The US Nephrology Workforce: Developments and Trends
First GWU Analysis of Nephrology Workforce Trends
Edward Salsberg, MPA
George Washington University School of Nursing
Leah Masselink, PhD
Xiaoli Wu, MS
George Washington University Milken Institute School of Public Health
Executive Summary
For many years the nephrology community has been concerned with three important workforce questions:
Will the United States have an adequate supply of nephrologists to assure access to needed care?
Will nephrology be able to continue to attract highly qualified applicants?
Will nephrology continue to produce investigators, particularly physician-scientists?
A number of recent developments, including the steady growth in fellowship positions, a 12-year decline in US medical school graduates (USMGs) selecting nephrology, and changing organization and reimbursement for nephrology services, have increased interest in these questions and the urgency of trying to answer them.
In 2014, the American Society of Nephrology (ASN) asked researchers at George Washington University (GWU) to review recent trends and developments in order to help the specialty answer these questions and to identify options for matching future supply and distribution with future needs with the ultimate goal of assuring access to highquality kidney care for all Americans. This report provides an overview of the nephrology workforce and factors influencing supply, demand, and use. Additional reports are planned for the next several years.
Based on the review of the key sources of data, a survey of nephrology fellows, and a literature review (Appendix), our research identified a number of important developments and trends impacting on the nephrology workforce:
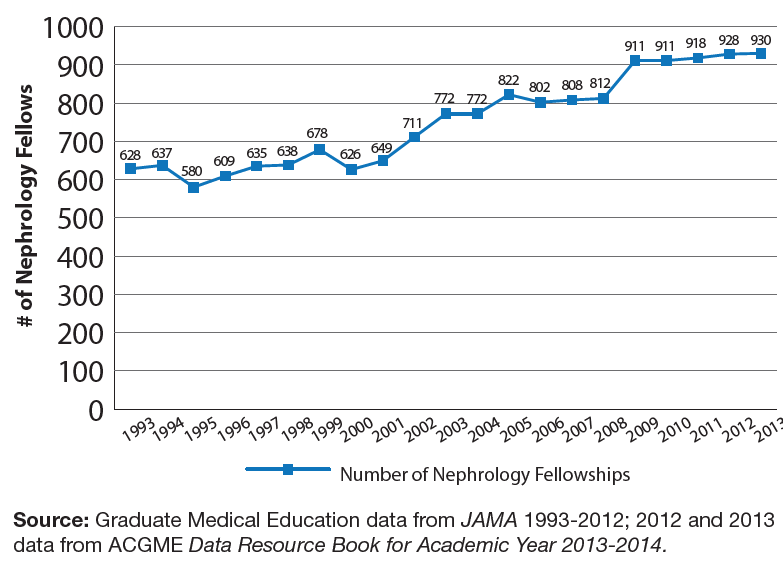
The number of fellowship positions has increased over the past several decades; this will lead to substantial future increases in supply. According to the Accreditation Council for Graduate Medical Education (ACGME) there were 473 1st-year fellows and 457 2nd-year fellows in the 2013–2014 academic year (AY)(ACGME 2014). The 930 fellows-in-training represent a 49% increase from the 626 in 2000. This will lead to a growing supply of nephrologists for many years to come.
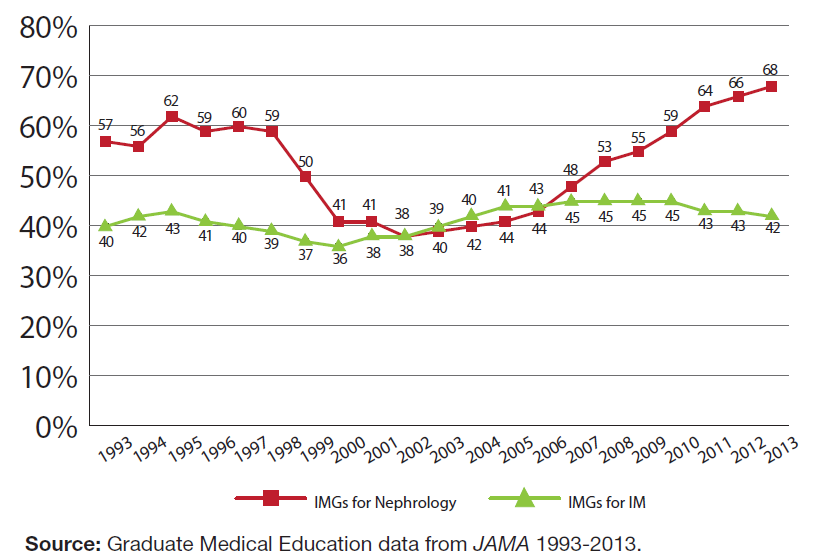
The percentage and number of USMGs selecting nephrology has been decreasing. The percentage of USMGs entering the specialty is lower now than it has been for decades despite an increase in US medical and osteopathic graduates. According to the ACGME, 68% of nephrology fellows in AY 2013–2014 were international medical school graduates (IMGs) compared to <40% a decade earlier. Between 2002 and 2006 nephrology recruited a higher percent of USMGs than general internal medicine (IM), but since 2006 the proportion of USMGs in IM has been increasing at the same time their proportion has been decreasing in nephrology.
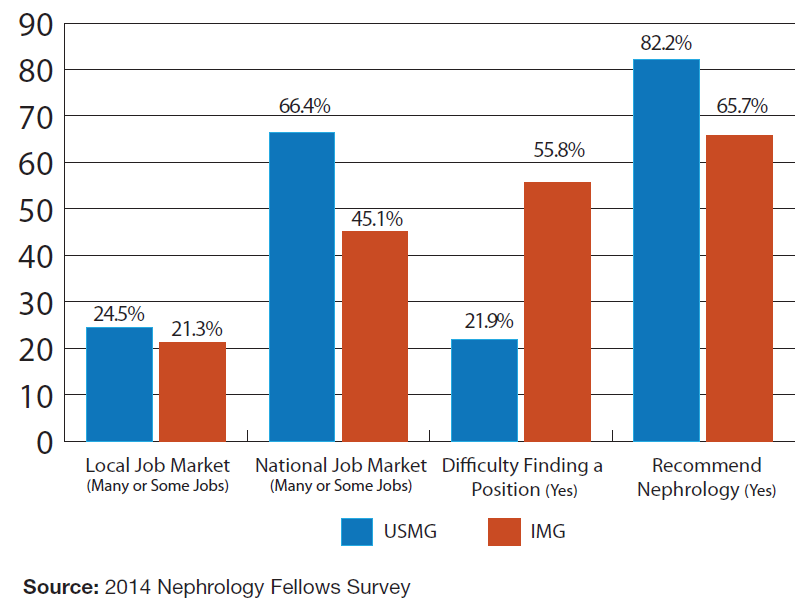
The 2014 nephrology fellows survey conducted for this study indicates the current job market for new nephrologists is limited, especially for IMGs. As noted later in this report, the job market appears tight, especially for IMGs, many of whom must practice in federally designated underserved areas in order to obtain a visa allowing them to stay in the United States. More than 56% of IMGs with at least 2 years of training reported difficulties finding a satisfactory position compared to only 22% of USMGs. The job market may be particularly tight near training sites, as fellows have a more positive impression of the national job market than the local job market. Despite the tight job market, there appear to be jobs available if nephrologists are willing to relocate to less-attractive areas. On a positive note, 83% of USMGs indicated they would recommend nephrology to medical students and residents.
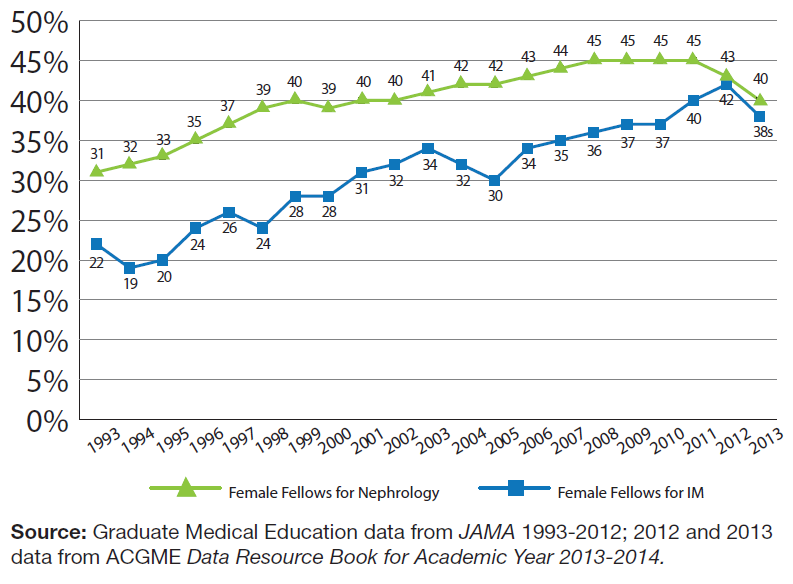
Nephrology appears to be recruiting a reasonable share of women and osteopaths to the specialty. Historically, the percentage of women in nephrology has been lower than in general IM residency programs. However, as of 2012, the percentage of female nephrology fellows was very similar to IM. Similarly, the percentage of osteopathic graduates selecting nephrology was consistent with IM. Given that the number of female medical school graduates is growing, this is an encouraging trend.
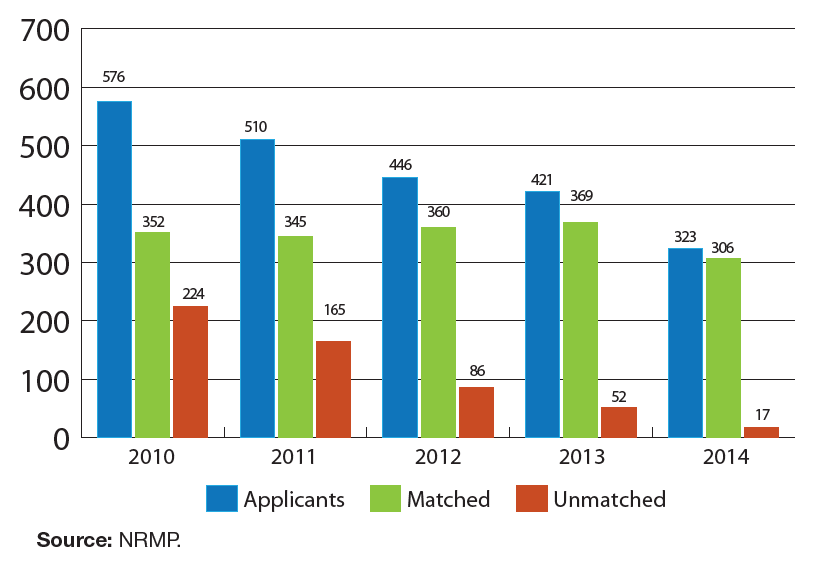
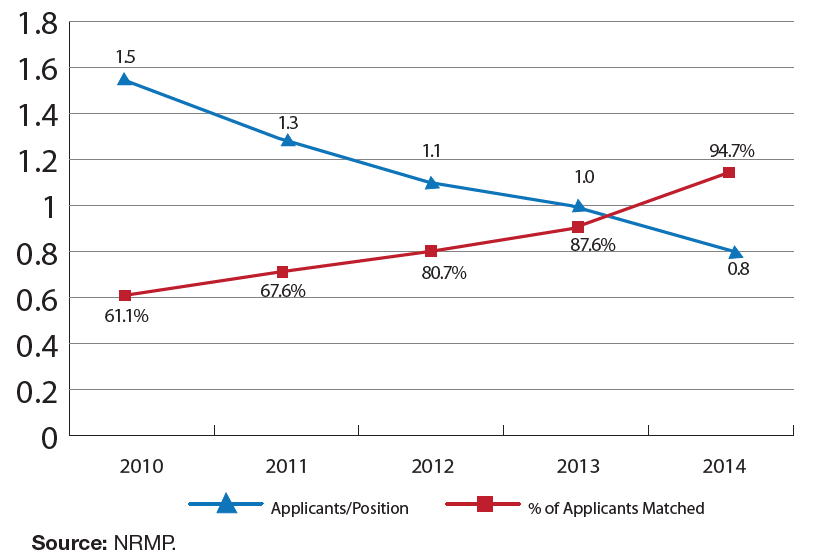
The number of applicants to nephrology through the National Residency Match Program (NRMP) is decreasing; many programs did not fill through the NRMP Match. The number of total applicants to nephrology through the NRMP Specialties Matching Service has decreased steadily over the past 5 years. In 2010, there were 1.5 applicants for available slots, but in 2014 only 0.8 applicants for each fellowship position (NRMP 2014).
While the cause of the drop in interest by USMGs is probably multifactorial, a soft job market appears to be playing an important role. As noted above, the nephrology fellows survey results suggest limited job opportunities, which is consistent with studies included in the literature review (Appendix). It is also consistent with the results of University at Albany Center for Health Workforce Studies (CHWS) NY State survey of residents and fellows completing training in the state, which found that the demand for nephrology fellows completing training in AY 2002–2004 was relatively high, but by AY 2012 had fallen to 22nd of the 25 specialties reported (Center for Health Workforce Studies 2010, 2013).
The demand for care related to kidney disease and injury is increasing. All indications—including an aging population, increased life expectancy, and an increasing incidence and prevalence of kidney disease and injury—indicate the need for nephrology services is likely to continue increasing.
The patient care delivery system for kidney disease and injury is evolving with pressure to constrain growth in expenditures. The delivery system transformation, spurred on in part by the efforts to constrain the growth in Medicare costs, is likely to affect the use and demand for nephrologists. The significant and growing role of for-profit organizations, new Medicare policies, as well as the increasing use of other health professionals in the kidney care team are contributing to the transformation of care.
Introduction
On the one hand, the increasing incidence and prevalence rates of chronic kidney disease (CKD) and end stage renal disease (ESRD), an aging population, Medicare coverage for ESRD care, and the implementation of the Affordable Care Act all suggest that the need and demand for services related to diagnosing and treating kidney disease and injury will increase in the future.
On the other hand, payment reforms and organizational changes designed to slow the growth of health expenditures and the increased supply of nephrologists may dampen demand for the specialty. The growing emphasis on team-based care and other health professionals (besides physicians) in chronic disease care raises the question of whether the increased need for kidney disease care necessarily translates into increased need or demand for nephrologists.
Furthermore, the recent decrease in the number and percentage of USMGs selecting nephrology fellowship training has heightened concern about the ability of the specialty to attract the most highly qualified physicians. Although declining USMG interest in nephrology in and of itself is a concern for the specialty, it also raises a question as to whether this reflects decreased job opportunities in nephrology.
Medicare spends billions of dollars treating kidney disease and injury and these costs have increased more rapidly than overall Medicare expenditures over time (>500% increase since 1991 vs. 369% overall). The program spent >$45 billion on CKD care and $34 billion on ESRD care out of a total $549 billion in 2011 (US Renal Data System 2013). The high cost of kidney disease care is likely to lead to continued scrutiny by policy makers and a focus on ways to control the costs of kidney care, including ways of utilizing the entire health professional workforce efficiently and effectively.
The research team at GWU reviewed existing data sources and studies and conducted a survey of nephrology fellows. The work of GWU builds on numerous prior studies in this area, many of which were supported by ASN and/or conducted by the society’s members. This report is the first of several over the next few years that will help ASN and the nephrology community better understand the kidney care needs for the United States and to assure a vibrant workforce to meet those needs.
This study relied on a number of data sources including:
American Medical Association (AMA) Masterfile data on physicians listing nephrology as their primary or secondary specialty or who had trained in nephrology
ACGME data on nephrology fellows and training programs
Findings from the nephrology fellows survey conducted in summer 2014
Data from the NRMP Specialties Matching Service
Results from the Resident Exit Survey conducted by the CHWS
Data on the incidence of CKD and ESRD from the 2013 US Renal Data System Atlas
A comprehensive review of the literature on the nephrology workforce
Profile of the Nephrologist Workforce and Nephrology Fellows
The Demographics and Distribution of the Current Nephrology Workforce
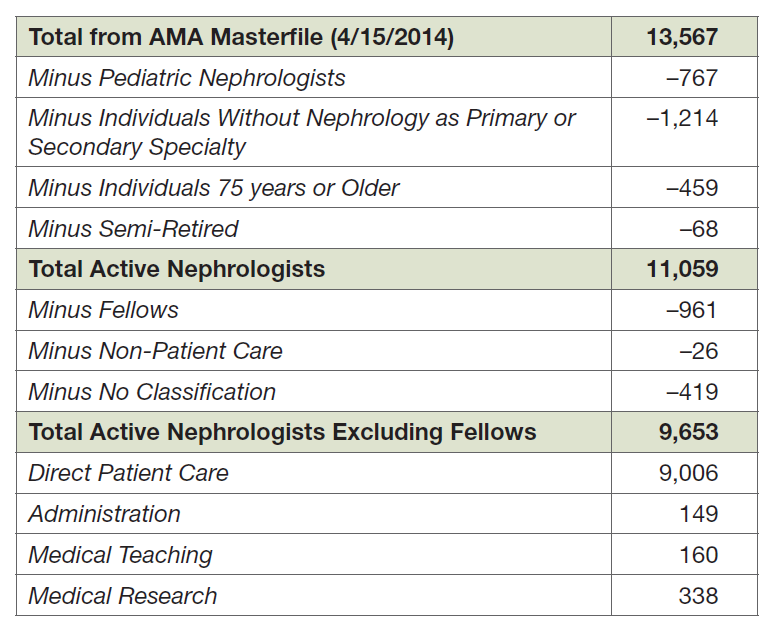
The AMA Masterfile of physicians includes extensive data on the physician workforce in the United States, including demographics, education, training, and current practice. As of April 15, 2014, there were 13,567 physicians in the Masterfile with some indication of training and/or practicing nephrology. After a variety of adjustments, it was determined that there were 9,653 physicians actively practicing in adult nephrology >20 hours per week. Of these, 9,006 were primarily engaged in direct patient care and 647 primarily engaged in teaching, research and/or administration (Exhibit 1). These 9,653 physicians were included in our analysis.
Age
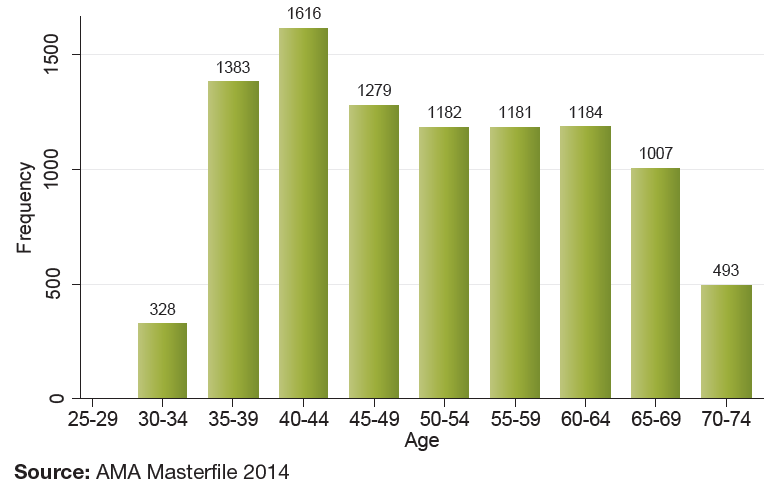
As indicated in Exhibit 2, the largest 5-year age cohort for nephrologists is the 40–44 years age group followed by the 35–39 years. Although this reflects an increased number of fellows entering the specialty, the high number of active nephrologists >60 years (2,684 [28%]) also indicates that there will be a fair amount of turnover in the specialty over the next several years.
Sex
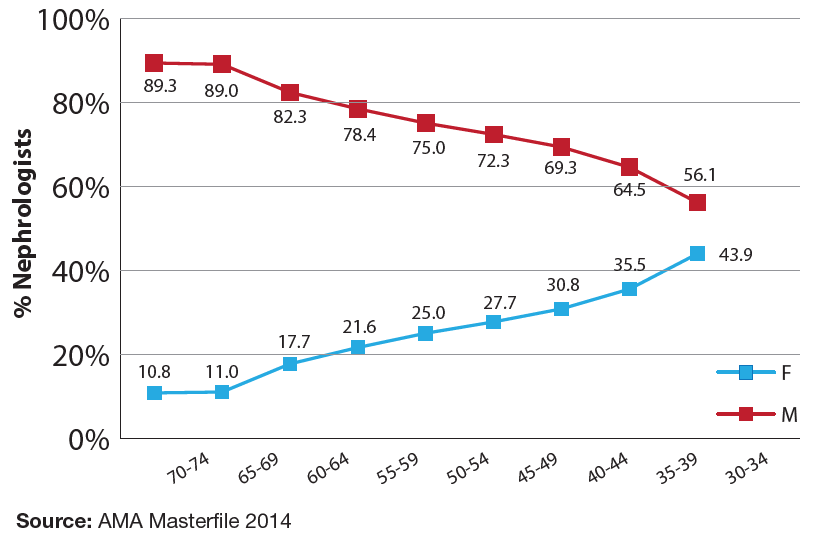
Exhibit 3 shows the sex distribution of nephrologists across 5-year age categories. (Note that for this figure, the older age categories are shown on the left and the younger categories are shown on the right to show the progression over time.) The percentage of women in nephrology has steadily increased reflecting both the increase of women in medicine and the increase of those selecting the specialty.
Race
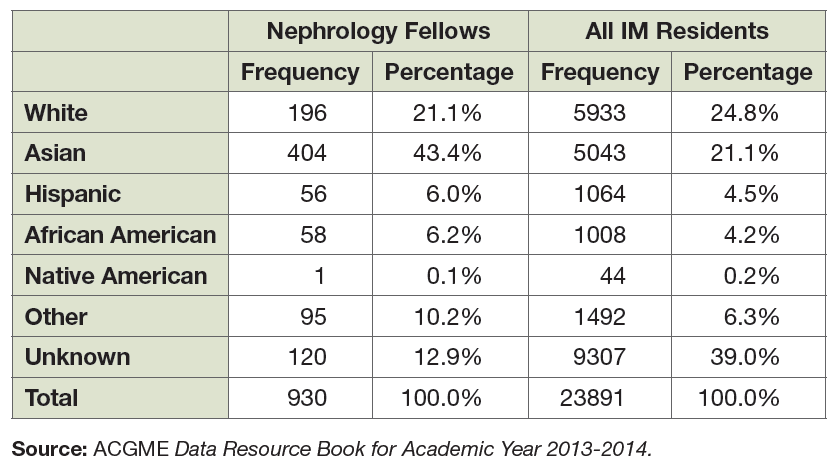
Good data on the race and ethnicity of practicing nephrologists is not readily available. However, ACGME data on physicians-in-training provides a picture of the incoming workforce. Exhibit 4 compares the composition of the AY 2013–2014 nephrology fellows and IM resident populations by race. Nephrology has a relatively high representation of Asians (43.4% vs. 21.1% of IM residents). It also has slightly higher percentages of African American (6.2% vs. 4.2% of IM residents) and Hispanic fellows (6.0% vs. 4.5% of IM residents). However, a far higher percentage of IM residents did not report their race/ethnicity (39% in IM vs. 12.9% in nephrology) indicating caution in drawing conclusions in direct comparisons.
Medical Education Type and Location
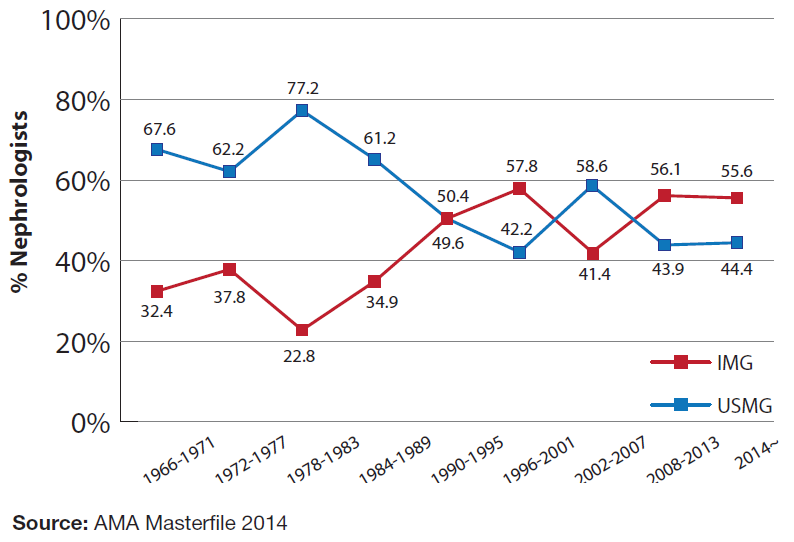
Exhibit 5 presents the percentages of practicing nephrologists that are USMGs and IMGs based on when they completed their nephrology training. Prior to 1990 new nephrologists were far more likely to be US medical and osteopathic graduates, but this changed with the 1990–1995 cohort and has varied since then. As discussed later, the percentage of new nephrologists who are USMGs has continued to drop further in recent years.
Geographic Distribution
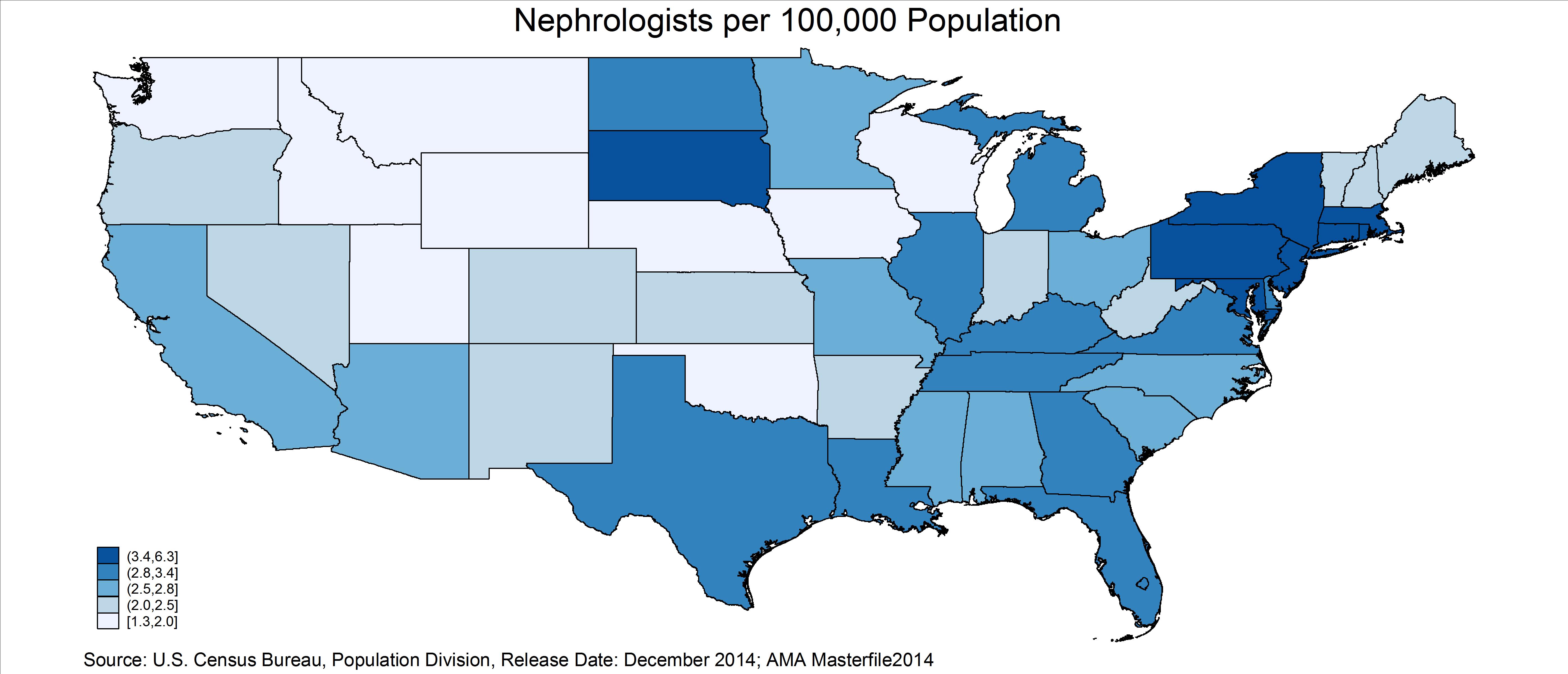
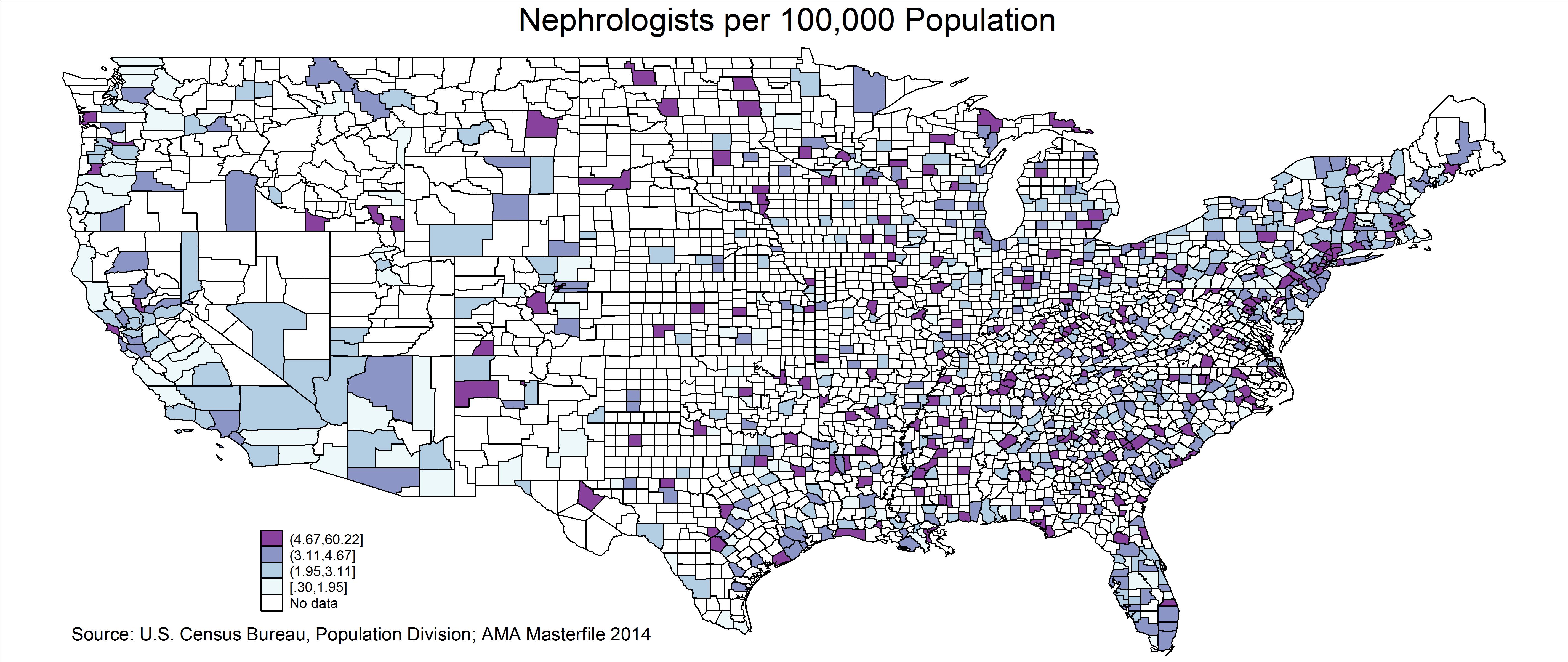
Exhibits 6 and 7 show the distribution of nephrologists per 100,000 population in the contiguous 48 US states and by county. The darkest color indicates the most nephrologists/population (highest quintile) and the lightest color indicates the fewest nephrologists/population (lowest quintile). This varies substantially by state—from a high of 6.3 in the District of Columbia to a low of 1.3 in Iowa. This variation will need to be reviewed closely. It is possible for a specialty to have an adequate national supply in total but still have major shortages within many communities across the country.
The Nephrology Pipeline: Fellows and Training Programs
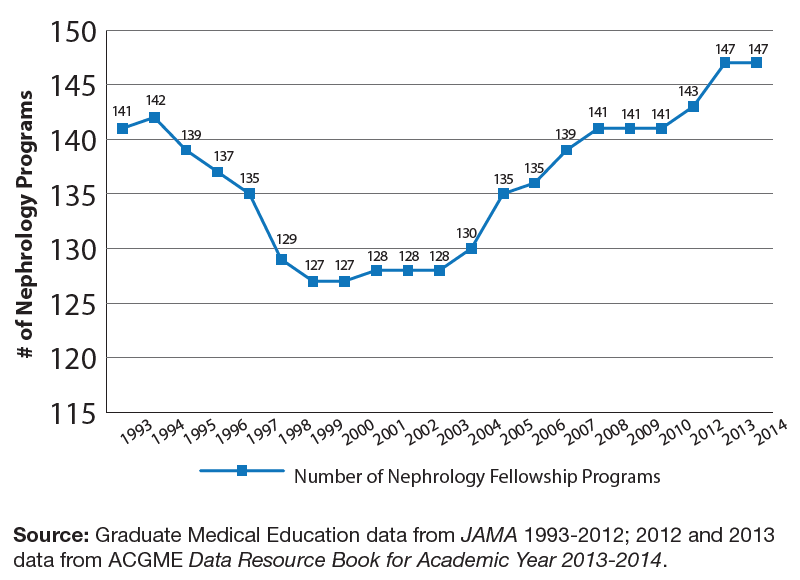
The current cadre of physicians training in nephrology and recent trends provide a picture of the future nephrology workforce. ACGME data on fellows and accredited nephrology training programs shows the overall number of nephrology fellowship programs shrank from 141 in 1993 to 127 in 2000 before increasing to 147 in 2012. The growth between 2000 and 2012 may reflect the prevailing belief that more nephrologists were needed to meet the expected increase in patients with CKD and ESRD.
Over the same period of time, the number of fellowship positions has exhibited a different pattern than fellowship programs, growing steadily from 628 in 1993 to 930 in 2013—a 49% increase (Exhibit 9). The average number of fellows per program has also grown over time from 4.45 fellows/program in 1993 to 6.33 fellows/program in 2013.
Another question of considerable interest to the nephrology community is the location and type of education of nephrologists (US-educated MD [USMD] vs. US-educated DO vs. non-Canadian IMG vs. Canadian).
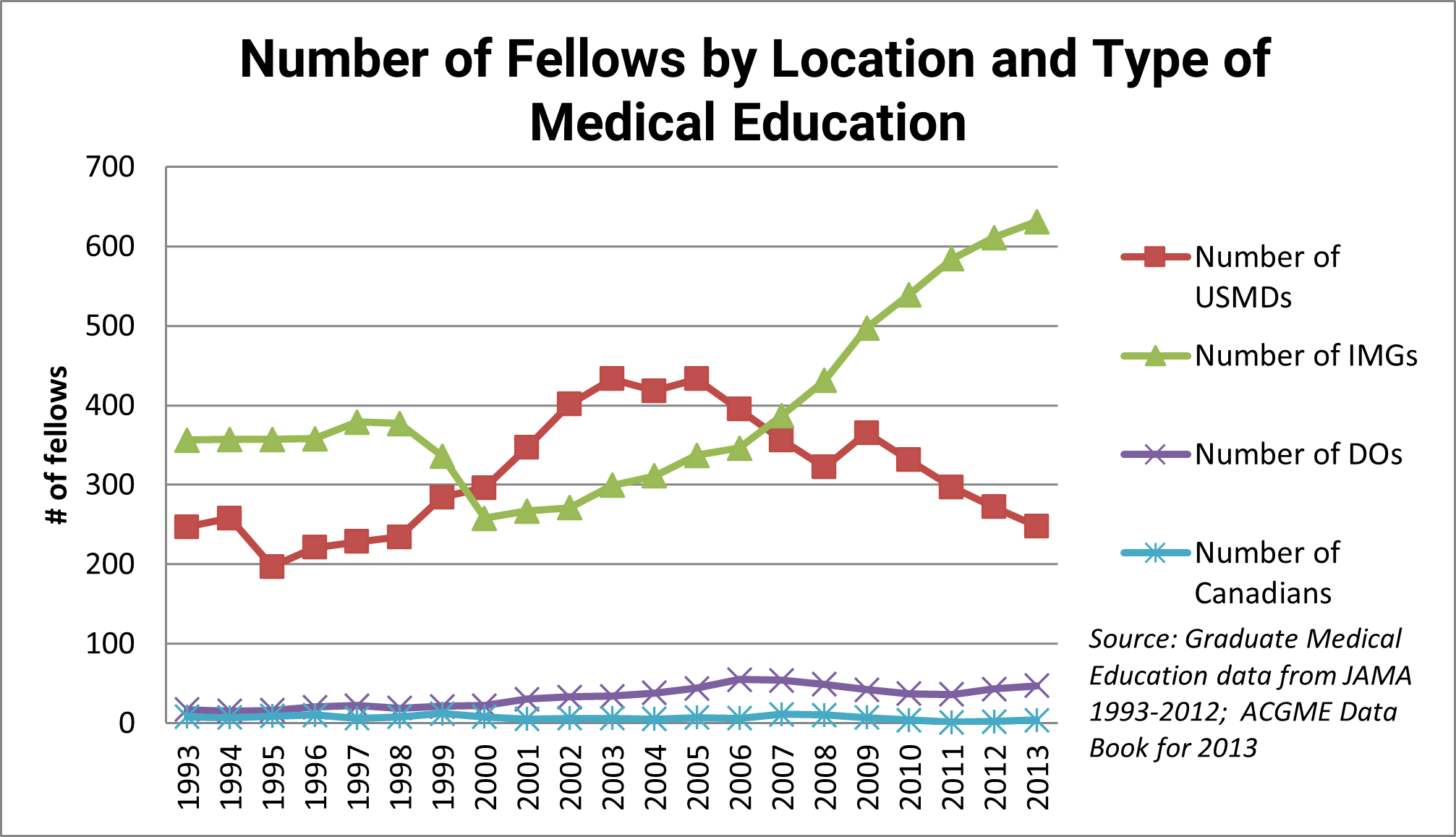
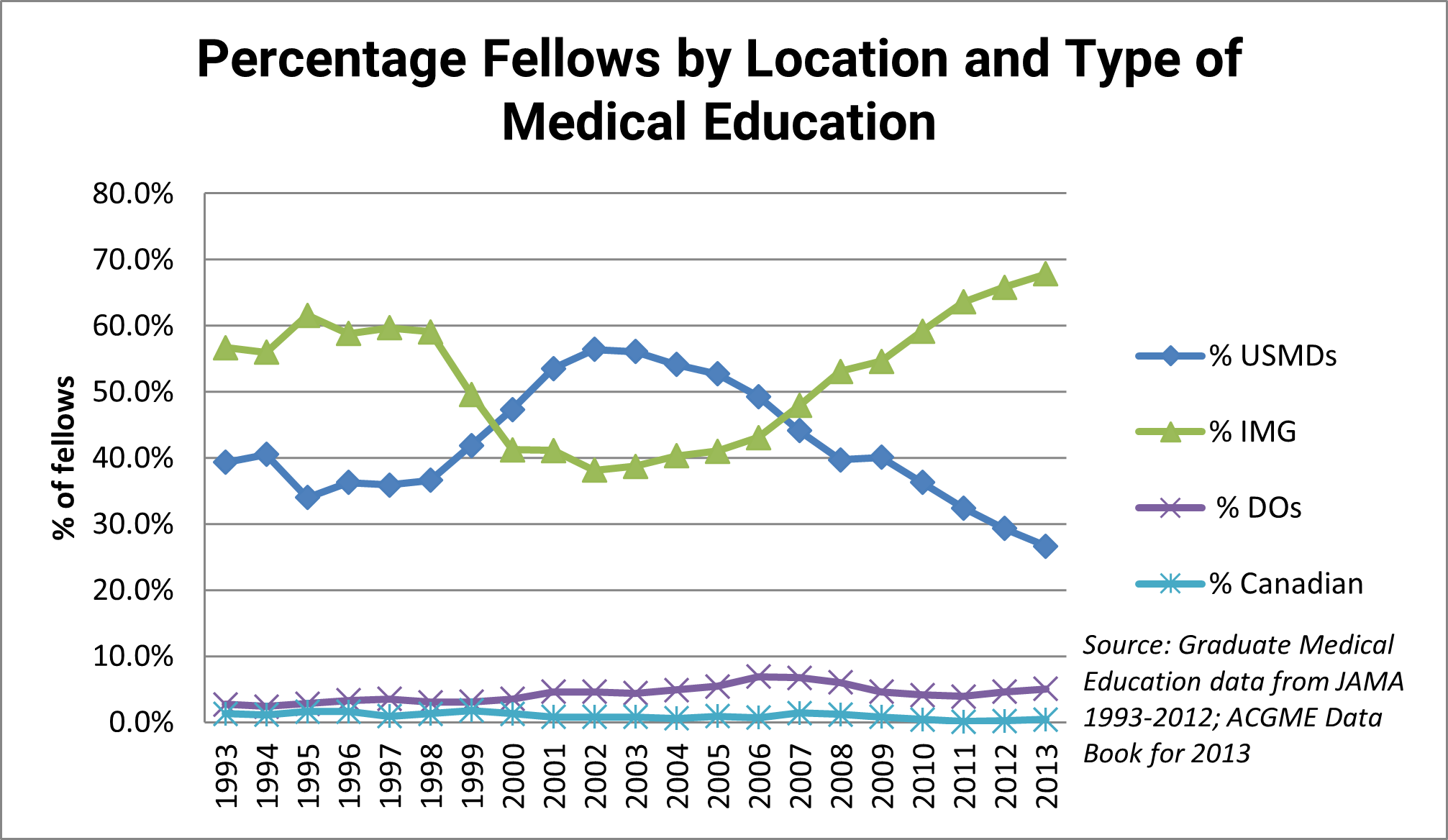
It is apparent that the location of medical education of the majority of nephrology fellows has changed over time: IMGs were most prominent in the 1990s, while USMGs were the largest group in the early 2000s. Since 2007, the number and proportion of IMGs has grown to unprecedented levels. In 2013, more than two-thirds of nephrology fellows were IMGs. Exhibit 12 compares the percentage of IMG nephrology fellows with the percentage of IMG IM residents over time. While the proportions of IMGs in each group briefly tracked each other in the early to mid-2000s, the figure shows that IMGs are overrepresented in nephrology fellowship training programs relative to their representation in IM residency programs. The disparity is particularly pronounced in the 1990s and since 2008, and the 23% disparity in 2013 (66% vs. 43%) is the largest recorded in the past 20 years.
Finally, Exhibit 13 addresses another key question of interest to the nephrology community: the degree to which female physicians are represented in nephrology fellowship programs over time. The percentage of females in nephrology fellowship programs has nearly doubled between 1993 and 2012, from 22% to 42%. While there was a substantial difference with the percentage in general IM in past years, with the proportion of women in IM being >50% higher than nephrology in some years, the gap is now nearly closed.
Results from the NRMP Specialties Matching Service
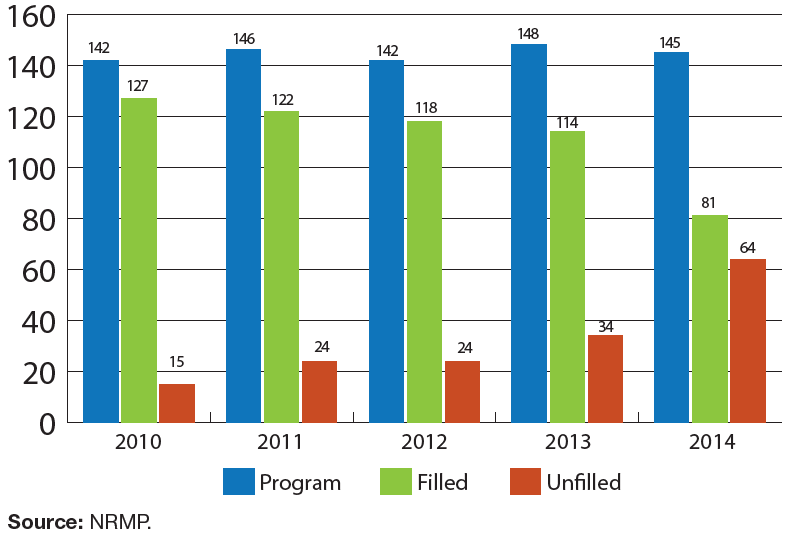
Data from the NRMP for AY 2014–2015 also provides information on the nephrology pipeline including the attractiveness of the specialty. Exhibit 14 shows the number of nephrology fellowship programs (overall, filled and unfilled/partially filled) over time from 2010 through 2014. While the number of nephrology fellowship programs counted by NRMP has remained nearly steady between 2010 and 2014, the figure shows a sharp increase in the number of unfilled programs, from 15 unfilled programs (10.6% of 142) in 2010 to 64 unfilled programs (44.1% of 145) in 2014.
The same trend is demonstrated in unfilled nephrology fellowship positions with the proportion of unfilled positions increasing from 5.9% in 2010 (22 unfilled positions of 374) to 24.1% in 2014 (97 unfilled positions of 403). The number of unfilled fellowship program positions doubled in just one year—from 47 in 2013 to 97 in 2014.
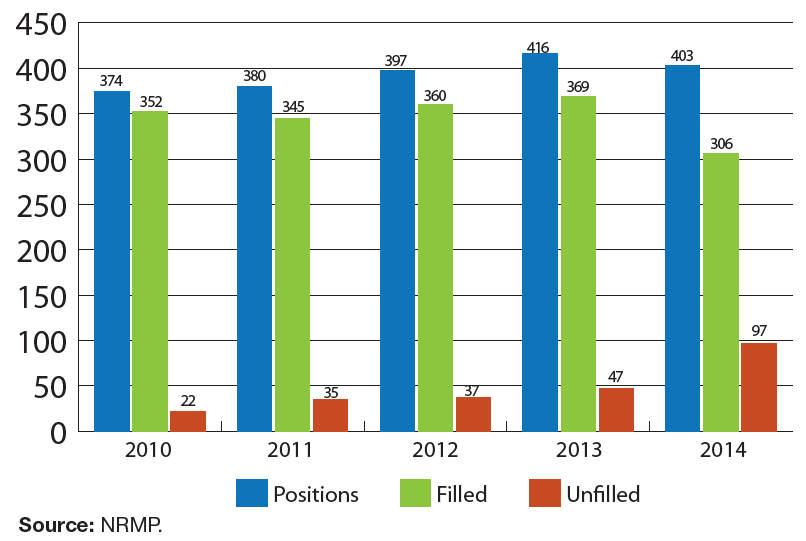
This increase in unfilled positions corresponded to a decline in the number of fellowship applicants—from 576 in 2010 to 323 in 2014. Only 323 individuals applied for 403 nephrology fellowship positions in 2014, a ratio of 0.8 applicants per position. Nephrology fellowship programs have become significantly less selective since 2010, when only 61.1% of applicants matched into programs. In 2014, the figure was 94.7%, with only 17 applicants failing to match, leaving 97 positions unfilled.
Findings from the Nephrology Fellows Survey: Job Market Experiences
We conducted an online survey to obtain direct insights from current nephrology fellows and trainees on recent developments affecting new nephrologists, including training backgrounds, educational debt, and factors influencing job opportunities and choices. The survey tool—adapted from the University at Albany Center for Health Workforce Studies (CHWS) annual NY State Resident Exit Survey—was distributed to the 1530 ASN nephrology fellow/trainee members (to whom ASN offers free membership) in June and July 2014. Of these, 534 fellows/trainees responded and provided informed consent (34.9% response rate).
The full findings from the nephrology fellows survey will be detailed in a future report, but the following presents findings related to nephrology fellows’ job market experiences to add insight to the data from other sources presented above.
We tested whether nephrology fellows’ reported job market experiences were significantly different across demographic categories using chi-square tests. We tested for differences in responses across three key categories:
Male vs. female fellows
USMGs vs. IMGs
Census regions (Northeast vs. Midwest vs. South vs. West)
We present the overall findings and accompanying chi-square test results for each of the job market experience questions. Probability values <0.05 were considered statistically significant. For this analysis we included respondents who had completed or were completing at least their 2nd year of training in 2014 and were not a pediatric nephrology fellow (300 respondents)—in other words, fellows who have at least the possibility of searching for a job in adult nephrology. Note that sample sizes for different sets of questions differ slightly because of missing data and/or skip patterns in the survey instrument.
Job Search Experiences
Among the 187 nephrology fellows who indicated they had already completed their basic nephrology training, we found the following with respect to their job search experiences.
Difficulty Finding a Satisfactory Position
Fellows’ experiences finding a satisfactory position were mixed: 43% reported they had difficulty finding a satisfactory practice position and 33% reported no difficulty. (The remaining 23% had not looked for a position yet.)
We found a statistically significant difference between male and female fellows’ reports of difficulty finding a position (p=0.03): more female fellows (32%) than male fellows (16%) had not looked for a position yet, and male fellows were more likely than female fellows to report difficulty finding a satisfactory position (49% vs. 35%).
We also found a statistically significant difference between IMG and USMG fellows’ reports of difficulty finding a position (p<0.01): USMGs were more likely not to have looked for a position than IMGs (33% vs. 18%), and IMGs were more likely to report difficulties in finding a satisfactory position (56% vs. 22%).
We found no statistically significant difference in reports of difficulty finding a position across census regions (p=0.12).
Reasons for Difficulty
Among the 76 fellows who reported difficulty finding a satisfactory position, the most frequently cited reasons were lack of jobs/practice opportunities in desired locations (32%) and lack of jobs/practice opportunities that meet visa status requirements (28%).
We found a statistically significant difference in reasons for difficulty finding a position between IMG and USMG fellows (p=0.04): IMGs were more likely than USMGs to note lack of jobs that meet visa requirements (33% vs. 0%), and USMGs were more likely than IMGs to note lack of jobs in desired locations (54% vs. 27%).
We found no statistically significant difference in the reasons for difficulty finding a position between male and female fellows (p=0.58) or across census regions (p=0.28).
Changing Plans due to Limited Practice Opportunities
A substantial proportion of nephrology fellows (43%) who had looked for jobs reported that they had changed their plans because of limited practice opportunities. We found no statistically significant differences in the degree to which fellows changed their plans between male and female fellows (p=0.44), IMGs and USMGs (p=0.19), or across census regions (p=0.39).
Number of Job Applications
Nephrology fellows’ reports of the numbers of job applications they had completed varied widely—60% applied for between 1 and 5 jobs, approximately 30% had applied for at least 6 jobs, and 10% had not applied for any jobs.
We found a statistically significant difference in the number of job applications between IMGs and USMG fellows (p=0.02): IMGs were more likely than USMGs to apply for >10 jobs (19% vs. 2%), although patterns across other ranges were less consistent.
We found no statistically significant differences in the number of job applications between male and female fellows (p=0.48) or across census regions (p=0.36).
Number of Job Offers
The majority of nephrology fellows (71%) reported receiving between 1 and 3 job offers, and about 12% of fellows reported receiving no job offers.
We found a statistically significant difference in the number of job offers across census regions (p=0.05). Fellows in the West census region were more likely than fellows from other regions to have no job offers (23% vs. 8% of fellows across the other regions). We found no statistically significant differences in the number of job offers between male and female fellows (p=0.16) or IMG and USMG fellows (p=0.48).
Job Offer Characteristics
Among 112 nephrology fellows who had already accepted job offers, we found the following with respect to their salary and compensation expectations.
Base Salary/Income
Fellows’ expected salaries ranged from <$100,000 to >$300,000. Among the fellows who had accepted job offers, >60% anticipated annual base salaries between $150,000 and $200,000, and another 11% expected salaries <$100,000.
We found no significant differences in expected salaries between male and female fellows (p=0.68), between IMGs and USMGs (p=0.18), or across census regions (p=0.40).
Anticipated Additional Incentive Income
Nearly half (48%) of fellows who had accepted job offers did not anticipate receiving any additional incentive income. Those expecting to receive incentive income reported a range of expected incentives from <$5000 to >$60,000. We found no significant differences in expected salaries between male and female fellows (p=0.61), between IMGs and USMGs (p=0.62), or across census regions (p=0.77).
Satisfaction with Salary/Compensation
The majority of fellows who had accepted job offers indicated that they were satisfied with their salary and compensation. Approximately 26% reported being “very satisfied”, and 45% indicated that they were “somewhat satisfied” with their salary and compensation.
We found a statistically significant difference between male and female fellows’ satisfaction (p=0.01): female fellows (86%) were more likely than male fellows (62%) to indicate that they were “very satisfied” or “satisfied” with their salary and compensation.
We found no statistically significant difference in satisfaction with salary and compensation between IMGs and USMGs (p=0.72) or across census regions (p=0.41).
Job Market Perceptions
Finally, we found the following among 280 fellows in adult nephrology who were in their second year of training or beyond.
Local Job Market Perceptions
Nephrology fellows’ perceptions of local nephrology job opportunities were dim: 71% reported that there were no, very few, or few nephrology practice opportunities within 50 miles of their training sites. This may reflect the reality around many medical schools and teaching hospitals where former fellows have settled.
We found a statistically significant difference in IMG and USMG fellows’ assessments of local nephrology practice opportunities (p<0.01): IMGs were more likely than USMGs to report no job opportunities in their local area (16% vs. 4%), although the overall proportions reporting no-very few or few jobs were similar (70% of IMGs and 72% of USMGs). USMGs were slightly more likely than IMGs to report that there were some or many job opportunities available (25% vs. 21%).
We found no statistically significant differences in local job market perceptions between male and female fellows (p=0.45) and across census regions (p=0.51).
National Job Market Perceptions
Nephrology fellows perceived national nephrology job opportunities much more positively than local opportunities—53% reported there were some or many nephrology practice opportunities nationally.
We also found a statistically significant difference in IMG and USMG fellows’ assessments of national nephrology practice opportunities (p<0.01): IMGs were more likely than USMGs to report that there were no, very few or few job opportunities available (51% vs. 25%), and USMGs were more likely than IMGs to report some or many job opportunities nationally (66% vs. 45%).
We found no statistically significant differences in national job market perceptions between male and female fellows (p=0.12) and across census regions (p=0.38).
The findings from the nephrology fellows survey suggest IMG nephrology fellows’ job market experiences were significantly less positive than USMGs. Exhibit 18 shows striking differences between USMGs’ and IMGs’ responses to several of the job market experience questions. IMGs were significantly less optimistic than USMGs about their local or national job markets, and they were significantly more likely to report difficulty finding an acceptable position (possibly because of a lack of positions available to J-1 visa applicants). IMGs were also nearly twice as likely as USMGs to report that they did not recommend the specialty to others.
Would Fellows Recommend Nephrology?
Despite their somewhat pessimistic impressions of local nephrology job opportunities, a vast majority of fellows (72%) indicated that they would recommend the specialty to medical students or IM residents.
We found a statistically significant difference in IMG and USMG fellows’ likelihood of recommending nephrology to others (p<0.01): while 82% of USMG fellows indicated that they would recommend the specialty, only 65% of IMG fellows indicated the same.
We found no statistically significant differences in the likelihood of recommending nephrology between male and female fellows (p=0.44) or across census regions (p=0.54).
Among the 35% of IMG fellows who did not recommend nephrology, several noted the lack of jobs for J-1 visa applicants as a key reason why they would not recommend the specialty:
No jobs for J-1 visa applicants despite so many fellows being on J-1 currently. Every job posting that I come across mentions that it is not a J-1 opportunity. What is the point of having so many J-1 fellowship training spots if no one is willing to offer jobs?—IMG 2nd year
Other concerns mentioned by both IMGs and USMGs who would not recommend nephrology included a lack of desirable job opportunities and the difficulty of maintaining healthy work-life balance while working as a nephrologist:
Very difficult to find a practice in a desired location and desired practice setting. Tried more than 10 months, but now accepted a position where spouse does not have a job, but I had to take the job.—IMG 2nd year
There are lots of opportunities in internal medicine which may provide equal amount of satisfaction, salary and work life balance without the need for additional fellowship training.—USMG 2nd year
Changes in the Provision & Utilization of Nephrology Services
The prevalence of kidney diseases has increased significantly in the past 20 years. The number of CKD patients reached 2.3 million estimated point prevalent patients in 2011 (USRDS 2013). The number of prevalent ESRD patients has increased threefold in the past 20 years, from approximately 205,000 point prevalent patients in 1991 to approximately 615,000 point prevalent patients in 2011 (5). Among these, approximately 400,000 patients were on dialysis as of 2009, with the numbers growing by 3% to 4% each year (Collins 2012).
Kidney conditions are also a significant cause for hospitalizations of Medicare patients. The hospitalization rate for acute kidney injury increased 346%, more than for any other diagnosis between 1997 and 2011 (Pfunter et al. 2013), and kidney failure is also one of the top 10 conditions associated with hospital readmissions of Medicare patients (Hines et al. 2011). However, it appears that the high rate of kidney disease–related hospital admissions does not necessarily lead to increased demand for nephrologists in hospitals. An industry publication explains:
“The opportunity to work as an employee of the hospital is not one that is usually afforded to young nephrologists, especially not in competitive markets. The reasons are numerous, but the key one is a result of the specialty itself. Nephrologists admit patients that tend to be the sickest of the sick and extremely costly to the hospitals, with higher than average readmission rates (Medicare has implemented new rules that penalize hospitals for readmissions). Hospitals do not benefit by employing nephrologists. The main reason for employing physicians is to increase referrals and fill beds—-in most cases, they would be getting those patients regardless of whether they were referred by the nephrologist or not.” (Osinski 2013)
Osinski estimates that 70% of nephrologists join either multispecialty or single-specialty private practices after completing their training. He suggests that multispecialty groups are often preferred because they bring built-in referral networks and “strength in numbers” negotiating with managed care organizations, ACOs, among others. As the specialty moves toward a focus on outpatient care (Jhaveri et al. 2013), nephrology practices are consolidating and increasing their revenue. A 2011 benchmarking survey by the Renal Physicians Association showed fewer practices with 4 to 7 nephrologists and more practices with 11 or more nephrologists since 2009, as well as a 27% increase in relative value units per nephrologist since 2009 (NN&I, 20 Mar 2013).
In addition to private practice, Osinski suggests that dialysis providers may become more appealing employers for nephrologists:
“Some of the dialysis companies are employing physicians through utilization of salaries and income guarantees, mixed with medical directorships. Early indications are that fellows appear to be open to the idea and the security it provides, similar in many ways to the security primary care physician groups have received by selling themselves off to hospitals. The idea of being financially supported by a dialysis provider is appealing and it is expected that (like in primary care) this trend will continue over the coming years.”
The effects of this new configuration on the nephrology workforce are still unknown. Most dialysis care is provided by for-profit providers, which one author has described as an “oligopoly” (2 large providers have 70% of US dialysis market share). While the consolidation of dialysis care facilitates data sharing and standardization of care, it can relegate nephrologists to “small cog in a big machine” status in the large bureaucracies (Himmelfarb et al. 2007). Changes in how Medicare pays for ESRD care have motivated key changes in the provision of care that could affect the future nephrology workforce. While there were previously very few nurse practitioners (NPs) or physician assistants (PAs) in nephrology, the number has increased since CMS began allowing 3 of 4 required dialysis visits to be conducted by NPs/PAs in 2004. NPs/PAs were first being used in dialysis clinics, but have since expanded to all aspects of nephrology care. NPs and PAs are especially well utilized in patient education, where their role expanded after the Medicare Improvements for Patients and Providers Act (MIPPA) authorized providers (including NPs and PAs) to bill Medicare for kidney disease education for CKD patients. NPs/PAs were the largest provider group providing kidney disease education between 2010 and 2012 (Davis and Zuber 2014). They are also involved in dialysis and transplantation follow-up care and research. NPs/PAs like the flexibility of making their own schedules for dialysis rounds as well as the challenge of working with complex patients (Davis and Zuber 2009, 2014).
For many years Medicare has paid for ESRD care using a “composite rate” that covers dialysis, drugs, and lab tests, although some tests/drugs are also billed separately. The bundled payment system was updated in 2011 to include dialysis procedures and labs (from the previous bundle) plus additional lab tests done by nephrologists, injections and oral medications. (Injections and many lab tests had previously been outside the bundle.) The payment rate is adjusted for acute conditions, new dialysis patients, and several comorbid conditions. Some have raised concerns about whether care would be sacrificed for higher profits (Himmelfarb et al. 2007). Early evidence suggests that the new bundled payment system has led to changes to dialysis care, most notably an increase in peritoneal dialysis utilization (Collins 2014).
Discussion
The issues of training an appropriate number of nephrologists for the need/demand for nephrology care and the attractiveness of the specialty to clinicians and physician-scientists are related. The recent increase in the number of fellowship positions at a time when Medicare, the major source of funding for nephrology care, has been taking steps to constrain rising costs of care appears to have led to a softening job market for new nephrologists. This in turn appears to be contributing to a decrease in applications to nephrology fellowship programs. This is consistent with findings from recent studies showing significant concern by residents and fellows about both job opportunities and compensation in nephrology (Shah et al. 2012).
While the belief that the United States will need more services for kidney-related conditions appears accurate, changes in the delivery system combined with and driven by changes in reimbursement policies may mean that increased service need may not translate into as much of an increase in the demand for nephrologists as previously expected. In fact, it is possible that the recent increase in nephrology fellowship positions has more than met the growing demand. This suggests a moderation in the number of fellowship positions may be warranted. However, it is important to look beyond today’s marketplace to assess whether the current level of production is appropriate for future needs; in other words, is the current soft job market temporary, reflecting uncertainties in a time of delivery transformation?
While there are a variety of steps that can be taken to try to make the specialty more attractive, the success of these efforts may depend on the marketplace. USMGs’ specialty choices are sensitive to job opportunities and compensation, so initiatives attempting to counter marketplace signals can be like swimming upstream. This is not to argue against efforts to attract more USMGs, but to suggest that the first step is to determine if the current production level is consistent with the future needs of the United States and the likely job market. An over-production of nephrologists would be detrimental to the specialty, physicians, and patients if quality were to drop.
These developments raise a number of questions the answers to which will impact on the supply, demand, and use of nephrologists. These key questions will be further explored by the GWU research team.
How is the evolving delivery system going to affect the use and demand for nephrologists? There are assumptions and guesses, but limited hard evidence. The delivery system for kidney illness and injury needs to be monitored and its impact on the workforce assessed on an on-going basis.
Does the apparent adequacy of the national supply mask serious maldistribution of the existing supply? Are there areas of the United States in need of additional nephrologists? As seen in Exhibits 6 and 7, there are significant variations in the number of nephrologists per capita across the nation. If there are areas of great need, what are the options for addressing maldistribution?
Is the soft job market temporary? Will demand exceed supply in a few years? While the supply seems adequate today as seen through the experience of new graduates, does this primarily reflect the current uncertainty in the market place?
Should ASN and the nephrology community be encouraging a decrease in the number of programs and fellows? The current number of 930 1st and 2nd year nephrology fellowship positions (accredited by ACGME) is higher than in the past. Nephrology has not done well in the specialty Match, and its performance has declined over time.
Are there specific nephrology subspecialty areas and geographic areas where the demand and job opportunities are different than for nephrology as a whole? Is grouping all nephrology together missing major variations within the specialty and by region?
What can be done to increase diversity of the specialty? Regardless of whether the national supply is adequate, given the high incidence of kidney disease and illness among African Americans and the low percentage of African American nephrologists, a workforce more reflective of the population to be served could improve access and quality of care.
What can be done to increase interest in the specialty? Despite the rise in nephrology positions and the recent increase in USMGs, the number of USMGs applying for positions in nephrology has been steadily decreasing since 2000. There are a number of steps that can be considered to inform and encourage USMGs to consider a career in nephrology.
References
ACGME. Data Resource Book for Academic Year 2013- 2014. Chicago, IL: ACGME, 2014.
American Medical Association Physician Masterfile. Accessed April 15, 2014.
Center for Health Workforce Studies. Trends in Demand for New Physicians, 2003-2009: A Summary of Demand Indicators for 35 Physician Specialties. Rensselaer, NY: University at Albany, State University of New York; 2010.
Center for Health Workforce Studies. 2012 New York Residency Training Outcomes. Rensselaer, NY: University at Albany, State University of New York; 2013.
Collins AJ. ESRD payment policy changes: The new “bundled” dialysis prospective payment system (PPS) in the United States. Available at www.usrds.org/2012/pres/USDialysisBundle_impact_NKFCM2012.pdf. [Accessed 8 July 2014.]
Davis JS, Zuber K. The nephrology interdisciplinary team: An education synergism. Advances in Chronic Kidney Disease 2014 Jul;21(4):338-343.
Davis JS, Zuber K. The role of advanced nurse practitioners in nephrology. Dialysis & Transplantation 2009 Dec;38(12):488-491.
Himmelfarb J, Berns A, Szczech L, Wesson D. Cost, quality, and value: the changing political economy of dialysis care. Journal of the American Society of Nephrology 2007 Jul;18(7):2021-7.
Hines AL, Barrett ML, Jiang HJ, Steiner CA. Conditions With the Largest Number of Adult Hospital Readmissions by Payer, 2011. HCUP Statistical Brief #172. April 2014. Agency for Healthcare Research and Quality, Rockville, MD.
Jhaveri KD, Sparks MA, Shah HH. Novel educational approaches to enhance learning and interest in nephrology. Advances in Chronic Kidney Disease 2013 Jul;20(4):336-46.
[No author.] Renal Physicians Association benchmarking survey shows changes in nephrology practice size, revenue sources. Nephrology News & Issues, 20 Mar 2013.
NRMP. Results and Data: Specialties Matching Service—2014 Appointment Year. Washington, DC: National Resident Matching Program; 2014.
Osinski M. Options in the job market for nephrology fellows. Nephrology News & Issues, 3 December 2013.
Pfuntner A, Wier LM, Stocks C. Most Frequent Conditions in U.S. Hospitals, 2011. HCUP Statistical Brief #162. September 2013. Agency for Healthcare Research and Quality, Rockville, MD.
Shah HH, Jhaveri KD, Sparks MA, Mattana J. Career choice selection and satisfaction among US adult nephrology fellows. Clin J Am Soc Nephrol 2012;7:1513–1520.
US Renal Data System. USRDS 2013 Annual Data Report. National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD.
Appendix: Literature Review
Allocation of Professional Time
The earliest studies of the nephrology workforce focused on how nephrologists spent their professional time and the types of patients they cared for. Two surveys conducted in 1991 (n=1590, 35% response rate) and 1996 (n~400, response rate unclear as a ‘select group of nephrologists’ was surveyed) assessed ASN members’ about allocation of professional effort between nephrology patient care, non-nephrology patient care, administration, and funded research. Key findings included the following:
1991 survey: “50% devoted more than 75% of their effort to patient care, predominately for patients with general nephrology and hypertension problems. Approximately 69% of respondents cared for fewer than 50 hemodialysis patients, and the majority of respondents felt the maximum number of dialysis patients for whom they could provide adequate medical care would be 50. Most respondents felt that there would be a deficiency of nephrologists in their community within 5 years.”
1996 survey: “…Approximately 35% of the respondents’ efforts were found to be devoted to the care of ESRD patients (6). Stated in other terms, the average work week amounted to 57.6 hours on average, yielding approximately 20 hours per week devoted to the care of ESRD patients and 13.5 hours per week caring for non-ESRD patients. Based on 4,500 nephrologists in the United States at the time of the survey and projected growth rates of the ESRD population, it was concluded that a minimum of 202 new trainees per year would be needed through the year 2010 to care for ESRD patients.” (Mitch & McClellan 1998)
Another commentary on the 1996 survey estimated that given the pace of retirements and new entrants to the field, number of full-time clinical nephrologists ’‘[would] be about the same in 2010 as it is today (1997)’. It noted that the growth rate of ESRD had been steady at 9-10%/year, but seemed to be slowing. The mortality rate for dialysis patients in the US was 23-24%/year (vs. rates in ‘teens’ in other countries). The article presents tests of various scenarios of ESRD incidence, FTEs needed for patient care and mortality to predict the number of new trainees needed annually in nephrology programs. Estimates of number of new trainees needed annually range from 202 to 661 depending on assumptions (Neilsen et al. 1997).
Supply and Demand
Since that time, several studies sponsored or otherwise supported by ASN have continued to examine issues of supply and demand in the nephrology workforce. A 2009 commentary/data analysis on nephrology workforce projections and pipeline estimated a shortage of 1000 nephrologists in 2007, given the following facts about the current workforce:
“According to the 2008 AMA report (based on 2006 data), there were 7,410 self-reported nephrologists in the United States, of which 6,761 reported performing patient care, 5,571 were office-based, 730 were fellows, 460 were hospital or university staff, 125 primarily were administrative, 126 reported being involved primarily in medical teaching, and 380 reported themselves as researchers.”
However, the authors suggested that a new workforce analysis is needed due to several factors:
CKD prevalence has increased, but it is unclear how much is due to actual disease and how much due to coding changes.
ESRD patients are also growing older and more medically complex.
New analyses must consider new models of care including generalists, NPs/PAs and multidisciplinary teams in nephrology care.
The authors noted that the overall pipeline/number of medical students has increased, but lack of funding and the cap on Medicare GME positions are major barriers to increasing nephrology training. The number of IM residencies has also been flat, and more IM residents are choosing hospital medicine or other subspecialties (besides nephrology). To address the declining pipeline, the authors recommended updates to nephrology training programs, improved mentoring, and development of nephrology research workforce (e.g. earlier exposure to nephrology, mentorship, flexible tenure clocks—Kohan & Rosenberg 2009).
A 2011 survey of nephrology fellows and qualitative study of blog posts about nephrology by medical residents reinforced these findings, showing that the number of USMGs in training has declined while number of IMGs has increased. The authors noted concerns that the number of IMGs available for nephrology training could continue to decline as J visas become harder to obtain and opportunities increase in IMGs’ home countries. The study’s qualitative findings were similar to other studies: fellows reported limited exposure to nephrology during med school & residency, perception of poor lifestyle and low salaries, complicated & unsatisfying patient care, etc. (Parker et al. 2011). A second study published in Nephrology News & Issues suggested that the current nephrologists delaying retirement and fewer consults from primary care physicians, along with uncertainty about future Medicare funding, were limiting factors to the growth of the nephrology workforce (Osinski 2011).
A 2013 study by members of the ASN Workforce Committee found many of the same issues in its examination of the state of the nephrology workforce. Key findings/comments included the following:
There were 8382 practicing nephrologists in US in 2010 (AMA Masterfile). The number of nephrologists increased 43% between 2000 and 2010.
The number of USMGs choosing nephrology has declined—54.6% of currently practicing nephrologists are USMGs vs. 56.6% in 2007. Nephrology has lower proportions of IMGs than other specialties including cardiology, gastroenterology, endocrinology, & rheumatology.
The number of nephrology fellows has increased from 711 in 2002 to 918 in 2011 (AAMC data). Trainees are more interested in ‘lifestyle specialties’ (not including nephrology), and many of them have higher debt burdens that can influence specialty choice.
Interest in research careers in nephrology has also waned (Parker et al. 2013)
A 2014 commentary on the state of the nephrology workforce (Berns et al. 2014) calls for a ‘new workforce analysis’ that reassesses future supplies of nephrologists needed based on a clarified scope of practice and enhanced training standards. The authors suggest that the workforce may need to be ‘right sized’ in the future, with a possible reduction of training slots to accommodate a leveling off of ESRD prevalence and to ensure that existing slots provide excellent clinical and research training.
Career Choices
In addition to studies of supply and demand, several studies have examined factors affecting career choices of physicians that could influence the future supply of nephrologists. A 2009 survey of ASN members about career choices (n=913, 23% response rate) found that nephrologists were still more likely to be male than in other specialties. It also showed high proportions of IMGs but low proportions of US-trained minority physicians despite high rates of kidney disease among minority communities. Most respondents were very satisfied with their careers. A small proportion received loan forgiveness or repayment, which could contribute to low numbers of academic nephrologists who earn less than nephrologists in clinical practice.
“Interest in nephrology began early in training, with the intellectual aspects of nephrology, early mentoring, and participation in nephrology electives named as the most common reasons in choosing nephrology. Academic nephrologists were more likely to have participated in research in medical school, have a master’s degree or PhD, and successfully obtained research funding during training. Academic debt was higher among nonacademic nephrologists. Research opportunities and intellectual stimulation were the main factors for academic nephrologists when choosing their first post-fellowship positions, whereas geographic location and work-life balance were foremost for nonacademic nephrologists.” (McMahon et al. 2012)
A 2010 survey of exiting nephrology fellows (n=60, 72% US citizens or green card holders) found that respondents listed academia & private practice as top ‘dream jobs’ and were less interested in hospitalist careers. A majority of respondents with jobs were headed to private practice (Torri et al. 2011).
A 2012 commentary on attracting more IM residents to nephrology suggested focusing recruitment efforts through research opportunities and improving mentoring and training. The author suggested that interventional nephrology can be attractive to residents interested in procedure-oriented specialties:
“Among internal medicine (IM) postgraduate year (PGY)-3 residents surveyed when taking the 2002 intraining examination,…residents selecting nephrology fellowships were interested in the ‘opportunity to participate in the care of critically ill patients,’ ‘longterm relationships with patients,’ and higher income (nephrology was viewed as a procedural specialty). Significantly more international medical graduates (IMGs) than US-educated medical graduates were interested in nephrology.”
“Lifestyle questions are included in many surveys, but several factors come under that heading: work hours and their predictability, call and intensity of work during calls, work stress including patient-related stress, and remuneration. We need to identify more clearly whether particular aspects of lifestyle are important to trainees, especially women and IMGs, who would otherwise be drawn to the discipline. We need to identify among our clinical colleagues various practice patterns so that trainees can find one that meets their needs.”
“Economic issues are also factors. Did falling income contribute to dissatisfaction with nephrology in a 2004–2005 survey of practicing physicians? How does this translate to our trainees? …Poor income potential and poor job opportunities after graduation were the two factors listed highest in fellows’ dissatisfaction…[The implication] that hospitalist jobs were somehow subpar for graduating nephrologists…neglects the intricacies of life for many of our trainees. Those international graduates with training visas need positions that fulfill visa waiver requirements. Few pure nephrology jobs meet them, and some, such as with correctional systems, may not appeal to most graduates, including IMGs. Graduates with no visa issues might still have reasons to work as a hospitalist, such as being part of a two-career couple with differing graduation dates, off-cycle training as might occur for maternity leave, or failure to meet nephrology board eligibility requirements necessary for a full-time nephrologist position. Nonetheless, we must understand better the market forces in nephrology positions and work to ensure good jobs for graduating fellows.” (Adams 2012)
A 2012 study of career choices & satisfaction of nephrology fellows (n=204, 22.9% response rate) found that 82% of fellows described nephrology as their first choice specialty. Fewer IMGs than USMGs described nephrology as their first choice specialty. Around 68% of fellows reported that they chose nephrology during residency while 23% chose nephrology during medical school (the remainder chose before medical school or after residency). The majority of nephrology fellows chose nephrology because of their interest in the subject during education/training, excellent mentorship (research interests, job opportunities & income potential were much less influential). Most were at least ‘somewhat satisfied’ with nephrology careers; fellows who didn’t choose nephrology as first choice career are less likely to be satisfied. Reasons for satisfaction included the following:
Excellent teaching and mentoring by faculty during fellowship training (78%)
“Stimulating” variety of cases (75%)
Fellows enjoy intensive care unit nephrology (69%)
Fellows enjoy association of general internal medicine with nephrology (69%)
Reasons for dissatisfaction included the following:
Poor income potential after graduation (70%)
Poor job opportunities after graduation (68%)
Long work hours (55%) (Shah et al. 2012)
A 2013 survey of IM fellows who chose specialties other than nephrology (n=714—11% response rate) found that non-nephrology fellows disliked the following aspects of nephrology:
Dialysis & transplant patients are too complicated
Lack of role model/mentor
Not enough procedures
Difficult subject matter
Perceived lifestyle of practicing nephrologists
Poor monetary benefits
Nephrology is not taught well (Jhaveri et al. 2013a)
Several studies and discussion papers published in nephrology journals have described efforts to increase USMGs’ interest in nephrology careers given ‘mounting concern’ about the ‘mismatch’ between growing numbers of kidney disease patients and falling numbers of USMGs pursuing nephrology training. One study notes that nephrology is the second to last career choice for USMGs (Hoenig et al. 2013). Some have suggested new approaches to nephrology training in medical education intended to attract more USMGs to nephrology—e.g., concept maps, case-based debates, simulations, more emphasis on procedures, and more attention to research training opportunities (Hoenig et al. 2013, Jhaveri et al. 2012, Jhaveri et al. 2013b, Kohan 2008, Kohan et al. 2014, Perazella 2010). Others have described broader efforts to increase interest in nephrology careers among medical students and IM residents including ASN’s Workforce Committee, ASN Kidney Week participation, mentoring programs, improved clinical experiences (Parker et al. 2013).
Diversity
Data about the diversity of the nephrology workforce (except the presence of IMGs) are relatively difficult to obtain, but one study was published in 2011 examining the racial composition of nephrology fellows vs. the population of patients with ESRD, with particular focus on African Americans. Using data sources from ACGME and the USRDS, the authors reported that “a significant disparity continues to exist between the proportional race makeup of African-American nephrology fellows (3.8%) and ESRD patients (32%). The low numbers of African-American nephrology fellows, and consequently new nephrologists, in light of the increase in ESRD patients has important implications for patient-centered nephrology care.” The authors call for increased recruitment of minority physicians into nephrology to foster trust between ESRD patients and providers (Onumah et al. 2011).
Appendix References
Adams ND. Attracting more residents into nephrology. Clinical Journal of the American Society of Nephrology 2012 Sep;7(9):1382-4.
Berns JS, Ellison DH, Linas SL, Rosner MH. Training the next generation’s nephrology workforce. Clinical Journal of the American Society of Nephrology 2014 Sept;9(9):1639- 1644.
Hoenig MP, Shapiro E, Hladik GA. Lessons learned from the ASN Renal Educator Listserv and survey. Clinical Journal of the American Society of Nephrology 2013 Jun;8(6):1054- 60.
Jhaveri KD, Shah HH, Mattana J. Enhancing interest in nephrology careers during medical residency. American Journal of Kidney Diseases 2012 Sep;60(3):350-3.
Jhaveri KD, Sparks MA, Shah HH, Khan S, Chawla A, Desai T, Iglesia E, Ferris M, Parker MG, Kohan DE. Why not nephrology? A survey of US internal medicine subspecialty fellows. American Journal of Kidney Diseases 2013 Apr;61(4):540-6.
Jhaveri KD, Sparks MA, Shah HH. Novel educational approaches to enhance learning and interest in nephrology. Advances in Chronic Kidney Disease 2013 Jul;20(4):336-46.
Kohan DE. Procedures in nephrology fellowships: time for change. Clinical Journal of the American Society of Nephrology 2008 Jul;3(4):931-2.
Kohan DE, Rosenberg ME. The chronic kidney disease epidemic: a challenge for nephrology training programs. Seminars in Nephrology 2009 Sep;29(5):539-47.
Kohan DE, Parker MG, Furth SL, Hudson BG, Warburton KM, Rys-Sikora KE, Rankin TL; Kidney Research National Dialogue. Propagating the nephrology research workforce: a Kidney Research National Dialogue training commentary. Clinical Journal of the American Society of Nephrology 2014 Jun 6;9(6):1144-7
McMahon GM, Thomas L, Tucker JK, Lin J. Factors in career choice among US nephrologists. Clinical Journal of the American Society of Nephrology 2012 Nov;7(11):1786-92.
Mitch W, McClellan WM. Patterns of patient care reported by nephrologists: implications for nephrology training. American Journal of Kidney Diseases 1998 Oct;32(4):551-6.
Neilsen EG, Hull AR, Wish JB, Neylan JF, Sherman D, Suki WN. The Ad Hoc Committee report on estimating the future workforce and training requirements for nephrology. Journal of the American Society of Nephrology 1997 May;8(5):S1-S4.
Onumah C, Kimmel PL, Rosenberg ME. Race disparities in U.S. nephrology fellowship training. Clinical Journal of the American Society of Nephrology 2011 Feb;6(2):390-4.
Osinski M. Staffing: The tide turns in the nephrology job market. Nephrology News & Issues, 27 April 2011.
Osinski M. Options in the job market for nephrology fellows. Nephrology News & Issues, 3 December 2013.
Parker MG, Ibrahim T, Shaffer R, Rosner MH, Molitoris BA. The future nephrology workforce: will there be one? Clinical Journal of the American Society of Nephrology 2011 Jun;6(6):1501-6.
Parker MG, Pivert KA, Ibrahim T, Molitoris BA. Recruiting the next generation of nephrologists. Advances in Chronic Kidney Disease 2013 Jul;20(4):326-35.
Perazella MA. Nephrology fellowship training in the 21st century: where do we stand? Clinical Journal of the American Society of Nephrology 2010 Mar;5(3):387-9.
Shah HH, Jhaveri KD, Sparks MA, Mattana J. Career choice selection and satisfaction among US adult nephrology fellows. Clinical Journal of the American Society of Nephrology 2012 Sep;7(9):1513-20.
Torri D, Sparks M, Calderon K, Shah H, Jhaveri K. Life after renal fellowship: Survey results. ASN Kidney News 2011 Jan;3(1):6.