earnings were reported by those in solo practices ($235,000) though with only two respondents in this category this result may not be representative. Five of the respondents included among the ‘other’ settings reported being based in hospitals (excluding one based in a VA hospital), with average earnings of $221,000, roughly comparable with earnings at multispecialty group practices.
NR: Not reportable; too few responses.
Splitting the salary data by sex and contrasting group with academic practices (Exhibit 31) reveals a pattern of males earning more than females in both types of setting, but with a much bigger male-female differential in group practices ($41,000) than in academic practices (around $10,500).
The pattern is less clear, but still evident, when comparing median salaries (Exhibit 32).
IMGs reported higher salaries than USMGs in group practices (by about $5,500) but lower salaries than USMGs in academic practices by more than $20,000 (Exhibit 33). This presents a somewhat different story to the apparent overall similarity of IMG and USMG salaries reported above in Exhibit 29. The pattern is similar but less pronounced in median salaries (Exhibit 34).
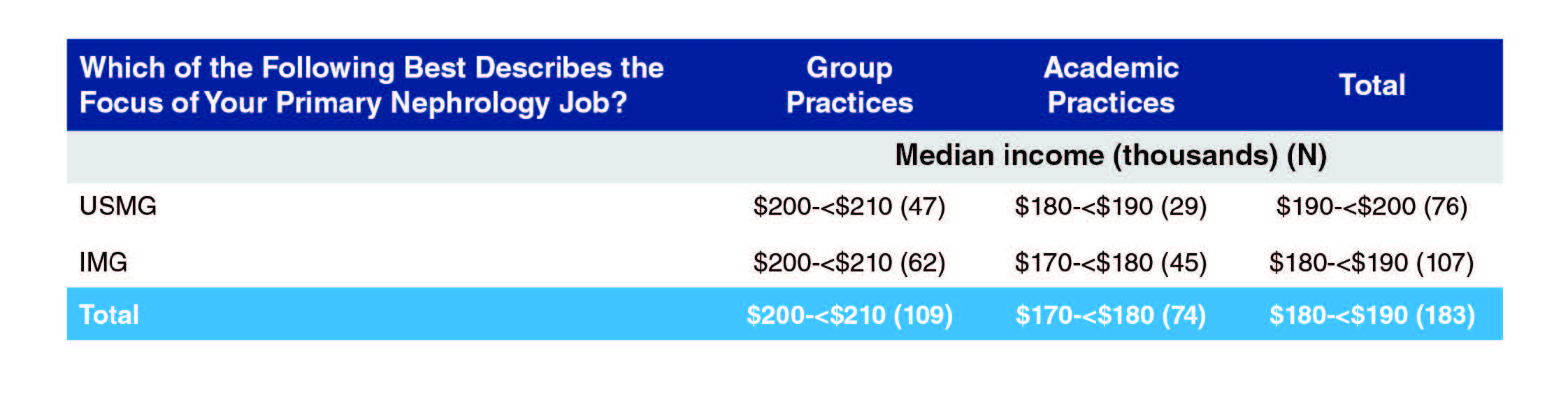
Transplant nephrology and general nephrology were the highest paid branches of nephrology ($192,000 and $189,699 respectively), with general nephrology far and away the most common focus reported (73.8% of respondents who supplied salary information on their primary nephrology job). Nephrology-focused hospitalists and interventional nephrologists reported the lowest salaries though the numbers involved were small, amounting together to only 4% of the respondents. Median salaries told a similar story.
Perhaps surprisingly, it was respondents who had completed core nephrology training in 2012 or earlier who reported the lowest salaries, more than $10,000 less on average than those who completed training later. This is most likely a consequence of the higher proportion in academic practices, where reported earnings are substantially less than in group practices.
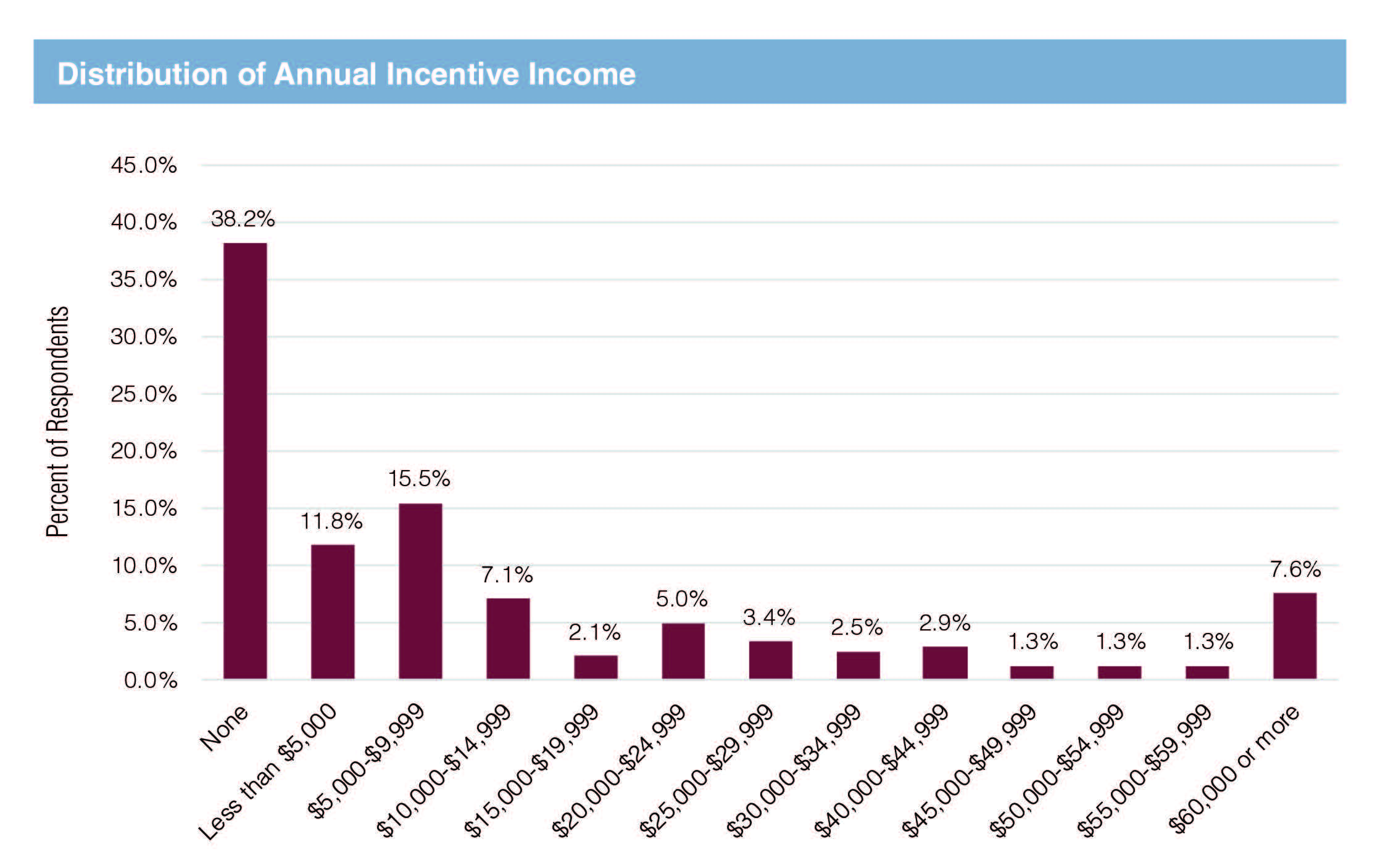
Just over 60% of respondents reported some incentive income, though only about a third overall (34.5%) reported incentive income above $10,000 annually. Only one in five (20.3%) reported incentive income above $25,000 but with about half of this group (10.2% of all respondents) reporting incentive income greater than $50,000.
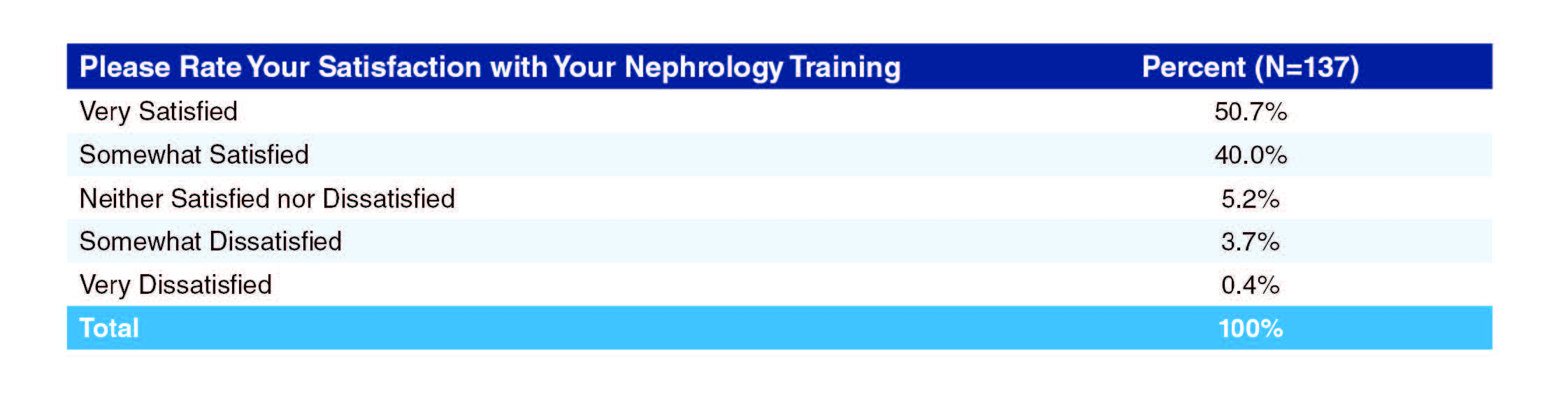
Satisfaction
While only a few nephrologists were dissatisfied with their nephrology training, only a bare majority of respondents (50.7%) were very satisfied, with USMGs a little more satisfied than IMGs (54.5% vs. 47.6% very satisfied respectively) and males a little more satisfied than females (53.5% vs. 47.8% very satisfied); a larger majority (62.5%) still strongly agreed that they were adequately prepared for nephrology practice by the end of their fellowship and only one respondent (0.4%) said they did not agree they were adequately prepared for practice. Differences in nephrology training satisfaction according to practice setting were not significant.
USMGs were much more likely to report being very satisfied with their overall salary than IMGs (28.1% vs. 12.2%), while IMGs were more likely to be very dissatisfied than USMGs (10.2% vs. 6.6%).
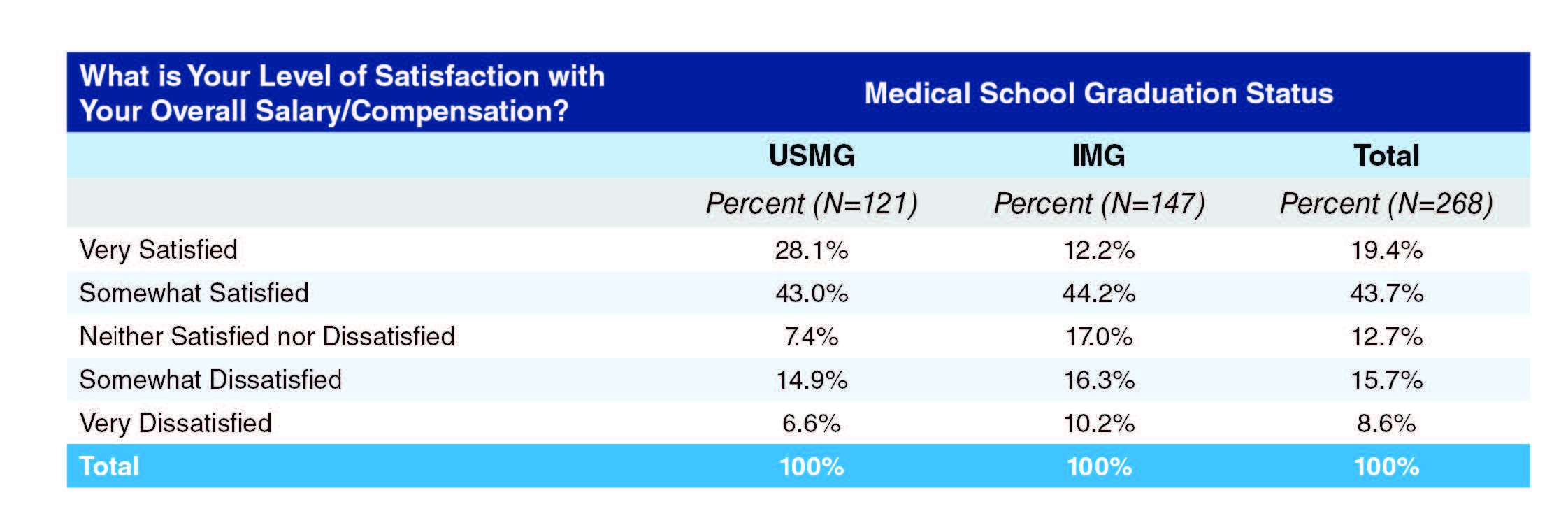
There were no significant differences in satisfaction with overall salary/compensation between group and academic practice settings (Exhibit 40).
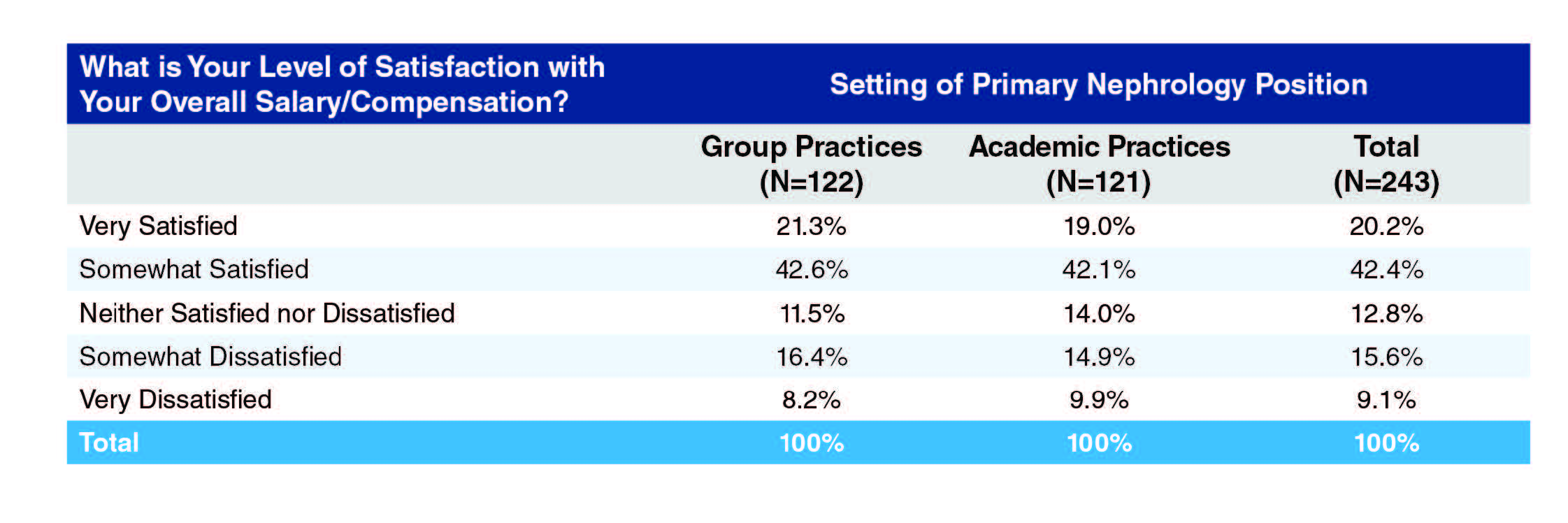
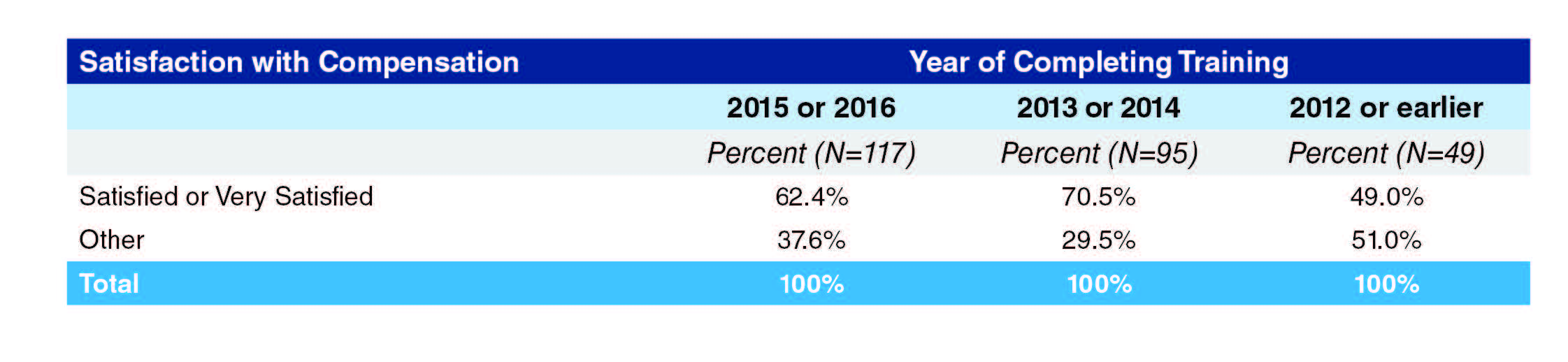
Satisfaction with compensation was highest among those who completed training in 2013 and 2014, with 70.5% satisfied or very satisfied with compensation compared to 62.4% of those completing training in 2015 and 2016. Only 49% of those completing training in 2012 or earlier were satisfied with compensation, likely reflecting the higher proportion in academic settings where earnings are lower than in group practices.
Respondents were very positive indeed about the quality of patient relationships and intellectual challenges in nephrology (93.2% and 92.5% positive or very positive respectively). They were least positive about administrative duties (30.2%), geographical job distribution (33.2%) and job opportunities (34%).
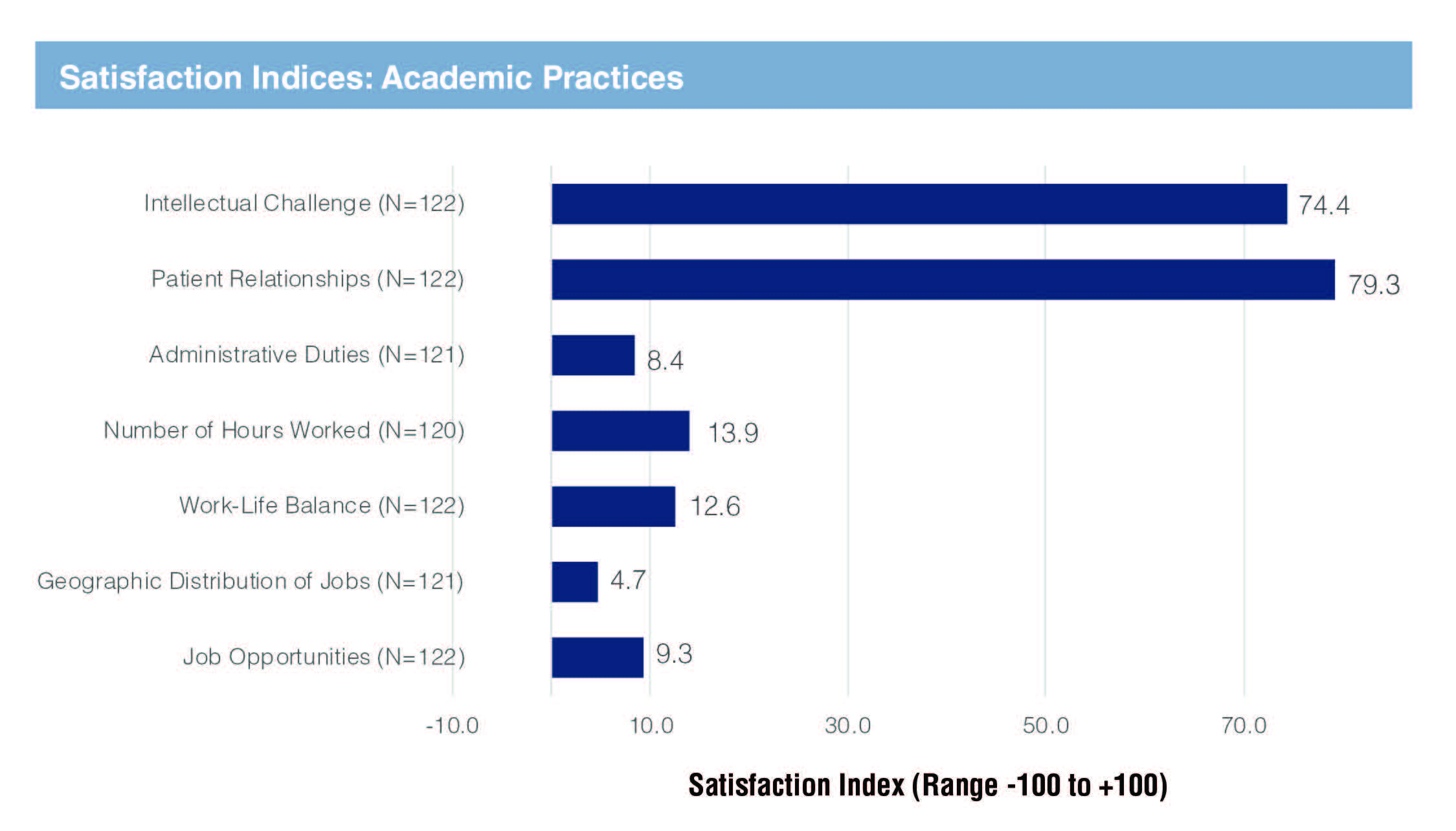
Using a satisfaction index obtained by awarding scores from -100 to +100 based on responses, respondents from academic practices were more satisfied than those from group practices in regard to patient relationships (satisfaction index of 79.3 vs. 70.1), number of hours worked (13.9 vs. 2.5), work-life balance (12.6 vs. 0.4), job opportunities (9.3 vs. -5.4) and geographic distribution of jobs (4.6 vs. -2.5). Satisfaction on intellectual challenge and administrative duties was about the same in both groups.
Respondents in academic practices were also more satisfied than those in group practices with their current position (41.3% very satisfied vs. 33.1%). Overall almost 80% were somewhat or very satisfied with their current positions.
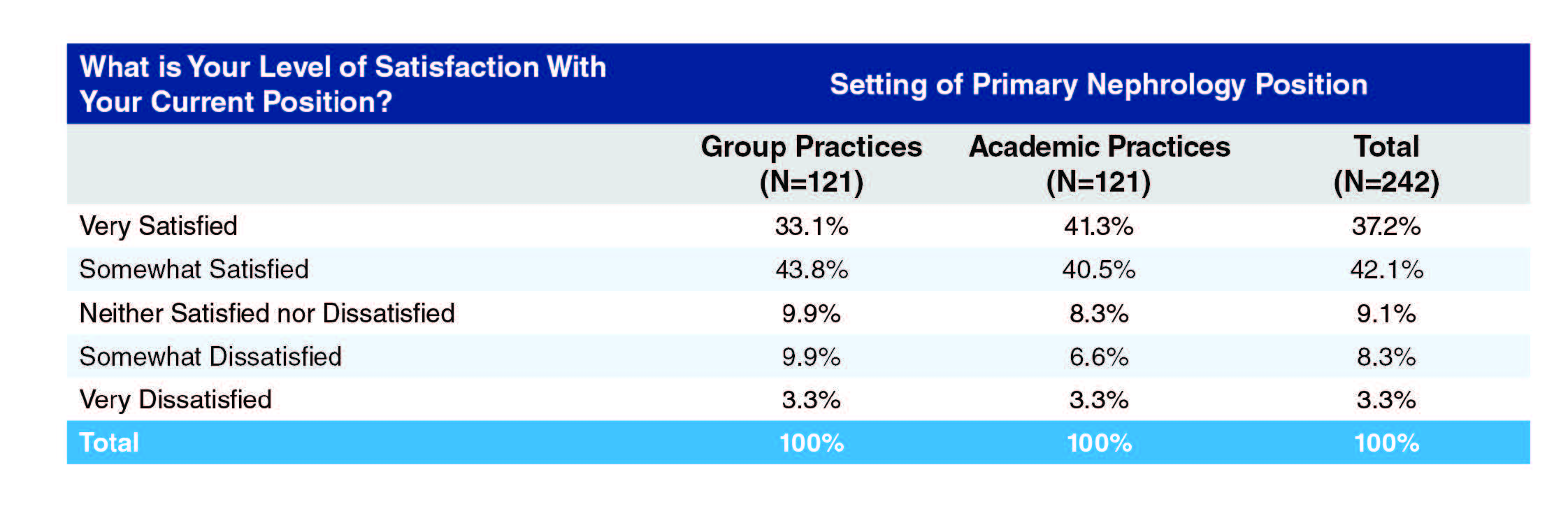
Despite the high level of personal satisfaction with some aspects of nephrology, a quarter of respondents did not feel they could recommend nephrology to current medical students and residents, with respondents from academic practices more likely than those from group practices to recommend nephrology to medical students and residents (81% vs. 69.7%, Exhibit 45). USMGs were more likely than IMGs to recommend nephrology (77.7% vs. 72.1%, Exhibit 46).
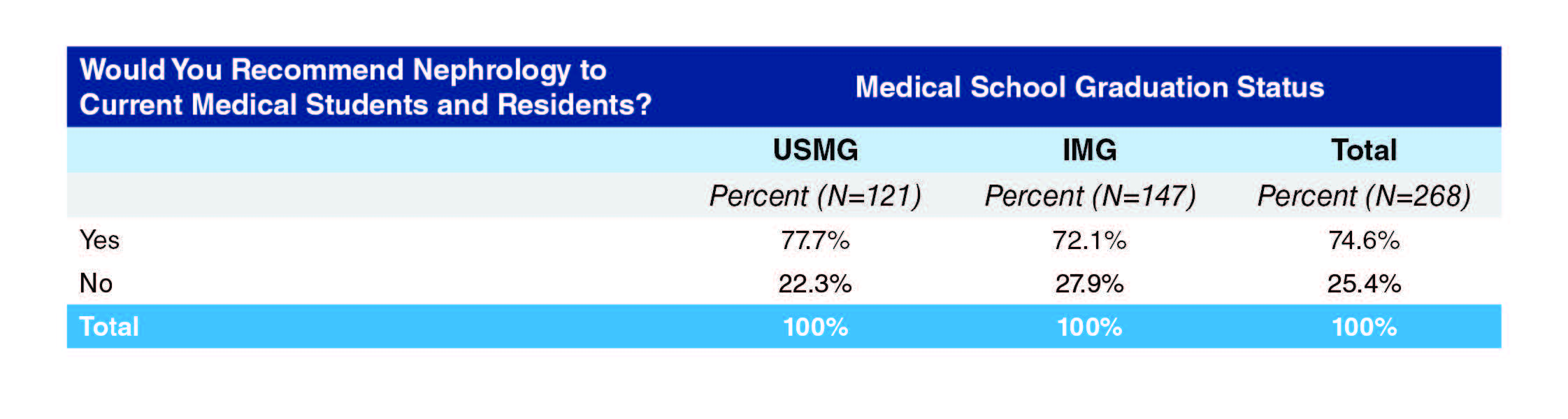
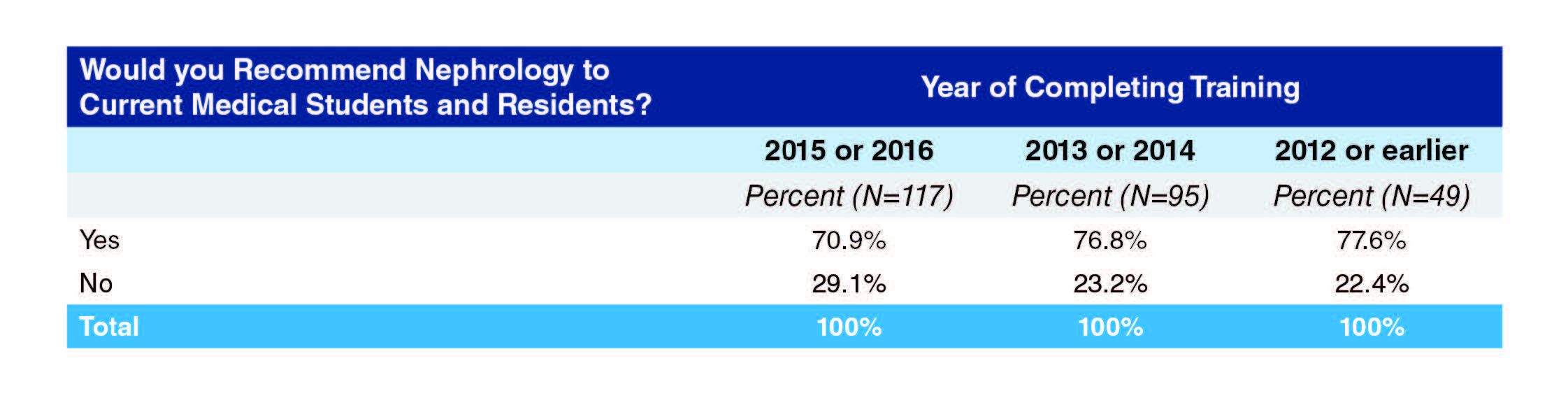
Respondents who completed training at least three years ago were more positive about recommending nephrology to medical students and residents (76.8% and 77.6% compared to 70.9%).
Reasons for Recommending
Many respondents cited the challenge, intellectual stimulation and variety/interest of the field. Though some were concerned about low pay and poor work-life balance, the extent of concern about these issues varied depending on the particular position held by the respondent. Many of the respondents saw in nephrology a more traditional physician role with close doctor-patient relationships, the stimulation of varied practice challenges, and the vocational rewards attendant on improving patients’ lives.
My love for nephrology makes it hard for me to understand why there is lack of interest in this field. It offers deep understanding of physiology, offers variety of paths including transplant, dialysis including home modalities, Glomerular diseases, stones, acute/critical care, Onconephrology , interventional etc. There is no lack of job opportunities either and life style is decent.
Nephrology - when practised in all its diversity, has a wide spectrum of problems, techniques and modalities to understand and use. From diseases as common as just HTN and diabetes all the way to complex autoimmune conditions, it mandates that the practitioner be an excellent internist, good with hands on skills and good with just business sense. Finally, with nephro, balancing your regular life out can be easier as compared to other fields. The remuneration is satisfactory in the long run.
Nephrology is certainly disappointing when it comes to compensation. However, it’s extremely interesting and mentally challenging medical specialty. If you like diagnostic and therapeutic challenges, you will enjoy the specialty.
Nephrology is the closest thing to traditional Internal Medicine practice. We develop relationships with our patients and see them in both the inpatient and outpatient setting. It is extremely rewarding. Nephrology is challenging and never dull. In academic nephrology I have had the opportunity to focus on what interests me the most and continue to improve nephrology practice through research.
Promotes critical thinking, care of the whole patient, challenging, rewarding, Long term patient physician relationships
There is a good mix of inpatient and outpatient care as well as variety to your day with rounding at the dialysis units. Of the inpatient consults, there is a mix of routine and critically ill patients. You are able to both see your impact over time as well as your impact within just a few hours once a patient’s labs or clinical status improves.
It remains to be a very interesting subspecialty of medicine and very challenging. It provides many opportunities to impact patients’ lives for the better
Interesting pathophysiology, good schedule, lots of teaching opportunities in academic practice, potential for research.
I enjoy long term care of patients. I like the diversity of disease processes that I deal with on a day to day basis. The changing clinical settings that negotiate in a week including inpatient, outpatient, dialysis units keeps me engaged.
Despite flaws in the specialty, I still find it to be very rewarding for the reasons I chose it as a specialty. I enjoy the complicated patients along with the investigative work it takes to determine cause of their kidney related diagnosis. It’s fun to think about the physiology and how that explains a patient’s renal or fluid/electrolyte/acid base abnormality. There is a lot of flexibility in the specialty in terms of hospital based work vs outpatient work. Nephrologists generally can find a position that fits with their interests and lifestyle.
An aspect medicine I find very relevant and interesting. A nephrologist is specialist but still somewhat involved in the general care/overview of the patient.
Reasons for Not Recommending
The reasons respondents gave for not recommending nephrology appeared to represent a difference in weighting between the positive and negative aspects of the profession, with each nephrologist weighing things differently according to the interests, sense of personal reward, and the position they held. Although the negatives included high workload and low pay, many of the responses regarded these as impacted significantly by practices themselves and reflected on the vulnerability of new nephrologists entering the field to unfair contract terms. In addition, some negatives (such as having to care almost single-handedly for a critically ill patient) would be regarded as positives by nephrologists who valued the more traditional physician role exemplified by such a case.
I like the pathophysiology very much and highly interested but I will NOT recommend them nephrology because private practices are NOT honest and fair to their juniors associates in terms of partnership track and incentives. There is literally no security in the practices that you will get the right partnership track in the end. Low salary to begin with poor incentives. There is a lot of dishonesty in this specialty in terms of honesty among the private practices. I heard lot of cases that after 3 or 5 years of practices, practices do not offer the partnership track. Good friends of mine, who came to this specialty because of me, joined the hospitalist once done with their fellowships due to above stories. That’s the main reason people are leaving the nephrology and entering into hospitalist jobs. There is a good security and incentives in hospitalist job and more time to your family. I would like to recommend to students and residents but they stated me above reasons. That’s why they do not want to join the nephrology specialty. We need to fix this above main issue. The other main issue is visa for foreign graduates. Not many IMG, getting into residency training due to visa issues.
Lifestyle limiting in small practice, frequency of call and hours worked, including on call return to hospital requirements, moderate compensation for time requires.
After 3 years of private practice as an associate nephrologist in [state], I resigned from my first Nephrology job since graduation due to an unfavorable partnership contract. I would caution residents with interest in Nephrology about the hostility to new graduates in the [state] area with relation to its competitiveness and also high risk of being taken advantage of. Private practice Nephrology is very work intensive, and the [state] area is saturated. I would caution that the partner level salary is barely higher than that of Hospitalist, which is one reason why my current job is a Nocturnist. I may return to Nephrology in the future if the contract is fair or favorable.
Although I love practicing what I do, and that is the reason I have continued practice in nephrology for last 5 years, despite many newer job opportunities (e.g. hospitalist, work from home- as peer reviewer with insurance companies, etc.); this branch sets you up for very long and busy work days, lots and lots of commute to get to various satellite dialysis clinics and outpatient/ CKD clinics, very poor reimbursement ( I am being paid much lower than a fresh family medicine graduate at the same practice despite much higher patient volume and wRVUS!!!), no time or mentorship for career advancement due to many responsibilities; and thus, a very high rate of burnout. I would hate for any enthusiastic student or resident have to make tough decisions like the ones I am faced with, so early in their career. • Getting a good nephrology practice is difficult these days. Most practice never keep their promises and overwork newly employed nephrologist.
I love nephrology itself, but the job market is very draining on a nephrology physician and I don’t think the specialty is recognized as well for the care we provide. I do believe the nephrology community itself is responsible for this situation. We haven’t promoted ourselves as aggressively as we should have so far.
Not enough compensation for the workload transportation time and responsibilities required A better quality of life could be had as a hospitalist with an interest in nephrology. The field is misunderstood by Business and therefore the important and mentally time consuming work is undervalued and our productivity is undervalued based on the lack of billable procedures. Many become burned out by the realities of the field at this time and therefore while I could encourage someone with an interest already but at the same time I would encourage them to make an informed decision which was in fact the same advice I was offered before I went to fellowship.
Not all nephrologists compensated appropriately for the amount of work and involvement of our patients. Part time options are not really part time and people complain that they end up working full time for part time pay.
The field isn’t what I joined it for. I joined for the opportunity to take care of seriously ill patients with interesting physiology; what I got was essentially preventative care with CKD, non-nephrologists having little respect for our opinion on critically ill patients, and a terrible salary-to-work ratio. To top it off, we’re losing turf to other providers. The current fellowship crisis stems from people seeing how miserable our situation is. Despite how much I love nephrology, critical care offers better opportunities for the ICU-inclined, and rheum offers better opportunities for interesting outpatient care with a better salary. I likely would still choose nephrology for myself, but cannot in good conscience recommend the mess that the specialty is to others right now unless they have a specific kidney research bent or some other factor that outweighs our issues.
What ASN Can Do To Support Careers in Nephrology
Responses fell into three main categories:
1. Lobbying & Advocacy, mainly around pay and reimbursement but also for immigration issues, for defending the role of the nephrologist
Dramatically reduce the number of nephrology fellowship so the demand and supply ratio is balanced. Reduce regulations faced by kidney transplant programs. Reduce regulations faced by dialysis units so that it is easier for a nephrologist to own dialysis units.
We have a shortage of people going into Nephrology and a large burnout rate (especially in private practice). I think that improving reimbursement in Nephrology is key to recruitment of future Nephrologists. It is a tough job with a lot of call/weekend responsibilities. It is disheartening to see that the reimbursement for a starting Nephrologist is less than a hospitalist, especially given the difference in work hours.
Intensified lobbying efforts for enhanced reimbursement
Lobby for better compensation for the care we do, working to re-establish our role in nephrology care issues like diagnostic procedures or interventional procedures.
By highlighting the practices in US that are abusing budding nephrologist on visa
Do a better job of explaining to Congress the need for J1/ H1 visas for nephrologists since a very high proportion of the physicians in this field are on waivers and they face a lot of trouble with regards to immigration. That coupled with a low paying job is driving a lot of IM residents to go for hospitalist jobs. Need to offer varied educational programs at ASN, geared not only to fellows (clinical education) but also those aimed towards people in practice (QI, business aspects of the field, etc.)
Not quite sure how ASN can be of help. More employers having idea about visa sponsorship needing professionals like me would help finding a good place to work.
Please save nephrology as a specialty, by maintaining higher standards for nephrology fellowships, limiting newer nephrology fellowship programs, and stemming the oversupply of (sometimes inadequately trained) nephrology applicants into a market with limited job opportunities.
2. Education, including appreciation of educational opportunities provided already by ASN
Continue great educational opportunities such as neph sap
Continued grant support Continued offering of CME materials such as NephSAP and special CJASN series (physiology, glomerular disease etc) I appreciate the educational content and funding opportunities that ASN provides.
More opportunities to appreciate the complexity of medical billing and the business of medicine, specifically nephrology.
3. Support and Mentoring in Job Search and Contract Negotiations, as nephrologists move into their first practice positions
ASN needs to work with private practices to mandate them to have high base salary and have a structured contract for partnership track. In this way, the new comer feel more secure. I am wondering if we do not work on above then this wonderful and pivotal specialty will be obsolete.
Continue to offer resources connecting young nephrologists with mentors in the field. Encourage training programs to expand the scope of training/ teaching; identify and enable the programs that are training future leaders with expanded skill sets.
Continue to work to support women in the field by continuing support networks and trying to create an atmosphere of full disclosure (as to fair pay to disclose the salary discrepancies that arise between men and women in the same job fields with the same experience)
Fellows need to learn about the business of nephrology. Unfortunately, there are many practices where physicians take advantage of the lack of knowledge of the business of nephrology recently graduated fellows have.
Find ways to guide those early in their careers to make the best of this profession, given the increasing regulations and less than ideal compensation.
I would have liked some guidance when I was looking for a job. My mentors in an academic setting couldn’t help. I would have liked to ask about - How many hospitals rounding at - How much windshield time - How does weekend coverage work I would have liked a better understanding about the loss of work life balance and would have liked to know what I was sacrificing when I took on my first job.
Set up some kind of network for graduating fellows to find jobs more easily. Right now, it’s all by word of mouth.
Mentorship programs are important and helpful. I had tremendous mentors in fellowship I hope all young nephrologists have this opportunity
4. Other
I think it will be difficult as most of the issue is a problem related to the market (salary, for life style just is not there bottom line). ASN is a great academic resource though.
Advocate strongly for policy changes to better support not only research but care for renal patients. More nephrology training and exposure at student and resident level. Aggressive promotion of the importance of specialty. The above will lead to increased recognition of renal problems, of the importance of nephrology care, and hopefully progression to early intervention programs. I am aware that ASN is actively involved in above currently.
What ASN Can Do To Support Efforts To Offer The Best Quality Care
Many of the responses were highly complimentary about ASN’s efforts to support quality care, while others made suggestions for improvements. Comments fell into five areas: professional educational activities, production or endorsement of guidelines, improved quality measures, professional empowerment, and patient information and education.
1. Educational activities, often with a plea for low cost or nil cost materials:
ASN is doing a great job with the educational resources and i hope you keep up the great work. getting input of fresh graduates in practice would provide insight as well.
Training on different aspects on nephrology- like coding, Medical directorship role and responsibilities. Continuing to provide online modules - if possible in video format for CME. Ongoing CME. Perhaps pod-casts/educational courses that could be taken online for CME. Similar to the Board Review Course but with modules and not just content experts but actual medical educators providing the content to ensure it’s educational.
Including KSAP in membership fees. :)
2. Guidelines:
Provide guidelines in heretofore ambiguous areas
Come up with frequent and simple patient/ office-based guidelines
Continued CME as above; endorsement/summarizing of clinical practice guidelines
Regular updates on recommendations/guidelines. Not being in an academic environment can be challenging to get the most up to date information and journals are not very focused on guidelines issues.
3. Improved quality measures:
Please lobby for more scientifically developed standards of quality assessment. Targets not set in strong scientific foundations hurt doctors and patients alike. Quality measures which have known interventions should be selected, otherwise there is a danger of forcing providers to cherry pick their patients.
Lobbying to include patient-centered measures in metrics that determine reimbursement, as a perfect phosphorus or putting in an AVF is not the right metric of the quality of my care in a physically declining 80 year old patient who still wants to do dialysis.
Use ASN leadership to use their legislative and lobbying efforts to better assess outcomes and reward quality of care than to just correct numbers!
4. Professional empowerment:
Increase physician oversight in the for profit dialysis unit. Specifically, physician who do not have a stake in the profits.
Fighting to get rid of the many nonsensical CMS regulations that make it much harder for me to provide the right care to the right patient.
ASN should adopt a statement on work life balance and workaholism. This is our achilles heel and I worry it impacts recruiting.
5. Patient information and education:
Provide ‘information for patients’ portals or handouts. Might help keep our patients informed and save time for providers.
Work directly with patients to help them understand importance of adherence with therapy. Advocacy to government regarding issues with non-adherent patients and the fact we are obligated to take care of them when they don’t do their part and yet it affects our reimbursement
Create standardized handouts for nephrology handouts that are free to physicians and can be given to patients. Advocate for increased payments for Medicare patients.
More patient educational material to understand CKD and final stages in understanding different modalities